Abstract
Suffering related to dementia is multifaceted because cognitive and physical functioning slowly deteriorates. Advanced age and sex, two of the most prominent risk factors for dementia, are not modifiable. Lifestyle factors such as smoking, excessive alcohol use, and poor diet modulate susceptibility to dementia in both males and females. The degree to which the resulting health conditions (eg, obesity, type 2 diabetes, and cardiovascular disease) impact dementia risk varies by sex. Depending on the subtype of dementia, the ratio of male to female prevalence differs. For example, females are at greater risk of developing Alzheimer disease dementia, whereas males are at greater risk of developing vascular dementia. This review examines sex and gender differences in the development of dementia with the goal of highlighting factors that require further investigation. Considering sex as a biological variable in dementia research promises to advance our understanding of the pathophysiology and treatment of these conditions.
El sufrimiento relacionado con la demencia es multifacético porque el funcionamiento cognitivo y físico se deteriora lentamente. La edad avanzada y el sexo, dos de los factores de riesgo más importantes para la demencia, no son modificables. Los factores del estilo de vida, como el fumar, el uso excesivo de alcohol y la dieta pobre modulan la susceptibilidad a la demencia tanto en hombres como en mujeres. El grado por el cual las condiciones de salud resultantes (como obesidad, diabetes tipo 2 y enfermedad cardiovascular) impactan en el riesgo de demencia varía según el sexo. Según el subtipo de demencia la relación de la prevalencia hombre mujer es diferente. Por ejemplo, las mujeres tienen mayor riesgo de desarrollar demencia tipo Enfermedad de Alzheimer, en cambio los hombres tienen mayor riesgo de desarrollar demencia vascular. Esta revisión examina las diferencias por sexo y género en el desarrollo de las demencias, con el propósito de destacar los factores que requieren de futuras investigaciones. El tener en consideración el sexo como una variable biológica en la investigación de las demencias promete avanzar en la comprensión de la fisiopatología y terapéutica de estas condiciones.
La souffrance liée à la démence est multiforme, car les fonctionnements cognitif et physique se détériorent lentement. L'âge avancé et le sexe, deux des principaux facteurs de risque de démence, ne sont pas modifiables. Les facteurs de mode de vie comme le tabagisme, l'alcoolisme et une mauvaise alimentation modulent la susceptibilité à la démence chez les hommes comme chez les femmes. L'impact des pathologies (par ex. l'obésité, le diabète de type 2 et les maladies cardiovasculaires) sur le risque de démence varie selon le sexe. Selon le sous-type de démence, la prévalence du rapport hommes/femmes diffère. Par exemple, les femmes ont plus de risque de développer une démence de type Alzheimer, tandis que les hommes ont plus de risque de développer une démence vasculaire. Cet article examine les différences de sexe et de genre dans le développement des démences afin de souligner les facteurs qui nécessitent davantage de recherche. Envisager le sexe comme une variable biologique dans la recherche sur les démences permettra de mieux comprendre la physiopathologie et le traitement de ces maladies.
Introduction
Dementia is a pathological, neurodegenerative process leading to progressive decline in cognitive and functional abilities. It has multiple causes, diverse manifestations, and heterogeneity with respect to the impact of sex or gender on prevalence, risk factors, and outcomes (Table I).Citation1-Citation17 Alzheimer disease (AD) is the most common form of dementia, comprising up to 80% of cases; however, not all studies distinguish AD from all-cause dementia. The estimated prevalence of all-cause dementia varies from 4.7% in Central Europe to 8.7% in North Africa/Middle East, with North America falling between at 6.4%. Currently, over 46 million individuals live with dementia worldwide and this number is projected to increase to 131.5 million by 2050. The economic impact is enormous. By 2018, dementia is expected to become a trillion dollar disease. To put these costs in more tangible terms, dementia care, if it were a country, would be the world's 18th largest economy.Citation18
TABLE I. Prevalence/incidence of disorders leading to dementia and the impact of sex or gender. LOC, loss of consciousness; TBI, traumatic brain injury.
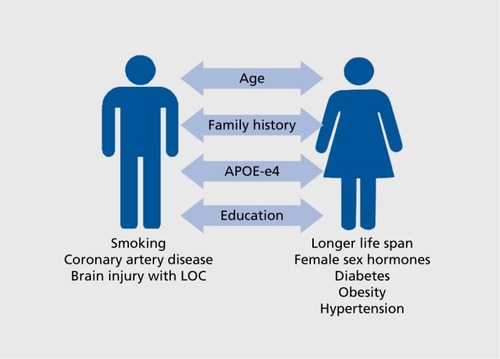
Current treatments for dementia are inadequate in slowing the progression of disease, and there are no cures, with the possible exception of dementia related to normal pressure hydrocephalus (NPH). Hence, identification of modifiable risk factors () has been a primary focus of much investigation. Unfortunately, the two strongest predictors of dementia—age and sex—do not fall into this category. Moreover, sex and gender factors interact with age across development to alter risk for dementia. Beginning in utero and onward, the brain is acted upon in a sexually dimorphic manner. This promotes risk and resilience with respect to health outcomes across the life span.
This review will examine current knowledge regarding individual and interactive effects of sex and gender as they relate to dementia risk, prevention, and treatment. Briefly, sex refers to the classification of human beings according to their sex chromosomal compliment, with females having two X chromosomes and males having one X and one Y chromosome. Gender refers to a person's psychosocial and cultural self-identification as being male or female. Past researchers have reviewed sex- and gender-specific risk factors for development of dementia; however, the separation of sex as a biological variable (SABV) and gender as a societal construct/personal identity has not always been clearly defined in dementia research. The waters between sex and gender can indeed be muddy when considering that aspects of gender influence an individual's biology, and vice versa. Similarly, one's gender does not always conform to one's biological sex. Although there is a growing need to consider health outcomes in transgender and intersex communities, this review will focus on sex and gender differences in dementia among individuals who have expected chromosomal compliment for males (XY) and females (XX) and are not utilizing exogenous hormones or surgical procedures to alter their gender or sexual identity.
