Abstract
Managing complications after attempted hind foot and ankle arthrodesis with intramedullary nail fixation is a challenge. This situation becomes more problematic in the patient with diabetes mellitus and multiple comorbidities. Infection and subsequent osteomyelitis can be a devastating, limb threatening complication associated with these procedures. The surgeon must manage both the infectious process and the skeletal instability concurrently. This article provides a literature review and detailed management strategies for a modified technique of employing antibiotic impregnated polymethylmethacrylate-coated intramedullary nailing.
The use of an intramedullary (IM) nail is a valuable tool in the armamentarium of the foot and ankle surgeon, in particular for salvage procedures of the complicated diabetic patient. Successful tibiotalocalcaneal (TTC) arthrodesis implementing IM nails are described in the literature Citation1 Citation2 Citation3 Citation4 Citation5 Citation6 Citation7 Citation8 . In addition, the utilization of IM nails has been shown to be an effective option when dealing with management of distal tibial fractures, cited frequently in the orthopedic literature Citation9 Citation10 Citation11 Citation12 Citation13 Citation14 Citation15 Citation16 .
Infection is a major complication encountered with the use of IM nails. IM nailing of closed tibial fractures has an associated infection rate of approximately 1% (16). The infection rate is expected to be significantly higher in those patients undergoing reconstructive TTC arthrodesis attempts, especially in those patients with complicated diabetes mellitus Citation17. Due to the nature and anatomic location of IM nails, post-operative infections are often limb-threatening Citation18. Deep-seeded IM infections may be the result of bacteria's ability to remain on the surface of the implant, protected from antibiotic and immune system attacks in biofilms Citation19. Other complications of this procedure include delayed union, mal-union, and nonunion (1–8). Failure of the achievement of osseous union across the arthrodesis site is often paired with infection and commonly the two problems must be managed concurrently.
Failure in the management of an IM infection and nonunion often ends in limb loss. Amputation has dramatic effects on the quality of life and overall life expectancy of the patient Citation20. Understanding how to manage infection following IM nail implantation is imperative. One should not attempt IM nailing if they are not prepared to deal with this potentially devastating complication. This review article focuses on the current techniques described for IM infection management following IM nail application in diabetic limb salvage.
Infection control
In the presence of clinical signs and symptoms of infection following IM nail implantation, management of the infection from both a medical and surgical perspective is vital. Any wounds showing clinical signs of infection should be cultured and sent for Gram stain and antibiotic sensitivity. The patient should be placed on broad-spectrum intravenous antibiotics until the responsible organism is identified. Medical stabilization of the patient is very important, as many patients undergoing these procedures have multiple medical comorbidities in addition to their diabetes. Radiological studies, including plain film radiographs and/or computed tomography, should be obtained for correlation with clinical symptoms as well as surgical planning. Next, the patient should be taken to the operating room following medical clearance for removal of the IM nail and debridement of the IM canal, infected soft tissue, and other areas of osseous involvement (9–14). Soft tissue resection margins should be bleeding viable tissue with no evidence of remaining necrotic tissue. Debridement of the IM canal consists of utilizing an IM reamer approximately 1–2 mm larger in diameter than the IM nail that was removed. This is paired with a powered pulse-lavage irrigation using at least nine liters of saline (9, 10). Debridement products and the removed IM nail should also be cultured and sent for deep intra-operative culture and sensitivity testing.
Following culture and sensitivity results, intravenous antibiotics should be modified for focused eradication of the responsible organisms. It is common for culture results to yield no growth, in which case the patient should remain on empiric antibiotic therapy. In most cases, this is due to the antibiotic treatment administered to the patient in the days preceding the surgical debridement (9, 10). Some authors advocate for the discontinuation of systemic antibiotics three days prior to surgical debridement to avoid false negative culture results (12). White blood cell (WBC) counts, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) laboratory levels are necessary to monitor the progression of infection resolution in the post-debridement period. It should be noted that WBC counts are often normal in patients with infected nonunions and chronic osteomyelitis, especially in the setting of immuno-suppressed hosts (18).
