Abstract
Depressive disorders are common, recurrent, and chronic, and require treatment A review of the symptom picture and current drug targets demonstrates the need for accument of depression severity, including suicidaliltial focus of treatment is rapid resolution of: during an acute phase, followed by continuation. Maintenance treatment is indicated if the risk of recurrence is high. The range of available medications is considerable and the benefit/risk ratio is acceptable. Depression is diagnosable across the life span and treatable at every age (although recent disagreement has arisen with regard to young patients). Comorbidity, both psychiatric and medical, need to be assessed, as does the possible presence of two subtypes of depression (psychotic and bipolar) often requiring different interventions. It is expected that the next generation of antidepressants would be associated with more specific disease and outcome biomarkers.
Los trastornos depresivos se caracterizan por ser comunes, recurrentes, crónicos y requerir tratamiento. Una revisión del cuadro clínico y de los fármacos actualmente disponibles demuestra la necesidad de una acuciosa evaluación de la gravedad de la depresión, incluyendo el riesgo suicida. Ei foco inicial del tratamiento se centra en ia resolución rápida de los síntomas durante la fase aguda, a lo que debe seguir la fase de continuación. El tratamiento de mantención se indicará cuando el riesgo de recurrencia sea alto. La cantidad de medicamentos disponibles es considerable y la relación riesgo/beneficio es aceptable. La depresión se puede diagnosticar a lo largo de toda la vida y tratar en cada edad (aunque recientemente han surgido algunos desacuerdos en relación a los pacientes más jóvenes). También debe ser evaluada la comorbilidad, tanto psiquiátrica como médica, al igual que la posible presencia de dos de los subtipos de depresión (psicótica y bipolar) ya que habitúalmente requieren de intervenciones diferentes. Se espera que la próxima generación de antídepresivos se asocie con enfermedades y con marcadores biológicos de evolución mas específicas.
Les troubles dépressifs sont courants, récurrents, chroniques et nécessitent un traitement, Une revue de la symptomatologie et des cibles médicamenteuses actuelles met en évidence un besoin d'évaluation exacte de la sévérité de la dépression, «suicidalité» incluse. Le but initial du traitement est la résolution rapide des symptômes pendant la phase aiguë, et sa poursuite. Le traitement d'entretien est indiqué si le risque de récidive est élevé. La gamme de médicaments disponibles est très importante et le rapport bénéfice risque est acceptable. La dépression peut être diagnostiquée tout au long de la vie et traitée quel que soit l'âge (malgré des désaccords récents concernant les patients jeunes). La comorbidité, à la fois psychiatrique et médicale, doit être évaluée comme doit l'être la présence éventuelle de deux sous-types de dépression (psychotique et bipolaire) pour lesquels les besoins thérapeutiques sont souvent différents. On espère que la nouvelle génération d'antidépresseurs s'adressera à des troubles plus spécifiques et comportera des biomarqueurs de résultats.
Depressive disorders are common, recurrent, chronic, and require treatment. Major depressive disorder can occur across the entire life cycle and Is the most common of the severe psychiatric Illnesses. In the USA, the lifetime prevalence was 16.2% (32.6-35.1 million adults) and the 12-month prevalence was 6.6% (13.1-14.2 million adults) In a recent survey.Citation1 According to the World Health Organization's Global Burden of Disease Report,Citation2 major depression was the fourth leading cause of disease burden worldwide In 1990. The World Health Organization predicts that by 2020, major depression will become the second leading cause of worldwide disease burden, surpassed only by Ischemic heart disease. In this review, we will focus on major depressive disorder, although we will also briefly discuss bipolar depression.
Symptom picture syndrome
The cardinal feature of major depression Is persistent depressed mood or pervasive loss of Interest or pleasure for a minimum of 2 weeks, accompanied by a series of somatic and cognitive changes (Table I). In assessing the core components of depression, it is important to note that the psychological and biological symptoms are accompanied by negative thought content, cognitive dysfunction, and suicidal ideation. These components follow the American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) nosology for mood disorders, but recently there has been considerable interest in assessing not only current symptoms, but also “softer” or spectrum features, which may present lifetime signs of particular mood or mood-related spectra.Citation3,Citation4 In fact, such persistent features may relate to levels of functional impairment during episodes of depression more directly than current symptoms. Such assessment strategies raise the need for assessment of dimensional approaches to diagnosis, as well as the measurement of traditional categorical distinctions.Citation5 Women are at twice the risk of men. Depression can and often does co-occur with another psychiatric condition or with a medical disease. Depression is a life-threatening illness for both men and women since suicide is estimated to be the cause of death in up to 6% of individuals with clinical depression. Citation6
Table I. Core components of major depression.
Pathogenesis and drug targets
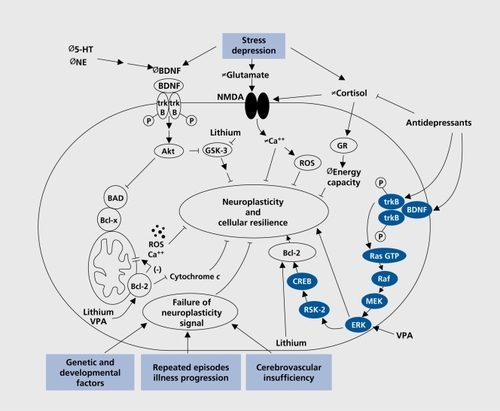
It has been assumed that the neurobiological systems involved in the pathogenesis of depression are primarily the monoaminergic neurotransmitter systems. Considerable research has been directed toward uncovering specific defects in serotonin (5-hydroxytryptamine [5-HT]), norepinephrine (NE), and to a lesser extent dopamine (DA) neurotransmitter systems. The blockade of neurotransmitter receptors or transporters by antidepressant drugs occurs at the level of the neuronal synapse. This capacity to produce acute increases in synaptic levels of monoamines (Table II)Citation7 has been long considered responsible for both therapeutic and adverse effects of antidepressants. However, recent advances in the neuroscience of mood regulation have pointed to the involvement of additional neurotransmitter systems and to the influence of several neuroendocrine axes; however, these discoveries have not yet led to approved treatments for depression, nor have they fundamentally changed our basic understanding of depression. Further developments in the drug treatment of depression are being actively pursued. Medications currently under testing programs include dual reuptake inhibitors, novel dopamine reuptake inhibitors, drugs combining 5-HT reuptake inhibition with 5-HT2/5-HT3 receptor antagonism, corticotropin-releasing factor (CRF) receptor antagonists, substance P (neurokinin) receptor antagonists, melatonergic agonists, and compounds modulating glutamatergic neurotransmission. Other novel treatment strategies are also in the pipeline.Citation8 Most recently, attention has moved from intrasynaptic changes in neurotransmitter levels to changes in intracellular signaling pathways.Citation9 In an important review, Manji and colleaguesCitation9 raise the possibility that depression may be associated with impairments in signaling pathways that are considered important for the regulation of neuroplasm ticity and cell survival. The heuristic value of such an approach, as highlighted in (), points to the wide-ranging possibilities of understanding the mechanisms of action of currently available medications, but raise the possibilities of new targets for future drug development. Furthermore, the review proposes roles for chronic stress. In turn, McEwen's concept of “allostatic load” may be incorporated into how recurrent depression leads to structural and functional central nervous system (CNS) impairment.Citation10
Table II. Antidepressant potency for blocking norepinephrine (NE), serotonin (5-hydroxytryptamine [5-HT]), and dopamine (DA) transporters. + to +++++, increasing levels of potency; -, weak; 0, no effect. Adapted from reference 7: Richelson E. The clinical relevance of antidepressant interaction with neurotransmitter transporters and receptors. Psychopharmacol Bull. 2002;36:133-149. Copyright © 2002. Medworks Media LLC.
