Abstract
Wilson disease is a rare genetic disease causing pathologic deposition of copper in the liver, brain, cornea, kidney, and cardiac muscles. Presented are two cases of neurologic Wilson disease with progressive movement disorder and Kayser-Fleischer rings with low serum copper, low ceruloplasmin, and increased 24-hour urine copper against a background of normal transaminases. Cranial imaging revealed symmetric basal ganglia hyperintensities in T2/FLAIR. More often than not, these cases go unnoticed and misdiagnosed because of its rarity and varied presentation. Extensive workup is necessary to confirm the diagnosis. As for management, the earlier the intervention is initiated, the better prognosis would be for recovery. There are several treatment options which should be tailored to every patient with neurologic Wilson disease. Neurologic Wilson disease is considered as a copper toxicity; immediate diagnostic evaluation and early treatment initiation is a must.
La Enfermedad de Wilson es una enfermedad genética rara provocada por un depósito patológico de cobre en el hígado, cerebro, córnea, riñón y músculo cardíaco. Se presentan dos casos de Enfermedad de Wilson neurológica con trastorno progresivo del movimiento y anillos de Kayser-Fleischer con cobre y ceruloplasmina séricos bajos, y aumento de cobre en orina de 24 horas, con transaminasas normales. Las imágenes craneales revelan hiperintensidad simétrica en T2/FLAIR de los ganglios basales. Lo más frecuente es que estos casos pasen inadvertidos o no se realice el diagnóstico correcto debido a la rareza y variedad de sus presentaciones. Se require de un completo trabajo para poder precisar el diagnóstico. Respecto al manejo, cuanto antes se inicie la intervención, mejor será el pronóstico para la recuperación. Existen diversas opciones terapéuticas y deben adaptarse a cada paciente con Enfermedad de Wilson neurológica. La Enfermedad de Wilson neurológica se considera una toxicidad al cobre, por lo que es una necesidad la evaluación diagnóstica inmediata y el tratamiento precoz.
La maladie de Wilson est une maladie génétique rare qui provoque un dépôt de cuivre pathologique dans le foie, le cerveau, la cornée, le rein et le muscle cardiaque. Nous présentons deux cas de maladie de Wilson dans sa forme neurologique avec un trouble kinétique progressif et des anneaux de Kayser-Fleischer, avec une hypocuprémie, une hypocéruloplasminémie et une hypercuprurie des 24 h, les transaminases étant normales. L'IRM cérébrale montre des hypersignaux symétriques en FLAIR et T2 des ganglions de la base. Le plus souvent ces cas ne sont pas diagnostiqués et passent inaperçus en raison de la rareté et de la présentation variée de la maladie. Un bilan approfondi est nécessaire pour établir le diagnostic. De même que pour la prise en charge, plus tôt le traitement est instauré, meilleur est le pronostic de guérison. Plusieurs options de traitement sont disponibles qui doivent être adaptées à chaque patient atteint de la maladie de Wilson. La maladie de Wilson sous sa forme neurologique est considérée comme une toxicité au cuivre ; elle nécessite une évaluation diagnostique immédiate et un traitement précoce.
Introduction
In 1912, a British neurologist, Samuel Wilson, described a neurologic disorder with pathologic findings of degeneration of the lenticular nucleus in the brain and hepatocytes in the liver. It was then called progressive hepatolenticular degeneration, better known by its eponym, Wilson disease (WD).Citation1,Citation2,Citation4
WD is attributed to a rare autosomal recessive genetic defect on ATP7B, a metal-transporting P-type adenosine triphosphate on chromosome 13ql4.3. Deficiency or absence of the transporter protein results in decreased biliary excretion of copper and thereby excessive deposition of copper in the liver, central nervous system, cornea, kidney, and cardiac muscles.Citation3
WD has a prevalence rate of 15 to 30 cases per million, qualifying as a rare disease based on the criterion of European Commission on Public Health and Institute of Human Genetics.Citation4
The manifestations of WD are more likely to be hepatic in early childhood, and neurologic in adolescents and young adults. WD has varied presentations, classified into three movement disorder syndromes:
Dystonia (dystonic postures and choreoathethosis)
Ataxia (ataxia with postural and intentional tremors)
Parkinsonian symptoms (hypokinesia, rigidity, and resting tremors)Citation2
Emphasis should be given to reviewing vignettes, diagnostics, and treatment of patients in order to catch these rare conditions early and subsequently initiate treatment. We present two vignettes of WD.
Clinical vignettes
Case 1
A 20-year-old female presented with 12-month history of slowing of movement and difficulty writing legibly, with occasional reports of postural tremors, right more than the left and blurring of vision. She developed slurring of speech and involuntary hand movements.