Delivery of local antibiotic therapy in the form of impregnated polymethylmethacrylate (PMMA) cement molded into the shape of an IM rod has become very popular (9, 10, 12–14). These materials are implanted in the operating room following the IM canal debridement and pulse-lavage irrigation.
Local antibiosis with temporary cemented intramedullary nail
The use of an antibiotic impregnated cement coated IM nail following IM infections following nailing of tibia and femur fractures has been well-documented in the literature (9, 10, 12–14, Citation21 Citation22 Citation23 ). The use of an antibiotic impregnated cement nail in dealing with IM infection provides many advantages over other surgical management options. The cement nail provides some stability across the arthrodesis site, unlike cement beads. It has been well established that osseous stability is important in the management of an infected nonunion and IM osteomyelitis (18, 22, 23). Second, cement nails have been shown to elute a high concentration of antibiotic in local sites for up to 36 weeks. This was shown to have a therapeutic effect on refractory infection and allow a higher concentration of antibiotic present locally with fewer associated side effects than is achievable with systemic antibiosis (21, 22). The disadvantage of this procedure is that at least two surgical procedures in the operating room will be necessary (14). Compliance with non-weight bearing orders remains important after placement of a temporary antibiotic-coated IM nail, as the stability provided by this procedure does not provide the stability necessary for safe weight bearing status. Additional fixation may be required with temporary antibiotic-coated rods if weight bearing is desired.
Antibiotic cement rod preparation
Following IM debridement and pulse lavage irrigation, the leg and foot should be re-prepped and re-draped. The surgical team should change gowns, gloves, and use new sterile instrumentation. A sterile chest tube with an inner diameter comparable to the outer diameter of the removed IM nail is cut to the length of the IM nail. An intra-substance support wire, such as a 3 mm IM guide wire with or without olives (9, 10) or an Ender nail (12) is selected, bent to mimic the shape of the removed IM nail, and cut approximately 5 cm longer than the chest tube. The proximal end of this support wire may be bent into a loop to allow easy retrieval at a later date. A mixture of PMMA and antibiotic powder is then performed. Specific mixtures used in the literature can be found in . Liquid monomer should then be added to allow the mixture to dissolve. Some authors advocate for the substance to be mixed via vacuum mixing technique. Once thoroughly mixed, the cement can be put into a sterile cement gun or large bore syringe and injected into the chest tube. The chosen intra-substance support wire is placed in the center of the chest tube. As the exothermic reaction of the cement mixture takes place, the rod will begin to increase in temperature and harden. The curing of the cement takes several minutes. After hardening occurs, the chest tube can be cut longitudinally and peeled away from the periphery of the cement. Once cooled, the antibiotic cement rod is ready to be inserted.
Table 1. Examples of antibiotic impregnated bone cement products
Antibiotic cement rod removal
Systemic signs of infection, wound appearance, WBC count, ESR, and CRP should all be monitored closely in the post-operative period. Once these laboratory values have returned to normal, associated wounds have healed, and no local or systemic signs of infection are noted, the patient can be taken back to the operating room for antibiotic rod removal. Antibiotic cement rod removal ranges from 6 to 107 weeks following implantation in the literature (9, 10, 12). This wide range is probably a reflection of the varying levels of osteomyelitis chronicity reported. It is important that the IM canal is reamed and soft tissue and osseous structures are sent for histopathological analysis a second time following cement rod removal. This may be the only reliable way to ensure that the infection has been eradicated (9).