Impact of sex and gender during development: setting the stage
Seminal work conducted by McCarthy and Arnold and othersCitation19-Citation21 implicates a critical role of testosterone and its aromatization to estradiol in sexing of the human brain, with a greater degree of exposure enhancing masculinization. Variations in hormonal exposures/responses occur throughout the central nervous system (CNS) between brain regions and individual cells, leading to a mosaic of maleness and femaleness in any given brain.Citation22,Citation23 After birth, organizational effects of gonadal hormones are thought to be relatively quiescent until puberty when male and female gonads begin to produce sex steroids. However, brain regions (eg, hippocampus and prefrontal cortex) and physiologic processes (eg, cerebral blood flow) that are critical to cognition and brain health are rapidly developing across childhood and adolescence and thus vulnerable to environmental perturbations. Sex differences already present at birth can conceivably modify the individual's response to medical conditions and environmental insults such as adversity, whereas gender is associated with specific types of traumatic exposures.Citation24 Education, intellectual enrichment, and cognitive reserve are additional factors in the risk for dementia that may vary by gender.Citation25,Citation26 Although the vast majority of individuals receive some form of education during childhood, there are considerable gender disparities in the level of educational attainment in some countries and cultures. Moreover, education attainment interacts with gonadal steroids in a sex-specific manner. Among older men, low levels of free testosterone increased the risk of dementia to a greater degree in men with a high level of education than in those with a low level of education.Citation27 Gender differences in these and other exposures can interact with the biology of the individual in a sex-specific manner, which highlights the complexity of sex and gender when considering adult health outcomes.
Examples of early and developmental sex differences come from the large Philadelphia Neurodevelopmental Cohort in which individuals ages 8 to 22 years underwent brain imaging.Citation28 The basic physiologic process of cerebral perfusion is critical for brain metabolism and is diminished in numerous neurological disorders. This differs in magnitude and direction between males and females across development.Citation29-Citation31 Again, in the Philadelphia Neurodevelopmental Cohort, amygdala volume increased significantly in adolescent boys, whereas hippocampal volume increased and thinning of cortical gray matter occurred faster in girls.Citation32 These sex differences are crucial to consider when interpreting brain-imaging outcomes in normally developing individuals, as well as in those with neuropsychiatric and cognitive disorders. Sex differences in brain development serve as the proverbial stage on which medical conditions and other risk factors associated with dementia act to increase or reveal vulnerability to pathological cognitive aging.
Sex/gender differences in dementia by subtype
Alzheimer disease
AD, the most common cause of dementia, is characterized by β-amyloid plaques, neurofibrillary tangles, and neurodegeneration in areas of the brain associated with cognition, such as the cortex and hippocampus. The disruption to critical metabolic processes leads to cell death, neuronal loss, and progressive decline from mild cognitive impairment (MCI) to AD dementia.Citation33,Citation34 AD is characterized by interference with everyday activities involving memory, speech and language, reasoning, planning, and other cognitive abilities.Citation35,Citation36 Advanced age is the strongest predictor; however, sex and gender differences have been noted in prevalence, clinical manifestation, disease course, and prognosis.Citation37 Data from the Framingham Study, which enrolled a total of 2611 cognitively intact participants (1550 women and 1061 men) and followed up on many for 20 years, indicated that for a 65-year-old man, remaining lifetime risk of AD was 6.3% (95% confidence interval [CI], 3.9 to 8.7) and remaining lifetime risk of developing any dementing illness was 10.9% (95% CI, 8.0 to 13.8); corresponding risks for a 65-year-old woman were 12% (95% CI, 9.2 to 14.8) and 19% (95% CI, 17.2 to 22.5), almost twice that of men.Citation1
Several epidemiologic studies show that neurodegeneration and clinical symptoms occur more rapidly for females once a diagnosis is suspected.Citation36,Citation38-Citation40 Researchers have hypothesized that this is due to longer female life expectancy or sociocultural detection biasCitation34; however, there is support that faster progression is due to neurobiological vulnerability in postmenopausal females.Citation1,Citation36 Though progression of the disease may be more rapid among elderly women, studies conducted in the United States and United Kingdom suggest that males with AD have a shorter survival time.Citation41,Citation42 Women are often diagnosed earlier in the course of illness than men, which could confound determination of postdiagnosis longevity. However, data from a recent systematic review focusing on mortality in AD and all-cause dementia support findings of a shorter life span among males, regardless of age at diagnosis.Citation43 Among those who have a positive or stable response to cholinesterase inhibitors over 6 months, female sex is a predictor of longer life span.Citation44
The importance of considering SABV and gender with other risk factors for dementia such as apolipoprotein E (APOE) genotype, alcohol use, and depression, has become increasingly apparent. The APOE gene encodes a protein that transports cholesterol in the bloodstream. Carriers of the ε4 variant are predisposed to high cholesterol and AD. When examined at autopsy, a greater portion of individuals diagnosed with AD were found to have one or two copies of the APOE ε4 allele.Citation2 Female allele carriers were twice as likely as noncarriers to have dementia, and allele status predicted progression from MCI to AD in both sexes.Citation45 The CREDOS study (Clinical Research Center for Dementia of South Korea) of 301 individuals with MCI at enrollment confirmed that APOE ε4 status is a predictor of transition from MCI to AD in both males and females. However, APOE ε4 status affected the rapidity with which women transitioned, as did clinically relevant levels of depression at baseline. For men with MCI, baseline burden of periventricular white matter hyperintensities predicted a more rapid transition from MCI to AD over 3-year follow-up.Citation37 APOE ε4 allele status has been suggested to interact with degree of alcohol consumption