Pertinent neurologic examination revealed a Mini-Mental Status Examination (MMSE) score of 29/30, with deficit in attention and choreiform movements in upper and lower extremities coupled with athetoid movements of the hands. Classic wing-beating tremors were observed in the right arm. On passive range of motion, there was mild rigidity, right more than the left, and bradykinesia noted on rapid fine movements of fingers. Generalized hyperreflexia and tendency to fall backward on walking were observed.
Case 2
A 21-year-old female presented initially with spontaneous abortion, and then had slurring of speech and stiffness of the jaw, with occasional reports of cramps of facial muscles. She then developed tremors and stiffening of right extremities, which progressed to involve the contralateral side with accompanying weakness over a span of 18 months. Over the succeeding 4 months, there was progression of stiffness causing posturing of legs and difficulty ambulating, and worsening kinetic tremors. There were also episodes of freezing of gait and uncontrolled grin.
Relevant neurologic findings were: MMSE of 27/28, with deficit in recall. Poor gutturals and tongue fasciculations were noted on cranial nerve examination. There was marked atrophy of the intrinsic muscles of the hand and posterior leg muscles with paradoxical hypertrophy of triceps and quadriceps. Dystonic inversion posturing of both feet was notable on walking. The patient also had generalized rigidity and kinetic tremors, more prominent on the right than the left.
Diagnostic workup
The two cases were worked up for WD and can be classified differently; the first case falls into the ataxic type with parkinsonian symptoms and the second case fits the dystonic with parkinsonian symptoms (Table I).Citation5,Citation6
TABLE I. Clinical vignette summary; Wilson disease phenotypic classification; unified Wilson's Disease Rating Scale (UWDRS).
Both of the patients were subjected to slit-lamp examination revealing the presence of Kayser-Fleischer rings . A complete hepatic workup was done, revealing normal liver function: transaminases and clotting factors but with gross structural abnormalities noted on sonography (Table II). Diagnostic workup for copper accumulation revealed low serum copper, low ceruloplasmin, and increased urinary excretion of copper.Citation7,Citation8,Citation9 Citation10 Genetic testing was not done on these patients.

8th International Meeting on Wilson Disease Scoring System (Leipzig Score)
TABLE II. Diagnostic examination summary; 8th International Meeting on Wilson disease scoring system.
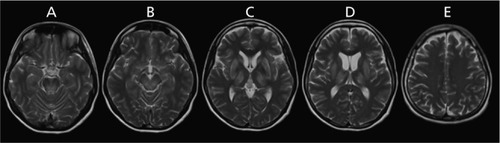
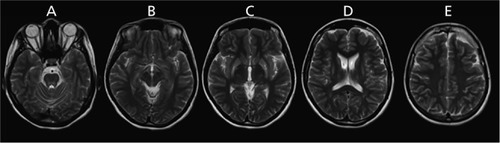
Magnetic resonance imaging of the brain did not reveal the typical double panda sign but showed symmetrical T2/FLAIR hyperintensities over the putamen, caudate and thalami nucleus ( and .Citation11,Citation12 Both findings were highly suggestive of mineral deposition. Furthermore, following the scoring by Leipzig et al, the two vignettes are definite cases of WD.Citation8,Citation13,Citation16
Because of the rarity of the disease, it is not cost-effective to initiate population-based screening. Screening however should be compulsory for patients presenting with unexplained neurological disease with or without associated liver disease. WD must be distinguished from mimickers such as essential tremor, young-onset Parkinson's disease, generalized dystonia, and other rare movement disorders like Huntington disease, Hallervorden-Spatz disease, idiopathic torsion dystonia, chorea-acanthocytosis and benign familial chorea. WD is therefore a diagnostic emergency, needing a complete and immediate workup.Citation2
Management
As for the treatment, definitive treatment includes liver transplantation, especially for those with acute hepatitis or fulminant hepatic failure. For those with serious and debilitating neurologic sequelae, the best option is either to increase urinary excretion of cooper directly ie, D-penicillamine and trientine or block gastrointestinal absorption of copper ie, zinc acetate/salts and tetrathiomolybdate (Table III).Citation14,Citation15,Citation16,Citation17
TABLE III Summary of treatment options for neurologic Wilson disease.