Assessment
In assessing depression, clinicians should consider the level of symptom severity and current functional impairment of the patient, the duration of the depression, the presence of psychotic symptoms, level of suicidality, and previous ill-ness and treatment history. Most depressed patients do not self-refer directly to a psychiatrist. Instead, they seek help from a primary care physician, often focusing on somatic disorders or energy rather than mood complaints. Recognition (sometimes more difficult in men) and appropriate diagnosis should be followed immediately by a treatment plan. If the plan includes medication, it must involve the choice of an appropriate drug prescribed at an adequate dosage and for a sufficient duration, with attention to treatment adherence by patient and family members or caretakers, if necessary.Citation11 Recognition and treatment of depression in the context of an ongoing medical disease, such as diabetes or hypertension, is very important. The primary care physician is generally in an excellent position to do so if he or she is responsible for the overall medical care of the patient. Consultation and referral to a psychiatrist is appropriate in selected cases if the primary care physician is concerned about the complexity of the case. The treating physician needs to evaluate the complexity of the symptom picture (eg, delusions, mixed manic and depressive symptoms) and dangerousness with respect to suicide or homicide at each visit. He or she should seek consultation in difficult-to-treat cases. Several forms of brief depression-specific psychotherapy, including cognitive therapyCitation12 and interpersonal psychotherapy,Citation13,Citation14 have been shown to have efficacy equal to that of antidepressant medication and should be considered as treatment options or adjuncts. However, a review of these treatment strategies is beyond the scope of this review.
Assessment of suicidality
Probably half of patients with major depressive episodes report death wishes, feeling that they have no reason to live, thinking they would be better off dead, thoughts of harming or killing themselves, or actual plans to do so. Suicidal risk should be assessed not only at the initiation of treatment, but repeatedly throughout treatment. Some patients will not report suicidal ideation until they feel comfortable with the clinician, often several weeks into treatment. It is essential to ask if patients have thoughts or plans to harm themselves, whether they have a history of suicide attempts (and, if so, to determine the medical seriousness of prior attempts), and whether they have access to means. This includes specific questions about access to firearms, since half of all suicides in the USA involve hand-guns.Citation15 If a patient acknowledges a plan or intent to harm him/herself, then emergency psychiatric evaluation is indicated. Up to 75% of patients who complete suicideCitation15 have seen a primary care physician within the month prior to death, meaning that the physician has a unique opportunity to prevent suicide through appropriate intervention. Depressed patients with suicidal ideation often take longer to respond to treatment, thus necessitating a longer period of vigilance on the clinician's part.Citation16 Due diligence includes both frequent assessments of suicidal ideation and hope- lessness, aggressive treatment of the depression, and creation of a safety net involving other members of the health care team and family members or caregivers. In the USA and UK over the past 18 months, considerable furor has raged about the risk that the use of one class of antidepressants, selective serotonin reuptake inhibitors (SSRIs) may actually raise the likelihood of suicidal ideation and suicidal acts, rather than reducing the likelihood. Examination of adverse event reports for SSRIs in children and adolescents has led to “black box warnings” in the package inserts for SSRIs in the USA and considerable “official” caution in the UK about prescribing such drugs for individuals under the age of 18. These policy decisions have illustrated the need for better methodical approaches for risk assessment (see below).
Phases of treatment
In developing a treatment strategy, it is useful for the clinician to consider treatment of major depression as involving three phases: acute, continuation, and maintenance (if appropriate). The goals of the acute phase are to achieve remission (resolution of all symptoms) and restore functioning (Table III).Citation17,Citation18 During this period, continued follow-up visits are essential The goal of the continuation phase is sustained remission. Unfortunately, only recently has renewed attention been devoted to the issue of response versus remission. Failure to achieve complete remission (recovery) has major adverse consequences including the following: increased risk of relapseCitation19 and treatment resistance; persistent functional impairmentCitation20; sustained risk of suicide; worsened morbidity of other psychiatric conditions; and medical disorders. This phase should last approximately 6 months following full remission of the acute episode. Then, the patient in whom the risk for recurrence is low should be gradually tapered from treatment over a period of 1 to 3 months. Rapid discontinuation of virtually all antidepressants, including those with long half-lives, tends to be associated with symptomatic relapse. Since the majority of depressed individuals suffer from recurrent depression, the physician should consider the appropriateness of a maintenance phase. Data on long-term treatment in the psychiatric specialty sector indicate that maintenance treatment should be sustained for a minimum of 3 to 5 years. Unfortunately, there are no suchCitation21-Citation23 studies in primary care to determine appropriate duration of long-term treatment in this setting.
Table III. Depression medication algorithms. Contact may be in person or by telephone. Reproduced from Rush AJ et al (The Texas Medication Algorithm Project), personal communication.
Available medications and their use in acute treatment
There is no paucity of medications approved by the Food and Drug Administration (FDA) for a depression indication. One of the two initial classes was the tricyclic anti-depressants (TCAs), a family of structurally related compounds with reuptake inhibitory properties on brain monoamine metabolism. All the TCAs are potent blockers of NE reuptake (except for clomipramine which highly serotonergic, but is approved by the FDA only for treatment of obsessive-compulsive disorder) and weak blockers of 5-HT reuptake. The second original class of drugs, the monoamine oxidase inhibitors (MAOIs), have never been widely prescribed because of real (and sometimes exaggerated) concerns about safety, despite their established efficacy in certain subtypes, especially atypical and bipolar depression.Citation24,Citation25
A majority of the newer compounds are considered to be SSRIs. Despite a number of meta-analyses of efficacy showing no differences between TCAs and SSRIs in ambulatory studies, the more favorable adverse effect profile (including a virtual absence of overdosage lethality), ease of administration, and acceptance by physicians across specialties have led to the emergence of the SSRI as first-line treatments.Citation26,Citation27 Patients can be started on the initial dose as indicated in Table IV and gradually increased over a 10-to 14-day period to the modal therapeutic dose. If the patient has not responded to this dose by 3 to 4 weeks, one should consider increasing the dose again. When the first drug in this class is not effective, experienced clinicians will often either try to augment the response with another medication or switch to another SSRI.
Table IV. Currently available antidepressants and their recommended dosages. SSRI, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressant; MAO I, monoamine oxidase inhibitor. *A generic formulation is available. †Approved by the Food and Drug Administration (FDA) for treatment of obsessive-compulsive disorder, but not depression. ‡The higher dosage is approved in some countries but not in the USA. §A maximum therapeutic dose has not yet been established for this compound. Even higher doses might be indicated if plasma drug concentrations are low (ie, <50 ng/mL). The maximum FDA-approved dosage of the extended-release formulation is 225 mg/day.