to promote risk or resilience to AD and other dementias. Further research is necessary to define light-to-moderate alcohol consumption by sex, determine effects of different types of alcohol, and consider co-use of alcohol and cigarettes on dementia risk.Citation46,Citation47 Finally, several sex and APOE genotype interactions have been described for effectiveness of treatments used to slow progression of cognitive decline in AD. Treatment with intranasal insulin showed a positive impact on cognition in male APOE ε4 carriers versus noncarriers, whereas their female APOE ε4-negative female counterparts experienced worsening cognition during insulin treatment.Citation48 Impact of APOE ε4 genotype status in men and women with respect to response to cholinesterase inhibitors has been decidedly mixed.Citation49 Knowledge of these sex differences in risk factors with respect to prevention, treatment, and prognosis highlight the importance of inclusion of SABV in all studies of normal cognitive aging, MCI, and dementia. The relationship between female sex and depression is particularly important given recent evidence that selective serotonin reuptake inhibitor treatment reduces accumulation of β-amyloid plaques in rodents and cerebrospinal levels of β-amyloid in humans.Citation50
Results from preclinical and human observational studies of estradiol treatment before a prolonged period of hypogonadism suggest a neuroprotective effect of estradiol.Citation51 The impact of estradiol on brain structure and function with respect to cognition are profoundCitation52-Citation54 and beyond the scope of this review. A study by the Women's Health Initiative (WHI), though important, created some confusion regarding the role of estrogen in preventing cognitive decline.Citation51,Citation55 Since the WHI released its findings of increased risk for thromboembolic events and cognitive decline in women randomized to conjugated equine estrogen and progestin medroxy-progesterone acetate, both preclinical and clinical researchers have put forth the “healthy cell hypothesis” that estradiol serves as a protectant when neural tissue is healthy.Citation56 Administration of estrogen after prolonged periods of hypogonadism, which was the experience of many WHI participants, has been shown to diminish the neuroprotective profile of the hormone and enhance markers of neuroinflammation. Cells have essentially become “less healthy” during the period of hypogonadism and aging.Citation57-Citation59
Development of AD at a later age among women has been linked to greater lifetime exposure to estrogens.Citation60 Nonetheless, during the late menopause transition, women experience a profound decrease in estradiol levels. Age-matched men either maintain their lifelong levels of gonadal steroids or experience a relatively slow decline in testosterone synthesis.Citation34,Citation61 Reductions in estradiol levels during the fifth decade and beyond may be responsible for deficits in brain metabolism and vascular pathologies, primarily among females, as age-matched males would still be aromatizing testosterone to estrogen. “Brain sex,” the degree of feminization and masculinization during development, is likely to moderate neuroprotective effects of estradiol and testosterone.Citation61
Inflammation is another risk factor for AD that varies by sex,Citation62 with inflammatory dysregulation being stronger in females.Citation63 Preclinical research suggests important sex differences in microglia, the primary immune cell of the CNS, during development and in response to fluctuating gonadal steroids across the life span. Females have been shown to have more microglia than in males, especially during adolescence, a time when female-biased disorders such as depression and anxiety are on the rise. Although causes of AD are unclear, it is possible that this disruption in microglia sets the stage for development of neurodegenerative diseases in older adulthood.Citation62,Citation64 Others have reported sexually dimorphic effects of glucocorticoids in brain regions critical to cognition.Citation65 In humans, low-grade inflammation is a feature of a number of medical conditions such as diabetes, obesity, and depression, which are risk factors themselves for AD and vary in prevalence and impact on AD risk, as well as that of other dementia subtypes.Citation66
Vascular dementia
Vascular dementia results from ischemic or hemorrhagic insults to regions of the brain critical for cognitive functions.Citation67 Research conducted worldwide indicates that stroke prevalence, whether ischemic or hemorrhagic, is 44% higher in men than women. In addition, men experience their first stroke at a younger age, 68.6 years versus 72.9 years.Citation3 Findings from the Framingham Study, however, indicate that women have a greater lifetime risk of stroke, perhaps given their longer life expectancy; increasing risk of stroke with ageCitation68; and increased risk for thrombosis and stroke with atrial fibrillation and diabetes.Citation69 A 2009 systematic review of the literature indicates that strokes tend to be more severe in women, with a 1-month case fatality of 24.7% in females and 10.7% in males.Citation3
Dementia is a consequence and a risk factor for stroke and vascular dementia. Many of the risk factors for stroke and multi-infarct dementia, such as atrial fibrillation, heart failure, high blood pressure, atherosclerosis, obesity, and diabetes, are more common among men, but women suffer disproportionate risk for dementia related to many of these risk factors.Citation70,Citation71 In a pooled analysis of 2.3 million individuals with over 100 000 cases of dementia, type 2 diabetes increased the risk for developing dementia by 60%. In this sample, risk for dementia among women with diabetes was 19% greater than for men.Citation71 Female sex, medial temporal lobe atrophy, and family history of dementia, are stronger predictors of pre- than poststroke dementia. Prestroke dementia may be a sign or cause of a primary degenerative pathology that increases the likelihood of vascular events.Citation72 Women are more likely than men to experience poststroke depression, another risk factor for dementia.Citation73
Lewy body dementia