Literature review
Qiang and colleagues (9) reported their results in 19 patients following infected nonunions status-post lower extremity fractures (13 tibias, 6 femurs) with mean follow-up of 16 months (range 6–28). Thirteen were open fractures and all underwent debridement and insertion of a temporary self-made antibiotic cement rod as described above. Cultures were positive for Staphylocccus aureus in eight patients and were negative for 11 patients despite obvious clinical signs of infection. All patients were receiving antibiotics at time of intra-operative cultures. The antibiotic rods were removed at an average of 57 days (range 35–123) following implantation. At the time of antibiotic rod removal, the IM canal was reamed a second time. Products of the reaming were sent for repeat culture. If evidence of infection remained based on clinical exam, laboratory findings, and/or culture results, the patient received repeated antibiotic rod implantation. Difficulty in retrieval of the antibiotic rod was experienced in two patients due to a broken rod and a rod too large in diameter, respectively. Both rods were removed successfully following bone fenestration, with the associated cost of resulting cortical defects. The authors suggested avoiding this complication by ensuring that the diameter of the cement rod is 2–3 mm smaller than the intramedullary canal, and re-reaming if necessary. No recurrent infections occurred in 18/19 cases. One patient underwent amputation due to infection that could not be controlled despite systemic and local antibiosis. Four patients achieved union without the use of further fixation. Thirteen patients underwent repeat permanent IM nailing once they were determined to be clear of infection. One patient underwent bone transport with external fixation for femoral defects. Eleven patients went on to achieve complete bone healing, six of the remaining patients achieved partial union and one patient experienced a nonunion.
Paley and Herzenberg (10) performed a retrospective analysis of IM infection following IM nailing in nine patients. Eight patients had undergone complex limb-lengthening and/or deformity correction procedures, with one patient being treated for a fracture (six femurs, two tibias, one humerus). Mean follow-up obtained was 40.9 months (range 32–48). Staphylococcus aureus was cultured on initial debridement in seven patients (five methicillin resistant and two methicillin sensitive), while cultures were negative in two patients despite clinical signs of infection. Both of these patients were on intravenous antibiotics at the time of culture. Four of the nine patients had recalcitrant nonunions, with each having undergone one or more attempts at failed revisions. All nine patients were prescribed functional removable braces to provide added stabilization in addition to the antibiotic cement rod. Cement rods were removed at an average of 164 days (range 29–753). Six of the nine patients had their temporary rods exchanged for permanent IM nail placement. One patient achieved solid union during treatment with the temporary rod, making additional internal fixation unnecessary. One patient who had a stiff asymptomatic nonunion of the humerus refused temporary rod removal. This patient experienced breakage of the rod two years post-operatively. Retrieval was attempted and was successful for the proximal half, but the distal half was left due to the patient's requests. No recurrent infections were noted in any of the patients. One rod was noted to be cracked at time of removal, however, no rods were broken and all were easily retrieved. The three nonunions treated with repeat nailing healed, with two requiring bone grafting. One patient that experienced an infected subtalar joint failed to achieve arthrodesis. This patient walked with an asymptomatic foot with the use of an ankle foot orthosis.
Sancineto and Barla (12) report their retrospective findings on 19 patients treated for both chronic and acute IM infection following lower limb shaft fractures (15 tibias, 4 femurs) treated with antibiotic cement rod placement. Follow-up ranged from 12 to 54 months, with no mean reported. Sixteen of the 19 patients had a nonunion in addition to the IM infection. The protocol described above was followed with negligible deviation. The offending organism was methicillin resistant Staphylococcus aureus in 17 of the 19 cases, with 26% being poly-microbial. The cement rod was removed ranging from 6 to 76 weeks, with no mean reported. One patient experienced a hypersensitivity reaction to vancomycin following cement rod implantation, necessitating early removal. This patient was the only subject to have positive cultures upon cement rod removal. Of the 16 patients who had nonunions, 12 patients had successful IM nailing performed following cement rod removal. One patient required bone transportation over the nail with an external fixator, while a second patient required cancellous bone graft mixed with vancomycin. Both were necessary to fill a bone defect. Two patients received cement-coated un-reamed tibial nails (UTN, Synthes, Oberdorf, Switzerland) in order to achieve union. No recurrent infections were noted in any of the patients who underwent the entire course of local antibiosis.