In Table IV, the starting, modal therapeutic, and maximum recommended doses are listed for the approved drugs by class. Other currently approved antidepressants are available in the USA include venlaf axine, mirtazapine, bupropion, trazodone, and nef azodone. While trazodone is often used as an adjunctive medication for sleep problems associated with depression itself or with the use of the more alerting SSRIs, of these four drugs, only venlafaxine (with presumed dual neuronal reuptake inhibition) has emerged as comparable in overall use to the SSRIs. In fact, several meta-analyses have pointed to increased efficacy when compared with fluoxetine, but not necessarily with other SSRIs (C. Nemeroff, personal communication).Citation28,Citation29
The antidepressant market remains a highly competitive one, with a number of pharmaceutical companies introducing compounds that they hope will prove to have faster onset of action, produce a more complete remission, and reduce side-effect burden, especially weight gain and sexual dysfunction. Escitalopram (the slngle-Isomer form of cltalopram) recently received FDA approval and duloxetlne (an SNRI [serotonin and noradrenaline uptake inhibitor] with dual reuptake inhibition of 5-HT and NE) has also been approved. It is also important to point out that several antidepressant drugs approved in Europe and Canada (eg, tianeptine, reboxetine, milnacipran, and moclobemlde) are not approved for use In the USA.
Therapeutic Interest In psychostimulants has led to studies suggesting that methylphenldate Is generally well tolerated and modestly efficacious for medically burdened depressed elders, but should only be used in the short term.Citation30 It Is also appropriate to comment on the current status of herbal remedies for depression that currently fall outside the FDA guidelines. Although there are a number of reports pointing to the efficacy of Hypericum perforatum (Saint John's wort) for major depression,Citation31,Citation32 two US trials comparing Hypericum with an SSRI and placebo have not supported this claim.Citation33,Citation35
While adverse effects are reported with all antidepressant compounds, most are transient and no major adverse effects have been reported after long-term use. In general, the TCAs are distinguished by anticholinergic and antihlstamlc effects (Table V).Citation36 Citation41 Drug Interaction with TCAs and other medications affecting the hepatic enzyme (CYP 2D6) can lead to significantly altered TCA plasma levels. MAOIs are used sparingly, partly because of concern with hypertensive crises, as well as their interaction with other prescribed medications and beer, red wine, and foodstuffs rich in the amino acid tyramine, such as aged cheese and liver. Clinical experiences in the last 15 years have shown that the SSRIs are relatively safe, but their adverse effect profile may not be the same across the entire class. While the efficacy and adverse effect profile should be considered in selecting among the SSRIs, in usual practice these drugs do not differ dramatically in efficacy from each other or from the older classes of antidepressants. The adverse effects that most frequently influence patients' decisions to discontinue treatment are sexual dysfunction and weight gain. In inpatient settings, TCAs are still often used as first-line treatment. Not all SSRI (eg, citalopram and sertraline) have a high degree of drug-drug interaction via the cytochrome P450 (CYP) system. While nausea, sedation, appetite change, and sexual dysfunction seem approximately similar for the SSRI class, claims for reduced adverse effects on sexual functioning have been made for fluvoxamine (only approved by the FDA for obsessive-compulsive disorder),Citation42 as have claims for reduced discontinuation effects for fluoxetine.Citation43 Finally, the high degree of comorbidity of depression and cigarette consumption needs to be fully understood. Tobacco smoking can induce CYP enzyme changes affecting blood levels of various antidepressants, as well as complicate drug management when smoking cessation occurs.Citation44
Table V Adverse effects of antidepressants.Citation36-Citation41 SSRl, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressant; NSRI, noradrenaline and serotonin reuptake inhibitor; MAOI, monoamine oxidase inhibitor; AMX, amoxapine; DOX, doxepine; IMI, imipramine; PRO, protriptyline; AMI, amitriptyline; EC IT, escitalopram; MRZ, mirtazapine; SER, sertraline; CIT, citalopram; FLVX, fluvoxamine; NOR, nortriptyline; TRY, tranylcypromine; CLO, clomipramine; FLX, fluoxetine; PAX, paroxetine; VEN, venlafaxine; DES, desipramine; CNS, central nervous system; Gl, gastrointestinal; ECG, electrocardiogram; CAD, coronary artery disease; Ml, myocardial infarction.
Depression across the life span
While some aspects of the symptom picture may change across the life span, the core features of depression are recognizable. In children and adolescents, depression is not always characterized by sadness, but instead by irritability, boredom, or an inability to experience pleasure. Depression is present in about 1% of children and 5% of adolescents at any given time.Citation45 Before puberty, boys and girls are at equal risk for depression, whereas after the onset of puberty, the rate of depression is about twice as high in girls. While prepubertal depression is less prevalent than postpubertal depression, appropriate management at any age for major depression is recommended. At the other end of the life span, depressed older adults will usually be seen at medical facilities. Major depression affects 5% to 10% of older adults who visit a primary care providerCitation46-Citation48 and has negative implications for the prognosis of almost all co-occurring medical illnesses with which such patients may present.
Treatment of child and adolescent depression
Drug treatment for children or adolescents with depression is primarily dependent on SSRIs as first-line acute treatment. Efficacy trials have been conducted with fluoxetine, paroxetine, and citalopram.Citation49-Citation51 The recommended practice is to start at half the usual dose of an SSRI (eg, 10 mg/day fluoxetine, paroxetine, or citalopram) for 1 week for adjustment purposes and then increase the dose to the equivalent of 20 mg/day fluoxetine for another 3 weeks.Citation45 It takes up to 4 weeks at steady state to determine whether a given dose will be helpful Thus, further increases should be made at 4-week intervals. Because children and adolescents metabolize SSRI more rapidly than adults, they often require doses above the equivalent of 20 mg fluoxetine to attain a clinical response.Citation52 The large National Institute of Mental Health (NIMH) multicenter contract, Treatment for Adolescents With Depression Study (TADS),Citation53 for the treatment of depression in adolescents has been recently completed, and perhaps will provide more definitive data for this population.
In a sample of 439 adolescents (aged 12 to 17 years) with major depression, four randomly assigned interventions were utilized: fluoxetine (10 to 40 mg/day) with cognitive behavioral therapy (CBT); fluoxetine alone; CBT alone; and placebo. As noted in Table VI, 71% responded to the combined treatment, with 60.6% to fluoxetine alone, 43.2% to CBT alone, and 34.8% to placebo. A clinically useful manner to review these findings is to calculate number needed to treat (NNT; calculated as 1/risk difference). NNT represents the number of subjects who would have to be treated with active treatment to obtain one success that would not be obtained with the control treatment. Referring to Table VI, NNT for the combination treatment is 3, fluoxetine alone 4, and CBT alone 12, suggesting a medium effect size for the combination treatment and for fluoxetine alone. In addition, clinically significant suicidal thinking present in 29% of the sample at baseline improved significantly. Seven (1.6%) of 439 patients attempted suicide, but there were no completed suicides.
Table VI. Treatment for Adolescents with Depression Study (TADS) randomized controlled trial.Citation53 NNT, number needed to treat; CBT, cognitive behavioral therapy.