The pathognomonic pathology in Lewy body dementia (LBD) is an abnormal accumulation of the protein α-synuclein, referred to as a Lewy body. Besides cognitive decline, common symptoms of LBD are visual hallucinations, sleep disturbance, autonomic dysregulation, fluctuating attention, depression, and Parkinson-like symptoms of bradykinesia, rigidity, and tremor. Clinically, LBD is distinguished from PDD by onset of dementia before or within the first year of onset of parkinsonism. Autopsy studies suggest that LBD accounts for 15% to 25% of dementia cases, making it the third most common type of dementia.Citation74-Citation76 Autopsy registries of individuals who died with known dementia revealed that Lewy bodies were present almost three times more often in males, regardless of age, smoking history, or education.Citation4 This sex difference in prevalence is consistent with a recent analysis of LBD and PDD among citizens of Olmsted, Minnesota, diagnosed with parkinsonism between 1991 and 2005. There was an almost fourfold higher incidence rate for LBD among men in this population study.Citation77 This male predominance is interesting given one of the risk factors for LBD is having a previous diagnosis of depression or anxiety, conditions more common among women.Citation78
Frontotemporal dementia
Unlike previously discussed dementias, frontotemporal dementia (FTD) is most prevalent among those 60 to 69 years of age, with roughly 13% having onset when younger than age 50.Citation16 Younger onset may be due in part to heavy genetic loading for FTD, with up to 50% of cases being familial and up to 40% autosomal-dominant in nature.Citation16 At least five genetic loci are associated with FTD, but none will be discussed herein as there are no data, to our knowledge, regarding potential sex interactions with these genes. Nongenetic risk factors include head trauma and thyroid disease.Citation79 Estimated point prevalence documented in several large studies is 15 to 22/100 000 individuals,Citation80,Citation81 and there is evidence of a three-to-4.7-fold greater prevalence in males than in females,Citation14,Citation15 although this sex distribution has not been supported by all studies.Citation82,Citation83 Inconsistency in prevalence with respect to sex differences between studies may be due, in part, to heterogeneity in clinical presentations. Based upon the predominant early features, there is a behavioral variant of FTD both with and without evidence of motor-neuron disease, such as amyotrophic lateral sclerosis (ALS) and atypical parkinsonism. The behavioral variant is characterized by progressive behavioral impairment and decline in executive function; the semantic dementia variant is characterized by loss of object knowledge and anomia; and the progressive nonfluent aphasia (PNFA) variant is characterized by expressive or motor speech deficits.Citation84
Given the midlife onset of FTD, there is a dramatic reduction in life expectancy that does not appear to differ by sex.Citation16 Survival partially depends on the variant of FTD and ranges from 2 to 3 years after symptom onset when motor neuron symptoms are prominent and up to 12 years for the semantic dementia variant.Citation16
Dementia from multiple causes (mixed dementia)
Mixed dementia refers to cognitive impairment due to multiple CNS pathologies. Most commonly, these pathologies are a combination of AD pathologies—β-amyloid deposits and tau tangles—and vascular compromise, such as that occurring with multiple microbleeds or infarcts.Citation85 Autopsy reports suggest that vascular pathology occurs in up to 28% of AD cases.Citation9,Citation10,Citation86 Dementia related to Parkinson disease (PD) is frequently accompanied by vascular-related lesions. A recent report from two longitudinal population-based studies, the Nun Study and HAAS (Honolulu-Asia Aging Study), found that neuropathic abnormalities such as Lewy bodies and AD changes were more common among white women in the Nun Study, whereas microinfarcts were more common in Japanese American HAAS men. As expected, cognitive decline was greatest among individuals with multiple types of neuropathologic changes, whether Lewy bodies, AD pathology, or vascular disease.Citation87 Cerebrospinal fluid markers of AD found in individuals diagnosed with LBD were associated with a more rapid cognitive decline among those participating in a large European multicenter study of LBD.Citation88 It is generally accepted that vascular dementias and mixed dementias occur more frequently in males, with rates of 31% versus 25% in females.Citation76,Citation11
Parkinson disease dementia
PD, a movement disorder characterized by bradykinesia, rigidity, tremor at rest, gait disturbance, and difficulty with speech, is more prevalent in males. Loss of midbrain dopaminergic neurons in the substantia nigra pars compacta and consequent loss of dopamine input to the caudate nucleus and putamen (striatum) lead to the motor and nonmotor symptoms of PD. Depression, anxiety, insomnia, and cognitive decline, can impact quality of life for individuals with PD to a degree that rivals that of the motor symptoms.Citation89 The prevalence of PD is between 0.3% and 3% of the population worldwide, with a 2 to 1 male to female ratio at any given age.Citation5,Citation6 On average, women are diagnosed 2 years later (53.4 years) than men (51.3 years),Citation7 perhaps due to a milder disease presentation among women. Women are likelier to present with a mild tremor, which is associated with a slower rate of motor decline. Whereas rigidity is more common among men with PD, dyskinesia and depression are more common among women with PD.Citation7
Sex differences in progression to dementia among individuals with PD are unclear. Men with PD have been reported to experience greater deficits in verbal fluency and recognition of facial emotions, whereas women reportedly experience more difficulties in visuospatial cognition.Citation7,Citation90 Findings from the NET-PD LS-1 (National Institutes of Health Exploratory Trials in Parkinson's Disease Long-Term Study-1) suggest that among individuals undergoing treatment during the early stages of PD, women fare better than men with respect to cognitive functioning.Citation8
Several additional nonmotor symptoms differ in prevalence and severity by sex. Women with PD are likelier to report fatigue, nervousness, sadness, constipation, and restless legs, whereas men report more difficulties pertaining to daytime sleepiness, dribbling saliva, interest in sex, and problems having sex.Citation91-Citation93 Life expectancy and quality of life are diminished among individuals with PD who develop dementia, regardless of sex.Citation94
Normal pressure hydrocephalus
The classic presentation for normal pressure hydrocephalus (NPH) is the triad of gait or motor disturbance, cognitive impairment, and bladder sphincter dysfunction, but individuals may present with some combination thereof.Citation12 Cognitive, motor, and behavioral changes associated with NPH occur as normal flow of cerebrospinal fluid within the brain becomes blocked, cerebrospinal fluid builds up, ventricles expand, and cortical tissue is compressed.Citation12,Citation95 NPH can be secondary to CNS insults, such as subarachnoid hemorrhage and infection, but cases with no identifiable cause are common and are referred to as idiopathic. The overall prevalence of NPH ranges from 0.02% to up to 5.9%, depending upon age and specific population studied.Citation96,Citation97