Local antibiosis with permanent cement-coated interlocking intramedullary nail
Thonse and Conway (14) present a novel approach to the surgical management of IM infections. Rather than placing a temporary antibiotic IM rod, the authors advocate for the placement of an interlocking IM nail that has an outer coating of antibiotic-impregnated PMMA. The goal of this technique is to provide antibiosis locally and permanent fixation with only one surgical procedure to the operating room required, as opposed to at least two as required with temporary cement rod placement. Debridement of the IM canal occurred as described above prior to preparation of the cement-coated interlocking IM nail. Their technique for IM nail preparation is described below. In their report, Thonse and Conway retrospectively shared their results of using this technique in 20 patients. Specific usage of the cement-coated interlocking IM nail varied with 4 patients undergoing ankle arthrodesis, four patients requiring revision of tibial nonunions, five patients receiving knee arthrodesis, and seven patients for revision of femoral nonunions. Control of infection was achieved in 95% (19/20) of the patients. The remaining patient in whom infection was not controlled underwent an above the knee amputation following intermittent wound discharge, despite achieving bony union. Bony union was achieved in 85% (17/20) of the patients. The remaining 15% (3/20) achieved a stable nonunion (one patient) and stable nonunion with the use of a cement spacer (two patients). Three out of 20 patients (15%) required exchange of the cement-coated interlocking IM nail due to continued infection. De-bonding of the cement from the nail occurred in all three patients who required nail exchanging in addition to a patient who requested that the nail be removed following achievement of bony union. The cement was removed with the use of a J-hook (Moreland Cemented Instruments; Depuy Orthopedics, Inc., Warsaw, IN) without complication. Half (10/20) of the patients did not require any additional procedures following placement of the cement-coated interlocking IM nail. One patient was lost to follow-up following achievement of infection control and a stable nonunion at 6 months. Infection had not recurred in the remaining 18 patients who achieved infection control at an average of 16 months (range 7–40 months) follow-up.
Cement-coated interlocking intramedullary nail preparation
On a sterile table, commercially available stainless steel molds (Biomet Inc., Warsaw, IN) were coated with a thin layer of lubricant gel. For tibial cases, the molds were 12 mm in width and were used in conjunction with a 10 mm nail. Powdered cement was then sprinkled onto the lubricant to allow for easy nail removal from the mold. For tibial nails, two batches of antibiotic-impregnated cement were mixed utilizing 1 gram of vancomycin, 3.6 grams of tobramycin, and 40 grams of PMMA. Liquid monomer was then added to allow mixing, followed by vacuum mixing technique. Once mixed, the cement was placed into each side of the mold using a cement gun while the mixture was in a liquid state. The interlocking IM nail was placed in one of the molds, ensuring that the proximal interlocking holes were not within the mold. The second mold was then placed on top of the remaining half of the interlocking IM nail. The cement was allowed to harden for approximately 8–10 min. The cement-covered IM nail can then be removed from the mold. Excess cement was then removed from the surface of the cement-coated nail using an osteotome. A file was also used to smooth the cement surface and create a bullet-shaped distal end of the nail.
Modified technique for permanent antibiotic impregnated intramedullary nail
Since these molds and large enough chest tubes are not commercially available to coat the IM nail, the senior author (PRB) has developed an alternative method for the insertion of a permanent antibiotic impregnated IM nail. Initially, the IM nail is roughed with a saw or other instrumentation to increase the adherence of the cement. The IM nail is then simply coated with cement by hand once it meets handling characteristics, with care to evenly spread the cement. As it hardens, it is rolled on the table to even distribution and overall shape. The interlocking screw holes are then cleared with a curette or similar instrumentation. The patient is then re-prepped, re-draped, and the surgical team is re-gowned to re-establish a sterile field.
The IM canal may then be reamed in preparation for the IM nail implantation. The authors suggest reaming the tibial canal 1.5 mm larger than the diameter of the IM nail to be implanted. Distally the calcaneus, talus and the distal part of the tibia, are reamed further, typically up to 15 mm. This accommodates both the IM nail and cement. If the more proximal tibia cannot be reamed enough to accommodate the IM nail and cement, the cement is only applied to the distal 2/3 of the IM nail. This still allows the antibiotic to be concentrated in the area most needed, near the ankle and hind foot where most infections and ulcerations have occurred in this patient population.