Treatment of geriatric depression
In a similar fashion, SSRIs have now largely replaced TCAs and MAOIs as first-line acute treatments for latelife depression.Citation54 SSRIs are administered in older patients with initial dosing at half the usual effective dose and doubled after 1 week. A recent review has concluded that SSRIs are efficacious, safe, and well tolerated in older patients with depression without comorbidity, as well as in those with medical comorbidity,Citation55 including dementia,Citation56-Citation60 cardiovascular disease,Citation61 cerebrovascular disease,Citation62 stroke,Citation63,Citation64 and other medical conditions.Citation65-Citation69
Although most data are supportive of SSRIs as a class in the treatment of geriatric depression, experts favor the use of citalopram or sertraline over fluvoxamine and fluoxetineCitation54-Citation70 because of their favorable pharmacokinetic profiles, a lower potential for clinically significant drug-drug interaction, and data suggesting their superiority in terms of cognitive improvement.Citation57,Citation58,Citation71,Citation72 One placebo-controlled study with sertraline in elderly outpatients with major depression treated in both psychiatric and primary care settings further supports use of SSRIs in geriatric depression.Citation73 In the “old-old” population (>75
years old) with depression, active medication (citalopram) was no more effective than placebo, except for patients with high levels of baseline severity.Citation74 Among the TCAs, where cardiac monitoring is recommended, nortriptyline is the most frequently used agent in the elderly, probably because it is considered the least cardiotoxic drug in this class and blood levels can be monitored. Adverse drug reactions increase dramatically in frequency and severity with advanced age.Citation75 Factors that may influence proper dosing include the different pharmacokinetic properties of antidepressants in elderly compared with younger patients and individual patient characteristics, such as cardiovascular or renal function. In elderly patients, antidepressant side effects of particular concern include orthostatic hypotension and anticholinergic effects (more common with TCAs), as well as extrapyramidal symptoms, and the syndrome of inappropriate antidiuretic hormone secretion.
Course of treatment
While it used to be assumed that the typical major depression was self-limiting (of 3 to 6 months duration) and associated with complete recovery, the present view is not as sanguine. Clinical trials have demonstrated that 30% to 40% of depressed patients fail to respond to firstline antidepressant treatment despite adequate adherence, dose, and duration,Citation76,Citation77 60% to 70% fail to achieve a complete remission of symptoms,Citation78 up to 20% have not recovered 2 years after initiation of treatment,Citation79,Citation80 and 10% remain depressed despite multiple interventions.Citation76,Citation81
Many patients suffer from recurrent depression that requires long-term maintenance treatment to prevent future episodes of depression. Some depressive conditions, including psychotic depression, bipolar depression, and depression with psychiatric or medical comorbidity, have been associated with poor outcome and/or a higher degree of resistance to specific types of treatment or to treatment in general.Citation82
Successful treatment of major depression may require more than one drug trial. A full discussion of the tactics involved in selection of the second treatment (same class, different class), choice of whether to augment the first drug with a second compound or with psychotherapy or to change treatment completely is beyond the scope of this review. Clinicians who wish to treat rather than refer these or complex patients can consult the treatment algorithms derived from the Texas Medical Algorithm Project (TMAP).Citation18 The goal of treatment is full remission of symptoms, but less than 50% of patients achieve this goal within 8 to 12 weeks. In general, if a patient has not shown marked improvement within 8 weeks, psychiatric consultation is recommended. Clearer guidelines for treatment augmentation and switching should be derived from the ongoing multisite NIMH contract, Sequenced Treatment Alternative to Relieve Depression (STARED).Citation83 This large multicenter trial (ultimately enrolling more than 4000 patients nationwide) is prospectively evaluating alternative antidepressants and augmentation strategies for patients at three stages of treatment resistance.
Psychotic depression
Psychotic depression, representing over 15% of more severely depressed cases,Citation84 is characterized by the presence of either delusions or hallucinations, which are often but not always congruent with the depressive themes. Psychotic depression has less than one half the likelihood of responding to antidepressant monotherapy compared with a nonpsychotic depressive disorder.Citation85-Citation88
Initially, TCAs, especially in the higher dose range, were used. Subsequent investigations indicated that TCAs combined with typical antipsychotics provided greater levels of efficacy (eg, amitriptyline and perphenazine).Citation88 Although SSRIs alone have not been used routinely to treat psychotic depression, the use of an SSRI and an atypical antipsychotic has shown efficacy greater than an SSRI alone.Citation89 C-f 073 (mifepristone), a selective glucocorticoid receptor II (GRII) antagonist (not currently on the US market), has shown some promise in the acute treatment phase of psychotic depression.Citation90 In urgent situations or when other treatments have failed, electroconvulsive treatment (ECT) is warranted. While ECT is efficacious (for psychotic depression), it has many drawbacks including the requirement that the treatment must be administered under anesthesia in a hospital setting or a similarly equipped ambulatory setting.Citation91
Bipolar depression
Bipolar depression (major depression in patients also experiencing periods of mania or hypomania) represents a major challenge to clinicians, since response to treatment is often poor and the process of achieving complete remission without a switch into mania is challenging. Generally, patients are already being treated with mood stabilizers. A number of investigators have pointed to the relatively poor response to traditional TCAs in this population.Citation92-Citation94 Most SSRIs demonstrate only moderate success. Recently, efforts to combine an SSRI with an atypical antipsychoticCitation95 have shown promising results in bipolar depression.Citation96 A number of atypical antipsychotic drugs are also showing some degree of antidepressant effect, perhaps similar to that of lithium.
The usual strategy is to use mood stabilizer monotherapy as the first-line therapy for bipolar depression, with the addition of an antidepressant reserved for depressed patients who do not benefit from mood stabilizer monotherapy. One hierarchy of mood stabilizer options is: (i) lithium carbonate; (ii) divalproex; (iii) olanzapine (now FDA-approved for mania and maintenance in bipolar disorder); and (iv) lamotrigine (FDA-approved for maintenance in bipolar disorder).Citation95,Citation97,Citation98 The particular medication is chosen on the basis of the patient's history; patients known to not have responded to one monotherapy should be advanced to the next strategy A minimum adequate trial is 4 weeks of mood stabilizer monotherapy at an optimal dose/blood level.
In contrast to the treatment of mania, pharmacological treatment of bipolar depression remains vastly understudied. Although two important placebo-controlled trials were concluded recently,Citation99,Citation100 they are the first two adequately powered studies ever conducted on this condition. Despite the severity of pediatric bipolar depression, empirical data on its treatment are limited, largely because of the relatively low prevalence of pediatric bipolar disorder. The SSRIs are the only class of medications with some level of proven efficacy in pediatric unipolar depression.Citation49,Citation101,Citation102 Practitioners are compelled to treat depressed bipolar children and adolescents using the SSRI because the illness is so severe; however, the SSRI sometimes worsen the cyclicity of the disorder. We also lack any controlled treatment studies of bipolar depression in later life.Citation103
Comorbidity
Comorbidity or “co-occurrence” of either other psychiatric disorders or medical disorders is very common in major depression. Indeed, it is so common that the frequent questions raised include the heterogeneity of the depressive disorder, subgroups with specific comorbidities, and whether such nosological differences have treatment and/or pathophysiological implications.Citation5 For example, bipolar depression is associated often with panic-anxiety features, substance use, and cardiovascular disease, all of which have effects on immediate and long-term prognostic indicators.