Timely diagnosis of NPH is critical, as shunting to drain the cerebrospinal fluid can reduce pressure on the brain and improve prognosis.Citation13 In a large population study conducted in Spain, where the male-to-female ratio for individuals 60 years and older was 0.756:1 in the general population, the male-to-female ratio for those with idiopathic NPH (iNPH) was 1.39:1 (P<0.0001). The corresponding incidence rate ratio between male and females with iNPH was 1.838 (P<0.0001), indicating that iNPH is almost twice as likely to occur in older males than older females.Citation12
Creutzfeldt-Jakob disease
Creutzfeldt-Jakob disease (CJD) occurs primarily in individuals older than 60 years of age and affects roughly 1 out of a million individuals worldwide. Although much about the pathophysiology of the disease is not known, investigators believe that the disease is caused by a prion, or misfolded protein, which aggregates in the brain and leads to neuronal death.Citation17 In some variant cases, CJD presents with psychiatric symptoms, but problems with muscular coordination, personality changes, impaired vision, and rapidly progressive dementia are more common presentations.Citation98 As with many other dementias, confirmation of diagnosis occurs postmortem when, in the case of CJD, spongiform changes in the brain can be directly observed. Premortem electrocephalography (EEG) can identify periodic sharp-wave complexes in approximately two thirds of patients whose diagnosis is later confirmed by pathology. Whether sporadic, inherited, or by contamination, cases of CJD do not appear to vary by sex, nor is survival time of 3.8 months (on average) from diagnosis different in males and females.Citation17 It is known, however, that cerebrospinal fluid levels of T-tau and P-tau, markers of CJD, were significantly higher in women diagnosed with CJD in Sweden between 2002 and 2012, suggesting that CNS changes related to prions may differ to some degree in females.Citation99
Conclusions
Dementia prevalence and risk factors vary by and interact with the sex of the individual in some, but not all, types of dementia. Reproductive hormones and environmental factors program the brain in a sexually dimorphic manner across early development. Our understanding of the importance of this window of development with respect to risk and resilience for dementia is an area of increasing interest, as sex differences in brain development set the stage on which lifestyle and health conditions exert an influence. Gender comes into play when societal factors create opportunities for advanced education and healthy lifestyles.
Behavioral interventions that target risk factors for dementia, such as those that focus on diet and exercise, must consider gender in order to be successful. Prevalence of exercise across the life span, uptake and compliance with recommended exercise plans, and motivation for physical activity vary by sex.Citation100-Citation102 Regrettably, there is a dearth of literature regarding the impact of sex on response to pharmacotherapy, including hormone therapy, in the prevention and treatment of dementia.
We are aware that risk factors interact with sex in several cases, but there is no literature clearly indicating whether sex impacts the effectiveness of strategies to prevent or target these risk factors. For example, we previously discussed the fact that type 2 diabetes exerts a greater risk for dementia among women than men. However, it is not known whether adequate glucose control would reverse this disproportionate risk among women. Similarly, concussion with loss of consciousness is more common among males, and thyroid disease occurs more frequently in women; however, to our knowledge, there is no literature regarding the role of sex in these conditions as it relates to risk for FTD or whether effective treatment of these conditions is preventative.
Given the prevalence of dementia in our society and the vast number of individuals who will be affected in the decades to come, it is critical that we further our understanding of how sex and gender create risk and resilience for dementia. Because sex is not typically modifiable, both it and gender may influence our treatments and the effectiveness in targeting modifiable risk factors.
Selected abbreviations and acronyms
| AD | = | Alzheimer disease |
| APOE | = | apolipoprotein E |
| CI | = | confidence interval |
| CJD | = | Creutzfeldt-Jakob disease |
| CNS | = | central nervous system |
| FTD | = | frontotemporal lobe dementia |
| LBD | = | Lewy body dementia |
| MCI | = | mild cognitive impairment |
| NPH | = | normal pressure hydrocephalus |
| PD | = | Parkinson disease |
Conflict of interest/Disclosures: C Neill Epperson discloses that she has received research grant support from Sage Therapeutics and Shire. Dr Epperson consults to both Forest Laboratories and Asarina Pharmaceuticals. Dr. Epperson and/or her family have investments in Pfizer, Eli Lily, Merck, Abbvie, Abbott, and Johnson and Johnson.
REFERENCES
- SeshadriS1.WolfPA.BeiserA.et alLifetime risk of dementia and Alzheimer's disease. The impact of mortality on risk estimates in the Framingham Study.Neurology.1997496149815049409336
- FarrerLA.CupplesLA.HainesJL.et alEffects of age, sex, and ethnicity on the association between apolipoprotein E genotype and Alzheimer disease. A meta-analysis.JAMA.199727816134913569343467
- AppelrosP.StegmayrB.TereA.Sex differences in stroke epidemiology: a systematic review.Stroke.2009401082109019211488
- NelsonPT.SchmittFA.JichaGA.et alAssociation between male gender and cortical Lewy body pathology in large autopsy series.J Neurol.2010257111875188120563821
- ElbazA.BowerJH.MaraganoreDM.et alRisk tables for parkinsonism and Parkinson's disease.J Clin Epidemiol.2002551253111781119
- ElbazA.et alSurvival study of Parkinson disease in Olmsted County, Minnesota.Arch Neurol.2003601919612533094
- GilliesGE.PienaarIS.VohraS.QamhawiZ.Sex differences in Parkinson's disease.Front Neuroendocrinol.201435337038424607323
- AugustineEF.PérezA.DhallR.et alSex differences in clinical features of early, treated Parkinson's disease.PLoS One.2015107e013300226171861
- LangaKM.FosterNL.LarsonEB.Mixed dementia: emerging concepts and therapeutic implications.JAMA.2004292232901290815598922
- MassoudF.DeviG.SternY.et alA clinicopathological comparison of community-based and clinic-based cohorts of patients with dementia.Arch Neurol.199956111368137310555657
- KnappM.PrinceM.AlbaneseE.et alDementia UK: The Full Report. London, UK: Alzheimer's Society; 2007.