Once the cement is stable, the IM nail is inserted as usual with the use of the insertion jig. The IM nail may no longer accommodate the initial guide-wire used during the IM reaming process, so it should be removed before inserting the permanent antibiotic impregnated IM nail. The interlocking screws are placed in typical fashion. The wounds are closed, and a posterior splint is then applied. Non-weight bearing status is maintained until signs of radiographic union have occurred. As with most revisional or complicated arthrodesis cases in patients with diabetes, an estimated 8–10 weeks of non-weight bearing status may be required. The patients are then slowly transitioned to a removable surgical boot until clear signs of radiographic healing and clinical stability. This process is lengthy and can sometimes take up to 8–10 months for healing. Lower extremity orthosis and/or double upright bracing may be also necessary for permanent use on certain individuals ().
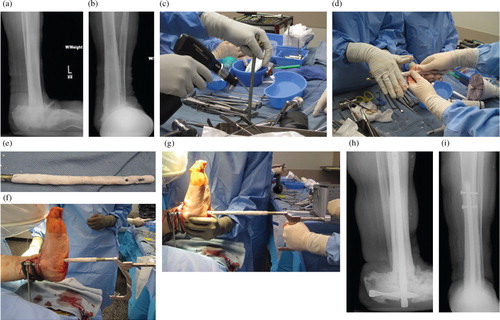
Fig. 1. Pre-operative radiographic views (A, B) showing an infected collapsed ankle and hind foot after a previous failed surgical attempt of tibiotalocalcaneal arthrodesis with an intramedullary (IM) nail. Intra-operative views showing the use of a large sagittal saw to create imperfections within the IM nail that allows increased adherence of the cement (C) and rolling of the antibiotic impregnated cement by hand onto the IM nail (D). The cement that covers the holes for the interlocking screws when placing the permanent antibiotic impregnated IM nail is removed (E). Insertion of the antibiotic coated IM nail using the insertion jig is showing in figure (F). Note that coating the IM nail with antibiotic cement precludes the use of the IM guide wire for a cannulated IM nail insertion (G). Final post-operative radiographic views (H, I) at one year follow-up. Note the density surrounding the IM nail within the tibial canal consistent with antibiotic cement..
Discussion
Significant ankle and hind foot deformities are not uncommon in the complicated diabetic patient. Implantation of both temporary and permanent antibiotic IM nails may be very useful procedures in diabetic limb salvage cases and especially in those patients with severe lower extremity infection, osteomyelitis and Charcot neuroathropathy. Because of the complexity associated with handling these types of procedures, they are frequently staged and fixation is often paired with adjunctive use of circular external fixation for further lower extremity stabilization and soft tissue management. Infectious disease consultation and appropriate medical management in this patient population is also necessary to ensure eradication of the infected lower extremity.
The techniques discussed in this paper can be utilized in the diabetic patient with active infection, but the use of permanent antibiotic-coated IM nailing may also be useful in cases with chronic or suspected infection, or in those with previous or current open wounds. For these indications, the antibiotic cement may be used to prevent devastating recurrence or stimulation of latent infection. Proper identification and management of IM infection in the pre-operative period, aggressive surgical debridement, and proper monitoring post-operatively is paramount for the patient's successful outcome.
Conclusion
The use of permanent antibiotic impregnated cement IM nail is a valuable tool in the armamentarium of the foot and ankle surgeon and has shown to be effective in dealing with these difficult diabetic salvage cases.
Conflict of interest and funding
The authors have received no funding or benefits from industry or elsewhere to conduct this literature review.
References
- Goebel M, Gerdesmeyer L, Mueckley T, Schmitt-Sody M, Diehl P, Stienstra J, et al.. Retrograde intramedullary nailing in tibiotalocalcaneal arthrodesis: a short-term, prospective study. J Foot Ankle Surg. 2006; 45: 98–106.
- Boobbyer GN. The long term results of ankle arthrodesis. Acta Orthop Scand. 1981; 52: 107–10.
- Miehlke W, Gschwend N, Rippstein P, Simmen BR. Compression arthrodesis of the rheumatoid ankle and hind foot. Clin Orthop Relat Res. 1997; 340: 75–86.
- Mueller EJ, Wick M, Muhr G. Chirurgische Therapie bei Inkongruenzen und Arthrosen am oberen Sprunggelenk. Orthopäde. 1999; 28: 529–37.