For both cases, low copper diet was a mainstay of treatment. Zinc supplementation was also initiated, with subsequent noting of remarkable improvements in speech, tremors, and stiffening of extremities. The first case underwent D-penicillamine treatment with slow uptitration of the drug to avoid hematologic consequences and to monitor for paradoxical neurological deterioration. As for the second case, the patient was maintained on zinc supplementation because of relatively severe baseline neurologic status and high risk for paraxodical neurologic worsening. Treatment should still be individualized since no two patients with WD are the same.Citation8,Citation15,Citation16
For patients with debilitating movement disorder refractory to chelation and medical treatment, botulinum toxin injection may be offered. Screening of siblings of the patient and monitoring of their serum ceruloplasmin is also a big part of management.Citation18 Early intervention signifies better prognosis, thus can be considered as a therapeutic emergency as well.
Synthesis
Educating medical doctors about this neurologic condition and having a high index of suspicion can improve treatment of this debilitating condition. Familiarization of this rare genetic condition may also pave the way for future research to ascertain the prevalence, to facilitate detection, and to improve outcomes.
Dr Porlas, Dr de Castillo, and Dr Dioquino have nothing to disclose.
REFERENCES
- WalsheJM.History of Wilson disease: a personal account. In: Czlonkowska A, Schilsky ML, eds.Handbook of Clinical Neurology. Volume 142 (3rd series), Amsterdam, the Netherlands: Elsevier;2017.
- LorinczMT.Neurologic Wilson's disease.Ann N Y Acad Sci. doi: 10.1111/J.1749-6632.2009.05109.x.20101184173187
- WuF.WangJ.PuC.QiaoL.JiangC.Wilson's disease: a comprehensive review of the molecular mechanisms.Int J Mol Sci. doi:10.3390/ijms16036419.201516364196431
- MakCM.LamCW.Diagnosis of Wilson's disease: a comprehensive review.Crit Rev Clin Lab Sci. doi: 10.1080/10408360801991055.2008453263290
- VolpertHM.PfeiffenbergerJ.GrönerJB.StremmelW.GotthardtDN.SchäferM.WeissKH.WeilerM.Comparative assessment of clinical rating scales in Wilson's disease.BMC Neurol. doi: 10.1186/ S12883-017-0921-3.2017171140
- CzlonkowskaA.TarnackaB.MöllerJC.et al.Unified Wilson's Disease Rating Scale — a proposal for the neurological scoring of Wilson's disease patients.Neurol Neurochir Pol.200741111217330175
- BandmannO.WeissKH.KalerSG.Wilson's disease and other neurological copper disorders.Lancet Neurol. doi:10.1016/ S1474-4422(14)70190-5.2015141103113
- Rodriguez-CastroKl.Hevia-UrrutiaFJ.SturnioloGC.Wilson's disease: A review of what we have learned.World J Hepatol. doi: 10.4254/wjh.v7.i29.2859.201572928592870
- AlaA.WalkerAP.AshkanK.DooleyJS.SchilskyML.Wilson's disease.Lancet.2007369955939740817276780
- MediciV.RossaroL.SturnioloGC.Wilson Disease — A practical approach to diagnosis, treatment and follow-upDig Liver Dis.20073960160917382611
- CzlonkowskaA.LitwinT.ChabikG.Wilson's disease — neurologic features. In: Cztonkowska A, Schilsky ML, eds.Handbook of Clinical Neurology. Volume 142 (3rd series), Amsterdam, the Netherlands: Elsevier;2017.
- CetlinRS.RodriguesGR.Pena-PereiraMA.OliveiraDS.SouzaCP.TumasV.Teaching video neuroimages: excessive grinning in Wilson disease.Neurology. doi: 10.1212/WNL.0b013e3181bacef0.20097314e73
- FerenciP.CacaK.LoudianosG.Mieli-VerganiG.TannerS.SternliebI.SchilskyM.CoxD.BerrF.Diagnosis and phenotypic classification of Wilson disease.Liver Int.200323313914212955875
- BrewerGJ.Wilson's Disease. In: Frucht SJ, ed.Movement Disorder Emergencies: Diagnosis and Treatment Totowa, NJ: Human Press2013.
- BrewerGJ.Zinc acetate for the treatment of Wilson's disease.Exp Opin Pharmacother. https://doi.org/ 10.1517/14656566.2.9.1473.20012914731477
- BrewerGJ.HillGM.PrasadAS.CossackST.RabbaniP.Oral zinc therapy for Wilson's Disease.Ann Intern Med. https://doi.org/ 10.7326/0003-4819-99-3-314.1983993314320
- BrewerGJ.Zinc and tetrathiomolybdate for the treatment of Wilson's disease and the potential efficacy of anticopper therapy in a wide variety of diseases.Metallomics. doi: 10.1039/ b901614g.200913199206
- European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Wilson's Disease.J Hepatol. https://doi. org/10.1016/j.jhep.2011.11.007. 563671685