- Martin-LáezR.Caballero-ArzapaloH.Valle-SanRomán N.López-MenéndezLÁ.Arango-LasprillaJC.Vázquez-BarqueroA.Incidence of idiopathic normal-pressure hydrocephalus in northern Spain.World Neurosurg.20168729831026548835
- SirajS.An overview of normal pressure hydrocephalus and its importance: how much do we really know?J Am Med Dir Assoc.20111211921
- MercyL.HodgesJR.DawsonK.BarkerR.BrayneC.Incidence of early-onset dementias in Cambridgeshire, United KingdomNeurology.200871191496149918981371
- BernardiL.FrangipaneF.SmirneN.et alEpidemiology and genetics of frontotemporal dementia: a door-to-door survey in Southern Italy.Neurobiol Aging.201233122948.e12948.e10
- OnyikeCU.Diehl-SchmidJ.The epidemiology of frontotemporal dementia.Int Rev Psychiatry.201325213013723611343
- GubbelsS.BacciS.LaursenH.et alDescription and analysis of 12 years of surveillance for Creutzfeldt-Jakob disease in Denmark, 1997 to 2008.Euro Surveill.20121715pii20142
- PrinceM.WimoA.GuerchetMAliGCWuYT.PrinaM.Alzheimer's Disease International. World Alzheimer Report 2015: The Global Impact of Dementia: an Analysis of Prevalence, Incidence, Cost and Trend. Available at: https://www.alz.co.uk/research/world-report-2015. Accessed July 2016.
- ArnoldAP.The organizational-activational hypothesis as the foundation for a unified theory of sexual differentiation of all mammalian tissues.Horm Behav.200955557057819446073
- KonkleAT.McCarthyMM.Developmental time course of estradiol, testosterone, and dihydrotestosterone levels in discrete regions of male and female rat brain.Endocrinology.2011152122323521068160
- SchwarzJM.McCarthyMM.Steroid-induced sexual differentiation of the developing brain: multiple pathways, one goal.J Neurochem.200810551561157218384643
- JoelD.McCarthyMM.Incorporating sex as a biological variable in neuropsychiatric research: where are we now and where should we be?Neuropsychopharmacology. 2016 Jun 22. Epub ahead of print.
- JoelD.BermanZ.TavorI.et alSex beyond the genitalia: the human brain mosaic.Proc Natl Acad Sci U S A.201511250154681547326621705
- FelittiVJ.AndaRF.NordenbergD.et alRelationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the adverse childhood experiences (ACE) study.Am J Prev Med.19981442452589635069
- XuW.TanL.WangHF.et alEducation and risk of dementia: dose-response meta-analysis of prospective cohort studies.Mol Neurobiol.20165353113312325983035
- MortamaisM.PortetF.BrickmanAM.et alEducation modulates the impact of white matter lesions on the risk of mild cognitive impairment and dementia.Am J Geriatr Psychiatry.201422111336134524021219
- CarcaillonL.Brailly-TabardS.AncelinML.et alLow testosterone and the risk of dementia in elderly men: impact of age and education.Alzheimers Dement.2014105 supplS306S31424035146
- SatterthwaiteTD.ConnollyJJ.RuparelK.et alThe Philadelphia Neurodevelopmental Cohort: a publicly available resource for the study of normal and abnormal brain development in youth.Neuroimage.2016124pt B1115111925840117
- HamelE.Cerebral circulation: function and dysfunction in Alzheimer's disease.J Cardiovasc Pharmacol.201565431732425384195
- TodaN.AyajikiK.OkamuraT.Cerebral blood flow regulation by nitric oxide in neurological disorders.J Physiol Pharmacol.2009878581594
- SatterthwaiteTD.ShinoharaRT.WolfDH.et alImpact of puberty on the evolution of cerebral perfusion during adolescence.Proc Natl Acad Sci U S A.2014111238643864824912164
- SatterthwaiteTD.VandekarS.WolfDH.et alSex differences in the effect of puberty on hippocampal morphology.J Am Acad Child Adolesc Psychiatry.201453334135024565361
- WilsonRS.SegawaE.BoylePA.AnagnosSE.HizelLP.BennettDA.The natural history of cognitive decline in Alzheimer's disease.Psychol Aging.20122741008101722946521
- MielkeMM.VemuriP.RoccaWA.Clinical epidemiology of Alzheimer's disease: assessing sex and gender differences.Clin Epidemiol.20146374824470773
- Alzheimer's Association. 2015 Alzheimer's disease facts and figures.Alzheimers Dement201511333238425984581
- LinFC.ChuangYS.HsiehHM.et alEarly statin use and the progression of Alzheimer disease: a total population-based case-control study.Medicine (Baltimore).20159447e214326632742
- KimS.KimMJ.KimS.et alGender differences in risk factors for transition from mild cognitive impairment to Alzheimer's disease: a CREDOS study.Compr Psychiatry.20156211412226343475
- SinforianiE.CitterioA.ZucchellaC.et alImpact of gender differences on the outcome of Alzheimer's disease.Dement Geriatr Cogn Disord.20103014715420733307
- LawsKR.IrvineK.GaleTM.Sex differences in cognitive impairment in Alzheimer's disease.World J Psychiatry.201661546527014598
- HebertLE.WeuveJ.ScherrPA.EvansDA.Alzheimer disease in the United States (2010-2050) estimated using the 2010 census.Neurology.201380191778178323390181
- KuaEH.HoE.TanHH.TsoiC.ThngC.MahendranR.The natural history of dementia.Psychogeriatrics.201414319620125323961
- BurnsA.LewisG.JacobyR.LevyR.Factors affecting survival in Alzheimer's disease.Psychol Med.19912123633701876641