- Breitfuss H, Muhr G, Mönning B. Fixateur oder Schraube bei Arthrodesen am oberen Sprunggelenk. Unfallchirurg. 1989; 92: 245–53.
- Kile TA, Donnelly RE, Gehrke JC, Werner ME, Johnson KA. Tibiotalocalcaneal arthrodesis with an intramedullary device. Foot Ankle Int. 1994; 15: 669–73.
- Quill GE. Tibiotalocalcaneal arthrodesis. Tech Orthop. 1996; 11: 269–73.
- Stephenson KA, Kile TA, Graves SC. Estimating the insertion site during retrograde intramedullary tibiotalocalcaneal arthrodesis. Foot Ankle Int. 1996; 17: 781–2.
- Qiang Z, Jun PZ, Jie XJ, Hang L, Bing LJ, Cai LF. Use of antibiotic cement rod to treat intramedullary infection after nailing: preliminary study in 19 patients. Arch Orthop Trauma Surg. 2007; 127: 945–51.
- Paley D, Herzenberg JE. Intramedullary infections treated with antibiotic cement rods: preliminary results in nine cases. J Orthop Trauma. 2002; 16: 723–9.
- Richter D, Hanhn M, Laun R, Ekkernkamp A, Muhr G, Ostermann P. Arthrodesis of the infected ankle and subtalar joint: technique, indications, and results of 45 consecutive cases. J Trauma. 1999; 47: 1072–8.
- Sancineto CF, Barla JD. Treatment of long bone osteomyelitis with a mechanically stable intramedullar antibiotic dispenser: nineteen consecutive cases with a minimum of 12 months follow-up. J Trauma. 2008; 65: 1416–20.
- Madanagopal SG, Seligson D, Roberts CS. The antibiotic cement nail for infection after tibial nailing. Orthopedics. 2004; 27: 709–12.
- Thonse R, Conway J. Antibiotic cement-coated interlocking nail for the treatment of infected nonunions and segmental bone defects. J Orthop Trauma. 2007; 21: 258–68.
- Chan YS, Ueng SW, Wang CJ, Lee SS, Chen CY, Shin CH. Antibiotic-impregnated autogenic cancellous bone grafting is an effective and safe method for the management of small infected tibial defects: a comparison study. J Trauma. 2000; 48: 246–55.
- Blachut PA, O'Brien PJ, Meek RN, Broekhuyse HM. Interlocking intramedullary nailing with and without reaming for the treatment of closed fractures of the tibial shaft: a prospective, randomized study. J Bone Joint Surg Am. 1997; 79: 640–6.
- Wukich DK, Lowery NJ, McMillen RL, Frykberg RG. Post-operative infection rates in foot and ankle surgery: a comparison of patients with and without diabetes. J Bone Joint Surg Am. 2010; 92: 287–95.
- Patzakis MJ, Zalavras CG. Chronic posttraumatic osteomyeltis and infected nonunion of the tibia: current management concepts. J Am Acad Orthop Surg. 2005; 13: 417–27.
- Gristina AG, Costerton JW. Bacterial adherence to biomaterials and tissue. The significance of its role in clinical sepsis. J Bone Joint Surg Am. 1985; 67: 264–73.
- Lerner RK, Esterhai JL, Polomano RC, Cheatle MD, Heppenstall RB. Quality of life assessment of patients with posttraumatic fracture nonunion, chronic refractory osteomyelitis, and lower-extremity amputation. Clin Orthop Relat Res. 1993; 295: 28–36.
- Nelson CK, Hickmon SG, Harrison BH. Elution characteristics of gentamicin-PMMA beads after implantation in humans. Orthopedics. 1994; 17: 415–6.
- Nizegorodcew T, Palmieri G, Marzetti E. Antibiotic-coated nails in orthopedic and trauma surgery: state of the art. Int J Immunopathol Pharmacol. 2011; 24: 125–8.
- Riel RU, Gladden PB. A simple method for fashioning an antibiotic cement-coated interlocking intramedullary nail. Am J Orthop (Belle Mead NJ). 2010; 39: 18–21.