Comorbidity of substance and alcohol abuse with depression is generally associated with a worse prognosis.Citation104 Several symptoms of alcohol and substance abuse, such as sleep disturbance, irritability, and dysphoria, contribute to this outcome. In fact, even moderate use of psychoactive substances such as alcohol can have a negative effect on the outcome of treatment for major depression and should be discouraged until the depression is fully remitted.Citation105 The frequent association of substance abuse with other comorbid disorders (eg, antisocial personality or anxiety disorders) may further complicate the prognosis.Citation106
Medical co-occurrence represents another major factor contributing to poor treatment response. Diseases like hypothyroidism, stroke, diabetes, coronary artery disease, Parkinson's disease, human immunodeficiency viral infection and acquired immunodeficiency syndrome, cancer, and chronic pain syndrome can play a major role in reducing treatment responsiveness, especially when the medical illness is irreversible.Citation107 Even when a reversible underlying medical condition is contributing to depression, treatment of that condition alone is not always sufficient to resolve the depression. Furthermore, some of the medications used to treat comorbid medical conditions may induce or worsen a depressive episode. Depression is a risk factor for mortality after acute myocardial infarction (MI) and a morbidity risk factor associated with slow recovery from an MI and poorer quality of life.Citation108-Citation111 Recent trials with SSRIs are pointing to these medications as safe and effective treatment for recurrent depression with recent MI or unstable angina, although a beneficial effect on the underlying cardiac disease has not been found consistently in studies to date.Citation112,Citation113 It is likely that similar findings will emerge from intervention studies in depression and other concurrent serious medical conditions.
Continuation/maintenance treatment
Clinical guidelines generally recommend that treatment should be continued for at least 6 months following remission of acute symptoms.Citation114,Citation115 However, because of the recurrent nature of depressive disorder, a question is how long patients at risk of recurrence should remain on antidepressant medication. A recent review of data from longer-term studiesCitation116 pooling 31 randomized trials, demonstrated that continuing treatment reduced the odds of relapse by 70% (95% confidence interval [CI] 62% to 78%) compared to treatment discontinuation. The average rate of relapse or recurrence on placebo was 41% compared with 18% on active treatment. Most of the trials were of only 12 monthsCitation5 duration. Thus, the evidence on longer-term treatment requires confirmation; however, in the longer trials evaluated, the treatment effect appeared to persist for up to 36 months.
This new analysis reinforces the available findings from long-term maintenance trials conducted with TCA. The Prien et alCitation21 and Frank et alCitation22 maintenance studies with imipramine in mid-life adults, followed by the Reynolds et alCitation23 study in late-life depression with nortriptyline, established the efficacy of long-term maintenance treatment with antidepressants, specifically in recurrent major depression. Subsequent studies with SSRIs have pointed to similar levels of efficacy with fluoxetine, sertraline, and citalopram in mid-life patients and with citalopram in late-life patients, most of whom had experienced at least one prior episode of depression.Citation117-Citation120 Furthermore, studies on long-term treatment of chronic depression (major depression with an episode lasting greater than 2 years) with the TCAs, desipramine and imipramine, and the SSRI, sertraline, have demonstrated efficacy in chronic depression.Citation121,Citation122
While this report is not focused on psychotherapy for treatment of depression, it is noteworthy that the combination of antidepressants and specific targeted psychotherapy (interpersonal psychotherapy) has been conducted successfully in long-term trials with some suggestion in the elderly that combination treatment was better than antidepressants alone.Citation22,Citation23
Future directions and conclusions
As discussed earlier in this review on the section on pathogenesis and drug targets, considerable efforts are being directed toward the development of new strategies for drug discovery in depression. These strategies include, as highlighted by Nestler et alCitation123 “developing better animal models of mood disorders; identifying genetic determinants of normal and abnormal mood in humans and animals; discovering novel targets and biomarkers of mood disorders and treatments.“
Biomarkers for depression have traditionally been divided into four groupsCitation8: peripheral, CNS neurochemical, CNS functional, and genetic biomarkers. Recent advances in functional and positron emission tomography (PET) neuroimaging, as well as pharmacogenetics, have overshadowed the previous primacy of peripheral markers. The advantages of these new methodologies are numerous, such as more direct CNS determinations, the ability to combine modalities such as cognitive neuroscience paradigms and functional magnetic resonance imaging (fMRI), and repeatability of measures over extended periods of time. However, the current limitations including ligand development, better pharmacogenetic tactics, and appropriate recruitment of large sample sizes may limit the extent of the immediate payoff for such strategies.
One final concern in the overall positive picture for advances in therapeutics for depression has been our failure to utilize the best available methodological tools to design and interpret clinical trials in depression. Insufficient planning for sample size, target population, appropriate outcome measures, multisite “assessment,” and direct tactical planning for placebo effects have been associated on total focus on statistical significance, with less focus on clinical significance. Our failure to articulate clinical significance and effect size, as specified with the use of effect size determinations, is partially responsible for our weak clinical trial design strategies. Risk assessment for clinical trials to utilize tactics such as NNT for benefit (efficacy) and NNH (number needed to harm) for adverse events (risk) ratio should be conducted in all clinical trials and should be reported routinely. More attention should be given to moderator mediator analyses to identify important therapeutically responsive subgroups.Citation124 In summary, all the contemporary biostatistical methodological tools should be aligned with the neuroscience and genetic toolbox to increase the likelihood that newer treatments for depression will be developed in the near future.
Selected abbreviations and acronyms
| CBT | = | cognitive behavioral therapy |
| DA | = | dopamine |
| 5-HT | = | 5-hydroxytryptamine (serotonin) |
| MAOI | = | monoamine oxidase inhibitor |
| NE | = | norepinephrine |
| NNT | = | number needed to treat |
| SNRI | = | serotinin and noradrenalie uptake inhibitor |
| SSRI | = | selective serotonin reuptake inhibitor |
| TCA | = | tricyclic antidepressant |
Support for this work was provided in part by the National Institute of Mental Health grant MH30915. Also, the author wishes to gratefully acknowledge the expert advice of Drs Ellen Frank, Michael Thase, Bruce Pollock, and Charles Reynolds 111 of the Department of Psychiatry, University of Pittsburgh Medical Center.