- ToddS.BarrS.RobertsM.PassmoreAP.Survival in dementia and predictors of mortality: a review.Int J Geriatr Psychiatry.201328111109112423526458
- WattmoC.LondosE.MinthonL.Response to cholinesterase inhibitors affects lifespan in Alzheimer's disease.BMC Neurol.20141417325213579
- AltmannA.TianL.HendersonVW.GreiciusMD.Alzheimer's Disease Neuroimaging Initiative Investigators. Sex modifies the APOE-related risk of developing Alzheimer disease.Ann Neurol.201475456357324623176
- PanzaF.FrisardiV.SeripaD.et alAlcohol consumption in mild cognitive impairment and dementia: harmful or neuroprotective?Int J Geriatr Psychiatry.201227121218123822396249
- SolfrizziV.FrisardiV.CapursoC.et alModerate alcohol consumption, apolipoprotein E, and neuroprotection.Arch Neurol.200966454154219364947
- ClaxtonA.BakerLD.WilkinsonCW.et alSex and ApoE genotype differences in treatment response to two doses of intranasal insulin in adults with mild cognitive impairment or Alzheimer's disease.Am J Alzheimers Dis.2013354789797
- HaywoodWM.Mukaetova-LadinskaEB.Sex influences on cholinesterase inhibitor treatment in elderly individuals with Alzheimer's disease.Am J Geriatr Pharmacother.20064327328617062329
- ShelineYl.WestT.YarasheskiK.et alAn antidepressant decreases CSF A production in healthy individuals and in transgenic AD mice.Sci Transl Med.20146236236re4
- MakiPM.HendersonVW.Hormone therapy, dementia, and cognition: the Women's Health Initiative 10 years on.Climacteric.201215325626222612612
- ShanmughanS.EppersonCN.Estrogen and the prefrontal cortex: towards a new understanding of estrogen's effects on executive function.Human Brain Mapping.201435384786523238908
- HaraY.WatersEM.McEwenBS.MorrisonJH.Estrogen effects on cognitive and synaptic health over the lifecourse.Physiol Rev.201595378580726109339
- BaileyME.WangAC.HaoJ.et alInteractive effects of age and estrogen on cortical neurons: implications for cognitive aging.Neuroscience.201119114815821664255
- GurneyEP.NachtigallMJ.NachtigallLE.NaftolinF.The Women's Health Initiative trial and related studies: 10 years later: a clinician's view.J Steroid Biochem Mol Biol.201414241124172877
- BrintonRD.The healthy cell bias of estrogen action: mitochondrial bioenergeticsand neurological implications.Trends Neurosci.2008311052953718774188
- DanielJM.WittyCF.RodgersSP.Long-term consequences of estrogens administered in midlife on female cognitive aging.Horm Behav.201574778525917862
- AuA.FeherA.McPheeL.JessaA.OhS.EinsteinG.Estrogens, inflammation and cognition.Front Neuroendocrinol.2016408710026774208
- VegetoE.BenedusiV.MaggiA.Estrogen anti-inflammatory activity in brain: a therapeutic opportunity for menopause and neurodegenerative diseases.Front Neuroendocrinol.200829450751918522863
- LinJ.KroenkeCH.EpelE.et alGreater endogenous estrogen exposure is associated with longer telomeres in postmenopausal women at risk for cognitive decline.Brain Res.2011137922423120965155
- LiR.CuiJ.ShenY.Brain sex matters: estrogen in cognition and Alzheimer's disease.Mol Cell Endocrinol.20143891-2132124418360
- HanamsagarR.BilboSD.Sex differences in neurodevelopmental and neurodegenerative disorders: focus on microglial function and neuroinflammation during development.J Steroid Biochem Mol Biol.201616012713326435451
- HallJR.WiechmannAR.JohnsonLA.et alBiomarkers of vascular risk, systemic inflammation and microvascular pathology and neuropsychiatric symptoms in Alzheimer's disease.J Alzheimers Dis.201335236337123403534
- PetersonBL.WonS.GeddesRl.SayeedI.SteinDG.Sex-related differences in effects of progesterone following neonatal hypoxic brain injury.Behav Brain Res.201528615216525746450
- DeakT.QuinnM.CidlowskiJA.VictoriaNC.MurphyAZ.SheridanJF.Neuroimmune mechanisms of stress: sex differences, developmental plasticity, and implications for pharmacotherapy of stress-related disease.Stress.201518436738026176590
- HolmesC.Review: systemic inflammation and Alzheimer's disease.Neuropathol Appl Neurobiol.2013391516823046210
- GorelickPB.et alVascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the American Heart Association/ American Stroke Association.Stroke.20114292672271321778438
- SeshadriS.BeiserA.Kelly-HayesM.et alThe lifetime risk of stroke: estimates from the Framingham Study.Stroke.20063734535016397184
- ChengEY.KongMH.Gender differences of thromboembolic events in atrial fibrillation.Am J Cardiol.201611761021102726923085
- DufouilC.SeshadriS.ChêneG.Cardiovascular risk profile in women and dementia.J Alzheimers Dis.201442suppl 4S353S36325351109
- ChatterjeeS.PetersSA.WoodwardM.et alType 2 diabetes as a risk factor for dementia in women compared with men: a pooled analysis of 2.3 million people comprising more than 100,000 cases of dementia.Diabetes Care.201639230030726681727
- PendleburyST.RothwellPM.Prevalence, incidence, and factors associated with pre-stroke and post-stroke dementia: a systematic review and meta-analysis.Lancet Neurol.20098111006101819782001