REFERENCES
- KesslerRC.BerglundP.DemlerO.et al.The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R).JAMA.20032893095310512813115
- MurrayCJL.LopezAD.The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability from Diseases, Injuries, and Risk Factors in 1990 and Projected to 2020. Cambridge, Mass: Harvard School of Public Health on behalf of the World Health Organization and the World Bank, Harvard University Press;1996
- CassanoGB.RucciP.FrankE.et al.The mood spectrum in unipolar and bipolar disorder: arguments for a unitary approach.Am J Psychiatry.20041611264126915229060
- FrankE.CyranowskiJM.RucciP.et al.Clinical significance of lifetime panic spectrum symptoms in the treatment of patients with bipolar l disorder.Arch Gen Psychiatry.20025990591112365877
- KupferDJ.FirstMB.RegierDA.edsA Research Agenda for DSM-V. Washington, DC: American Psychiatric Association;2002
- InskipHM.HarrisEC.BarracloughB.Lifetime risk of suicide for affective disorder, alcoholism and schizophrenia.Br J Psychiatry.199817235379534829
- RichelsonE.The clinical relevance of antidepressant interactions with neurotransmitter transporters and receptors.Psychopharmacol Bull.20023613314912858153
- TammingaCA.NemeroffCB.BlakelyRD.et al.Developing novel treatments for mood disorders: accelerating discovery.Biol Psychiatry.20025258960912361670
- ManjiHK.DrevetsWC.CharneyDS.The cellular neurobiology of depression.Nat Med.2001754154711329053
- McEwenB.Mood disorders and allostatic load.Biol Psychiatry.20035420020712893096
- WhooleyMA.SimonGE.Managing depression in medical outpatients.N Engl J Med.20003431942195011136266
- BeckA.RushA.ShawB.EmeryG.Cognitive Therapy of Depression. New York, NY: Guilford Press;1979
- KlermanMM.WeissmanBJ.RounsavilleBJ.ChevronES.edsInterpersonal Psychotherapy of Depression. New York, NY: Basic Books;1984
- WeissmanMM.MarkowitzJC.KlermanGL.edsComprehensive Guide to Interpersonal Psychotherapy. New York, NY: Basic Books;2000
- GoldsmithSK.PellmarTC.KleinmanAM.BunneyWE.edsInstitute of Medicine, National Academy of Sciences: Reducing Suicide, a National Imperative. Washington, DC: The National Academies Press;2002
- SzantoK.MulsantBH.HouckP.DewMA.ReynoldsCF.Occurrence and course of suicidally during short-term treatment of late-life depression.Arch Gen Psychiatry.20036061061712796224
- LinEH.KatonWJ.VonKorffM.et al.Relapse of depression in primary care: rate and clinical predictors.Arch Fam Med.199874434499755737
- RushAJ.CrismonML.KashnerTM.et al.Texas Medication Algorithm Project, Phase 3 (TMAP-3): rationale and study design.J Clin Psychiatry.20036435736912716235
- JuddLL.AkiskalHS.MaserJD.et al.Major depressive disorder: a prospective study of residual subthreshold depressive symptoms as predictor of rapidrelapse. J Affect Disord.19985097108
- SimonGE.RevickiD.HeiligensteinJ.et al.Recovery from depression, work productivity, and health care costs among primary care patients.Gen Hosp Psychiatry.20002215316210880708
- PrïenRF.KupferDJ.ManskyPA.et al.Drug therapy in the prevention of recurrences in unipolar and bipolar affective disorders: a report of the NIMH Collaborative Study Group comparing lithium carbonate, imipramine, and a lithium carbonate-imipramine combination.Arch Gen Psychiatry.198441109611046437366
- FrankE.KupferDJ.PerelJM.et al.Three-year outcomes for maintenance therapies in recurrent depression.Arch Gen Psychiatry.199047109310992244793
- ReynoldsCF.FrankE.PerelJM.et al.Nortriptyline and interpersonal psychotherapy as maintenance therapies for recurrent major depression: a randomized controlled trial in patients older than 59 years.JAMA199928139459892449
- QuitkinFM.StewartJW.McGrathPJ.et al.Columbia atypical depression: a subgroup of dépressives with better response to MAOI than to tricyclic antidepressants or placebo.Br J Psychiatry.19931633034
- ThaseME.TrivediMH.RushAJ.MAOI in the contemporary treatment of depression.Neuropsychopharmacology.1995121852197612154
- WilliamsJW Jr.MulrowCD.ChiquetteE.HitchcockP.AguilarC.CornellJ.A systematic review of newer pharmacotherapies for depression in adults: evidence report summary.Ann Intern Med.200013274375610787370
- MacGillïvrayS.ArrollB.HatcherS.et al.Efficacy and tolerability of selective serotonin reuptake inhibitors compared with tricyclic antidepressants in depression treated in primary care: systematic review and meta-analysis.BMJ.20033261014101912742924
- ThaseME.EntsuahAR.RudolphRL.Remission rates during treatment with venlafaxine or selective serotonin reuptake inhibitors.Br J Psychiatry.20017823424111230034
- SmithD.DempsterC.GlanvilleJ.FreemantleN.AndersonI.Efficacy and tolerability of venlafaxine compared with selective serotonin reuptake inhibitors and other antidepressants: a meta-analysis.Br J Psychiatry.200218039640411983635
- WallaceAE.KofoedLL.WestAN.Double-blind placebo-controlled trial of methylphenidate in older, depressed, medically ill patients.Am J Psychiatry.19951529299317755127
- LecrubïerY.ClercG.DidïR.KïeserM.Efficacy of St John's wort extract WS 5570 in major depression: a double-blind, placebo-controlled trial.Am J Psychiatry.20021591361136612153829
- LindeK.RamirezG.MulrowDC.PaulsA.WeidenhammerW.MelchartD.St John's wort for depression: an overview and meta-analysis of randomised clinical trials.BMJ.19963132532588704532
- Hypericum Depression Trial Study Group: Effect of Hypericum perforatum (St John's wort) in major depressive disorder: a randomized controlled trialJAMA20022871807181411939866
- KupferDJ.FrankE.Placebo in clinical trials for depression: complexity and necessity (Editorial).JAMA.20022871853185411939872
- SheltonRC.KellerMB.GelenbergA.et al.Effectiveness of St John's wort in major depression: a randomized controlled trial.JAMA.20012851978198611308434
- HaddadPM.Antidepressant discontinuation syndromes. Clinical relevance, prevention and management.Drug Saf.20012418319711347722
- LiuB.MittmanN.KnowlesS.et al.Hyponatremia and the syndrome of inappropriate secretion of antidiuretic hormone associated with the use of selective serotonin reuptake inhibitors: a review of spontaneous reports.Can Med Assoc J.19961555195278804257
- OlverJ.BurrowsG.NormanT.Third-generation antidepressants: do they offer advantages over the SSRI?CNS Drugs.20011594195411735614
- GillHS.DeVaneLC.RischCS.Extrapyramidal symptoms associate with cyclic antidepressant treatment: a review of the literature and consolidating hypotheses.J Clin Psychopharmacol.1997173773899315989
- RosenRC.LaneRM.MenzaM.Effects of SSRI on sexual function: a critical review.J Clin Psychopharmacol.19991967859934946
- PerettiS.JudgeR.HindmarchI.Safety and tolerability considerations: tricyclic antidepressants vs selective serotonin reuptake inhibitors.Acta Psychiatr Scand Suppl.2000403172511019931
- WaldingerMD.HengeveldMW.ZwïndermanAH.et al.Effect of SSRI antidepressants on ejaculation: a double-blind, randomized, placebo-controlled study with fluoxetine, fluvoxamine, paroxetine, and sertraline.J Clin Psychopharmacol.1998182742819690692
- RosenbaumJF.FavaM.HoogSL.et al.Selective serotonin reuptake inhibitor discontinuation syndrome: a randomized clinical trial.Biol Psychiatry.19984477879646889
- HausteinK-O.HaffnerS.WoodcockBG.A review of the pharmacological and psychopharmacological aspects of smoking and smoking cessation in psychiatric patients.IntJ Clin Pharmacol Ther.20024040441812358157
- BrentDA.BirmaherB.Adolescent depression.N Engl J Med.200234766767112200555
- OxmanTE.BarrettJE.BarrettJ.GerberP.Symptomatology of late life minor depression among primary-care patients.Psychosomatics.1990311741802330398
- LynessJM.CaineED.KingDA.CoxC.YoedionoZ.Psychiatric disorders in older primary care patients.J Gen Intern Med.19991424925410203638
- SchulbergHC.KatonWJ.SimonGE.RushAJ.Best clinical practice: guidelines for managing major depression in primary medical care.J Clin Psychiatry.199960(suppl 7)S19S26
- EmslieGJ.RushAJ.WeinbergWA.et al.A double-blind, randomized, placebo-controlled trial of fluoxetine in children and adolescents with depression.Arch Gen Psychiatry.199754103110379366660
- KellerM.RyanND.StroberM.et al.Efficacy of paroxetine in the treatment of adolescent major depression: a randomized, controlled study.J Am Acad Child Adolesc Psychiatry.20014076277211437014
- WagnerKD.RobbAS.FindlingRL.JinJ.GutierrezMM.HeydornWE.A randomized, placebo-controlled trial of citalpram for the treatment of major depression in children and adolescents.Am J Psychiatry.20041611079108315169696
- AxelsonDA.PerelJM.BirmaherB.et al.Sertraline pharmacokinetics and dynamics inadolescents. J Am Acad Child Adolesc Psychiatry.20024110371044
- Treatment for Adolescents with Depression Study (TADS) Team Treatment for Adolescents with Depression Study (TADS) randomized controlled trials: fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression.JAMA.200429280782015315995
- AlexopoulosGS.KatzI.ReynoldsCF.CarpenterD.DochertyJP.RossRW.Pharmacotherapy of depressive disorders in older patients: a summary of the expert consensus guidelines.J Psychiatr Prac.20017361376
- MulsantBH.PollockBG.Psychopharmacology. In: Blazer DG, Steffans DC, Busse EW, eds.The American Psychiatric Publishing Textbook of Geriatric Psychiatry 3rd ed. Washington, DC: American Psychiatric Publishing;2004387411
- KatonaCLE.HunterBN.BrayJ.A double-blind comparison of the efficacy and safety of paroxetine and imipramine in the treatment of depression with dementia.Int J Geriatr Psychiatry.1998131001089526179
- NythAL.GottfriesCG.The clinical efficacy of citalopram in treatment of emotional disturbances in dementia disorders, a nordic multicentre study.Br J Psychiatry.19901578949011705151
- NythAL.GottfriesCG.LybyK.et al.A controlled multicenter clinical study of citalopram and placebo in elderly depressed patients with and without concomitant dementia.Acta Psychiatr Scand.1992861381451529737
- OlafssonK.JorgensenS.JensenHV.BilleA.ArupP.AndersonJ.Fluvoxamine in the treatment of demented elderly patients: a double-blind, placebo-controlled study.Acta Psychiatr Scand.1992854534561642129
- TaraganoFE.LyketsosCG.MangoneCA.AHegriRF.Comesana-DiazE.A double-blind, randomized, fixed-dose trial of fluoxetine vs amitriptyline in the treatment of major depression complicating Alzheimer's disease.Psychosomatics.1997382462529136253
- RooseSP.Considerations for the use of antidepressants in patients with cardiovascular disease.Am Heart J.2000140(4 suppl)S84S88
- KrïshnanKR.DelongM.KraemerH.et al.Comorbidity of depression with other medical diseases in the elderly.Biol Psychiatry.20025255958812361669
- AndersenG.VestergaardK.LauritzenL.Effective treatment of poststroke depression with the selective serotonin reuptake inhibitor citalopram.Stroke.199425109911048202964
- RobinsonR.SchultzS.CastilloC.Nortriptyline versus fluoxetine in the treatment of depression and in short-term recovery after stroke: a placebocontrolled, double-blind study.Am J Psychiatry.200015735135910698809
- ArranzFJ.RosS.Effects of comorbidity and polypharmacy on the clinical usefulness of sertraline in elderly depressed patients: an open multicentre study.J Affect Disord.1997462852919547126
- EvansM.HammondM.WilsonK.LyeM.CopelandJ.Treatment of depression in the elderly: effect of physical illness on response.Int J Geriatr Psychiatry.199712118911949444543
- GoodnickPJ.HernandezM.Treatment of depression in comorbid medical illness.Expert Opin Pharmacother.200011367138411249471
- SolaiLK.MulsantB.PollockBG.Selective serotonin reuptake inhibitors for late-life depression: a comparative review.Drugs Aging.20011835536811392444
- TraplerB.CohenCI.Use of SSRI in “very old” depressed nursing home residents.Am J Geriatr Psychiatry.1998683899469218
- MulsantBH.AlexopoulosGS.ReynoldsCF.et al.Pharmacological treatment of depression in older primary care patients: the PROSPECT algorithm.Int J Geriatr Psychiatry.20011658559211424167
- FurlanPM.KalianMJ.Ten HaveT.PollockBG.KatzI.LuckiI.Cognitive and psychomotor effects of paroxetine and sertraline on healthy elderly volunteers.Am J Geriatr Psychiatry.2001942943811739070
- NewhousePA.KrishnanKR.DoraiswamyPM.RichterEM.BatzarED.ClaryCM.A double-blind comparison of sertraline and fluoxetine in depressed elderly outpatients.J Clin Psychiatry.20006155956810982198
- SchneiderLS.NelsonJC.ClaryCM.et al.An 8-week multicenter, parallel-group, double-blind, placebo-controlled study of sertraline in elderly outpatients with major depression.Am J Psychiatry.20031601277128512832242
- RooseSP.SackeimHA.KrishnanKRR.et al.Antidepressant pharmacotherapy in the treatment of depression in the very old: a randomized, placebo-controlled trial.Am J Psych ia try.200416120502059
- PollockBG.Adverse reactions of antidepressants in elderly patients.J Clin Psychiatry.199960(suppl 20)S4S8
- NierenbergAA.AmsterdamJD.Treatment-resistant depression: definition and treatment approaches.J Clin Psychiatry.19905139472112132
- ThaseME.RushAJ.Treatment-resistant depression. In: Bloom FE, Kupfer DJ, eds.Psychopharmacology: The Fourth Generation of Progress. New York, NY: Raven Press;199510811098
- O'ReardonJP.AmsterdamJD.Treatment-resistant depression: progress and limitations.Psych Ann.199828633640
- KellerMB.ShapiroRW.LavoriPW.WolfeN.Relapse in major depressive disorder: analysis with the life table.Arch Gen Psychiatry.1982399119157103680
- PaykelES.Epidemiology of refractory depression. In: Nolen WA, Zohar J, Roose SP, Amsterdam JD, eds.Refractory Depression: Current Strategies and Future Directions. New York, NY: Wiley;1994318
- SoueryD.AmsterdamJ.de MontïgnyC.et al.Treatment resistant depression: methodological overview and operational criteria.Eur Neuropsychopharmacol.19999839110082232