- GladerE.StegmayrB.NorrvingB.et alSex differences in management and outcome after stroke: a Swedish national perspective.Stroke.20033481970197512855818
- PerryRH.IrvingD.TomlinsonBE.Lewy body prevalence in the aging brain: relationship to neuropsychiatric disorders, Alzheimer-type pathology and catecholaminergic nuclei.J Neurol Sci.19901001-22232331965207
- HeidebrinkJL.Is dementia with Lewy bodies the second most common cause of dementia?J Geriatr Psychiatry Neurol.20021518218712489913
- VannJones SA.O'BrienJT.The prevalence and incidence of dementia with Lewy bodies: a systematic review of population and clinical studies.Psychol Med.201444467368323521899
- SavicaR.GrossardtBR.BowerJH.BoeveBF.AhlskogJE.RoccaWA.Incidence of dementia with Lewy bodies and Parkinson disease dementia.JAMA Neurol.201370111396140224042491
- BootBP.OrrCF.AhlskogJE.et alRisk factors for dementia with Lewy bodies: a case-control study.Neurology.201381983384023892702
- RossoSM.LandweerEJ.HoutermanM.DonkerKaat L.vanDuijn C.vanSwieten J.Medical and environmental risk factors for sporadic frontotemporal dementia: a retrospective case-control study.J Neurol Neurosurg Psychiatry.200374111574157614617722
- KnopmanDS.PetersenRC.EdlandSD.ChaRH.RoccaWA.The incidence of frontotemporal lobar degeneration in Rochester, Minnesota, 1990 through 1994.Neurology.200462350650814872045
- Garre-OlmoJ.GenisBatlle D.del MarFernández M.et alIncidence and subtypes of early-onset dementia in a geographically defined general population.Neurology.201075141249125520810999
- RossoSM.KaatL.BaksT.JoosseM.Frontotemporal dementia in the Netherlands: patient characteristics and prevalence estimates from a population-based study.Brain.2003126pt 92016202212876142
- SeelaarH.RohrerJD.PijnenburgYA.et alClinical, genetic and pathological heterogeneity of frontotemporal dementia: a review.J Neurol Neurosurg Psychiatry.201182547648620971753
- SeltmanRE.MatthewsBR.Frontotemporal lobar degeneration: epidemiology, pathology, diagnosis and management.CNS Drugs.2012261084187022950490
- JellingerKA.Pathology and pathogenesis of vascular cognitive impairment—a critical update.Front Aging Neurosci.201351723596414
- GearingM.MirraSS.HedreenJC.SurniSM.Han-senLA.HeymanA.The consortium to establish a registry for Alzheimer's disease (CERAD). Part X. Neuropathology confirmation of the clinical diagnosis of Alzheimer's disease.Neurology.1995453 pt 14614667898697
- WhiteLR.EdlandSD.HemmyLS.et alNeuropathologic comorbidity and cognitive impairment in the Nun and Honolulu-Asia Aging Studies.Neurology.201686111000100826888993
- AbdelnourC.vanSteenoven I.LondosE.et alAlzheimer's disease cerebrospinal fluid biomarkers predict cognitive decline in Lewy body dementia.Mov Disord.20163181203120827296778
- GjerstadMD.Wentzel-LarsenT.AarslandD.LarsenJP.Insomnia in Parkinson's disease: frequency and progression over time.J Neurol Neurosurg Psychiatry.200778547647917098844
- HaaxmaCA.et alGender differences in Parkinson's disease.J Neurol Neurosurg Psychiatry.200778881982417098842
- MillerIN.Cronin-GolombA.Gender differences in Parkinson's disease: clinical characteristics and cognition.Mov Disord.201025162695270320925068
- ShulmanLM.BhatV.Gender disparities in Parkinson's disease.Expert Rev Neurother.20066340741616533144
- Martinez-MartinP.FalupPecurariu C.OdinP.et alGender-related differences in the burden of non-motor symptoms in Parkinson's disease.J Neurol.201225981639164722237822
- LouisED.MarderK.CoteL.et alMortality from Parkinson's disease.Arch Neurol.1997542602649074394
- BreanA.EidePK.Prevalence of probable idiopathic normal pressure hydrocephalus in a Norwegian population.Acta Neurol Scand.20081181485318205881
- SilverbergGD.MayoM.SaulT.RubensteinE.McGuireD.Alzheimer's disease, normal-pressure hydrocephalus, and senescent changes in CSF circulatory physiology: a hypothesis.Lancet Neurol.20032850651112878439
- JarajD.AgerskovS.RabieiK.et alVascular factors in suspected normal pressure hydrocephalus: a population-based study.Neurology.201686759259926773072
- NimbiwalBK.JalandhraMK.MonishS.SanjeevT.Prion protein as a pathogen: a review.UBAR.201237531536
- SkillbäckT.RosénC.AsztelyF.MattssonN.BlennowK.ZetterbergH.Diagnostic performance of cerebrospinal fluid total tau and phosphorylated tau in Creutzfeldt-Jakob disease: results from the Swedish Mortality Registry.JAMA Neurol.201471447648324566866
- BaumanAE.ReisRS.SallisJF.WellsJC.LoosRJ.MartinBW.Lancet Physical Activity Series Working Group. Correlates of physical activity: why are some people physically active and others not?Lancet.2012380983825827122818938
- PaveyT.TaylorA.HillsdonM.et alLevels and predictors of exercise referral scheme uptake and adherence: a systematic review.J Epidemiol Community Health.201266873774422493474
- SegarMJ.UpdegraffJA.Zikmund-FisherBJ.RichardsonCR.Physical activity advertisements that feature daily well-being improve autonomy and body image in overweight women but not men.J Obes.2012201235472122701782