- FagioliniA.KupferDJ.Is treatment-resistant depression a unique subtype of depression?Biol Psychiatry.20035364064812706950
- RushAJ.FavaM.WïsnïewskïSR.et al.Sequenced Treatment Alternatives to Relieve Depression (STAR*D): rationale and design.Control Clin Trial.200425119142
- OhayonMM.SchatzbergAF.Prevalence of depressive episodes with psychotic features in the general population.Am J Psychiatry.20021591855186112411219
- CharneyDS.NelsonJC.Delusional and nondelusional unipolar depression: further evidence for distinct subtypes.Am J Psychiatry.19811383283336110345
- CoryellW.TsuangMT.Primary unipolar depression and the prognostic importance of delusions.Arch Gen Psychiatry.198239118111847125847
- ParkerG.RoyK.Hadzi-PavlovîcD.PedicF.Psychotic (delusional) depression: a meta-analysis of physical treatments.J Affect Disord.19922417241347545
- SpikerDG.WeissJC.DealyRS.et al.The pharmacological treatment of delusional depression.Am J Psychiatry.19851424304363883815
- DubeS.AndersenSW.SangerTM.HostetlerJ.TohenMF.TollefsonGD.Olanzapine-fluoxetine combination for psychotic major depression. Presented at: 155th Annual Meeting of the American Psychiatric Association; Philadelphia, Pa. 2002 5 18-23
- BelanoffJK.RothschildAJ.CassïdyF.et al.An open label trial of C-1073 (mifepristone) for psychotic major depression.Biol Psychiatry.20025238639212242054
- RothschildAJ.Challenges in the treatment of depression with psychotic features.Biol Psychiatry.20035368069012706954
- HimmelhochJM.ThaseME.MallingerAG.HouckP.Tranylcypromine versus imipramine in anergic bipolar depression.Am J Psychiatry.19911489109162053632
- GoodwinFK.JamisonKR.Manic-Depressive Illness. New York, NY: Oxford University Press;1990
- ThaseME.SachsGS.Bipolar depression: pharmacotherapy and related therapeutic strategies.Biol Psychiatry.20004855857211018227
- CalabreseJR.BowdenCL.SachsG.et al.A placebo-controlled 18-month trial of lamotrigine and lithium maintenance treatment in recently depressed patients with bipolar I disorder.J Clin Psychiatry.2003641013102414628976
- TohenM.VietaE.CalabreseJR.et al.Efficacy of olanzapine and olanzapine-fluoxetine combination in the treatment of bipolar I depression.Arch Gen Psychiatry.2003601079108814609883
- American Psychiatric Association Practice guideline for the treatment of patients with bipolar disorder (revision).Am J Psychiatry.2002156350
- ThaseME.SachsGS.The challenges of pharmacotherapy of bipolar disorder.Clin Neurosci Res.20022213221
- CalabreseJR.BowdenCL.SachsGS.AscherJA.MonaghanE.RuddGD.A double-blind placebo-controlled study of lamotrigine monotherapy in outpatients with bipolar I depression.J Clin Psychiatry.199960798810084633
- NemeroffCB.EvansDL.GyulaiL.SachsGS.BowdenCL.GergelIP.Doubleblind, placebo-controlled comparison of imipramine and paroxetine in the treatment of bipolar depression.Am J Psychiatry.200115890691211384898
- EmslieGJ.HeiligensteinJH.WagnerKD.et al.Fluoxetine for acute treatment of depression in children and adolescents: a placebo-controlled, randomized clinical trial.J Am Acad Child Adolesc Psychiatry.2002411205121512364842
- KellerM.RyanND.StroberM.et al.Efficacy of paroxetine in the treatment of adolescent major depression: a randomized, controlled trial.J Am Acad Child Adolesc Psychiatry.20014076277211437014
- UmapathyC.MulsantBH.PollockBG.Bipolar disorder in the elderly.Psychiatr Ann.200030473480
- NunesEV.DeliyannidesD.DonovanS.McGrathPJ.The management of treatment resistance in depressed patients with substance use disorders.Psychiatr Clin North Am.1996193113278827192
- WorthingtonJ.FavaM.AgustinC.et al.Consumption of alcohol, nicotine, and caffeine among depressed outpatients: relationship with response to treatment.Psychosomatics.1996375185228942202
- AlpertJE.LagomasinoIT.Psychiatric comorbidity in treatment-resistant depression. In: Amsterdam JD, Hornig M, Nierenberg AA, eds.Treatment-Resistant Mood Disorders. New York, NY: Cambridge University Press;2001430478
- O'ReardonJP.AmsterdamJD.Medical disorders and treatment-resistant depression. In: Amsterdam JD, Hornig M, Nierenberg AA, eds.Treatment-Resistant Mood Disorders. New York, NY: Cambridge University Press;2001405429
- Frasure-SmithN.LesperanceF.TalajicM.Depression following myocardial infarction: impact on 6-month survival.JAMA.1993270181918258411525
- AhernDK.GorkinL.AndersonJL.et al.Biobehavioral variables and mortality or cardiac arrest in the Cardiac Arrhythmia Pilot Study (CAPS).Am J Cardiol.19906659622193497
- KaufmannMW.FïtzgibbonsJP.SussmanEJ.et al.Relation between myocardial infarction, depression, hostility, and death.Am Heart J.199913854955410467207
- BushDE.ZiegelsteïnRC.TaybackM.et al.Even minimal symptoms of depression increase mortality risk after acute myocardial infarction.Am J Cardiol.20018833734111545750
- Frasure-SmithN.LesperanceF.Depression: a cardiac risk factor in search of a treatment.JAMA.20032893171 317312813125
- GlassmanAH.O'ConnorCM.CalïffRM.et al.Sertraline treatment of major depression in patients with acute MI or unstable angina.JAMA.200228870170912169073
- GeddesJR.ButlerR.Depressive Disorders in Adults: Clinical Evidence. London, UK: BMJ Publishing Group;2002
- SchulbergHC.KatonW.SimonGE.RushAJ.Treating major depression in primary care practice: an update of the Agency for Health Care Policy and Research Practice Guidelines.Arch Gen Psychiatry.199855112111279862556
- GeddesJR.CarneySM.DaviesC.et al.Relapse prevention with antidepressive drug treatment in depressive disorders: a systematic review.Lancet.200336165366112606176
- GilaberteI.MontejoAL.de la GandaraJ.et al.Fluoxetine in the prevention of depressive recurrences: a double-blind study.J Clin Psychopharmacol.20012141742411476126
- KlysnerR.Bent-HansenJ.HansenHL.et al.Efficacy of citalopram in the prevention of recurrent depression in elderly patients: placebo-controlled study of maintenance therapy.Br J Psychiatry.2002181293512091260
- HochstrasserB.IsaksenPM.KoponenH.et al.Prophylactic effect of citalopram in unipolar, recurrent depression: placebo-controlled study of maintenance therapy.Br J Psychiatry.200117830431011282808
- LepineJP.GaillardV.BisserbeJC.et al.A randomized, placebo-controlled trial of sertraline for prophylactic treatment of highly recurrent major depressive disorder.Am J Psychiatry.200416183684215121648
- KellerMB.KocsisJH.ThaseME.et al.Maintenance phase efficacy of sertraline for chronic depression: a randomized controlled trial.JAMA.1998280166516729831997
- KocsisJH.FriedmanRA.MarkowïtzJC.et al.Maintenance therapy for chronic depression: a controlled clinical trial of desipramine.Arch Gen Psychiatry.1996537697748792753
- NestlerEJ.GouldE.ManjiH.et al.Preclinical models: status of basic research in depression.Biol Psychiatry.20025250352812361666
- KraemerHC.LoweKK.KupferDJ.To Your Health: How to Understand What Research Tells Us About Risk. New York, NY: Oxford University Press;2005