Abstract
Wound closure for the diabetic foot can be challenging and often involves amputation or reconstruction. The authors describe a surgical technique and a case report of lateral lesser toe fillet flap in the management of a diabetic foot wound. The lateral lesser toe fillet flap reconstruction is a reproducible technique that incurs comparatively minimal technical complexity and provides a favorable option in the management of diabetic foot wounds where soft tissue coverage is required.
Fillet flaps are axial pattern flaps harvested from non-functioning or unsalvageable osseous and soft tissue structures. They can then be used as a pedicle, island, or microvascular free flaps for reconstruction and are commonly used in the trauma setting (Citation1). Alpert and Buncke in 1978 were some of the first surgeons who described the concept of fillet flaps, where they treated mutilating hand injuries using a microvascular free flap from a non-replantable part for reconstruction (Citation1). The conventional fillet flap concept application has been extended to non-traumatic situations, such as defects caused by large pressure sores or by extensive tumor resection, where they are raised from anatomically intact limbs (Citation2–Citation5).
Open wounds caused by diabetic foot infections are commonly left to heal by secondary intention or by negative pressure wound therapy due to poor vascularity (Citation6). Fillet flap is one of the options for soft tissue closure in the diabetic foot either primarily or in staged reconstruction and depending on the patients’ vascular status. Advantages of the fillet flap include absence of donor-site morbidity, good durability, and leg length preservation, preventing the need for more proximal amputation for adequate soft tissue coverage. The clinical outcomes of fillet flap coverage for pressure wounds or selected amputations (forefoot and transmetatarsal) in diabetic patients have been proven to be reliable (Citation7–Citation9).
The purpose of this article was to describe the surgical technique of a lateral lesser toe fillet flap in the management of soft tissue closure in the diabetic foot.
Case report
A 26-year-old Indian shipyard worker with a history of poorly controlled diabetes mellitus (preoperative hemoglobin A1c of 11%) was admitted to the hospital with a 2-week history of left foot abscess without any prior history of trauma to the left foot. On physical examination, erythema and edema were noted over the plantar and dorsal aspect of the left foot. There was also a small abscess collection at the left fourth interspace foot region subcutaneously. The patient's hemoglobin level was 14 g/dL and his albumin level was 38 g/L. Dorsalis pedis and posterior tibial pulses were strongly palpable; however, Doppler ultrasound studies of the foot revealed suspicion of stenosis in the distal anterior tibial and dorsalis pedis arteries. Left foot plain radiographs did not show any signs of osteomyelitis and broad-spectrum intravenous antibiotics were started immediately. Non-invasive vascular studies including arterial ankle-brachial index (ABI) and toe-brachial index (TBI) for the dorsalis pedis and posterior tibial arteries were within normal limits.
The patient underwent multiple surgical debridements with a subsequent partial fifth ray (toe and metatarsal) amputation due to abscess extension circumferentially around the fifth metatarsophalangeal joint (MTPJ). Further extensive debridements were performed due to the unhealthy tissue along the fourth toe extensor tendon and paratenon of the fourth metatarsophalangeal capsule. It was noted that the fourth MTPJ capsule postdebridement was exposed. The wound was subsequently left to heal by negative pressure wound therapy application (). Tissue cultures grew penicillin-sensitive Streptococcus agalactiae and antibiotics were tailored according to the culture results. The total duration of antibiotics was 2 weeks prior to definitive closure. A lateral lesser toe fillet flap reconstruction was then performed and after repeated tissue cultures was negative prior to closure.
Operative technique
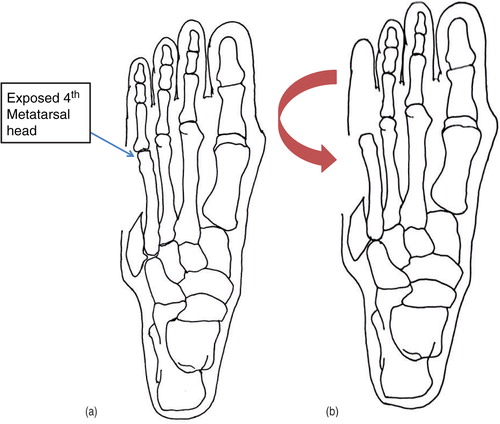
The surgical procedure was performed under regional anesthesia and a tourniquet was used for hemostasis. A sandbag was placed under the ipsilateral gluteal region to allow for better positioning in surgery via internal rotation of the leg. A direct lateral incision was made over the lateral aspect of the fourth toe from the tip of the distal toe to the metatarsal wound, exposing the phalanges of the fourth toe (). The phalanges, tendons, and joint capsule were filleted out from the skin, carefully preserving neurovascular bundles to ensure flap survival. The filleted skin flap was then approximated laterally to the wound using a non-absorbable 4-0 Prolene suture, covering the exposed fourth metatarsal head (a and b).
Fig. 2 Yellow dotted line showing the direct lateral incision made over lateral aspect of fourth toe, exposing the fourth toe phalanges and metatarsal head. Black dotted line showing the original surgical wound defect prior to reconstruction.
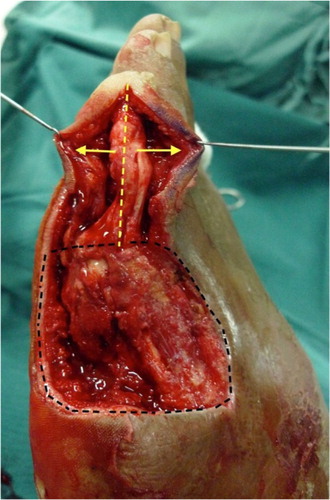
Fig. 3 (a, b) Filleted skin flap from lateral aspect of the fourth toe advanced laterally covering the exposed fourth metatarsal head.
Once the exposed structures were covered, a split-thickness skin graft (STSG) was harvested from the ipsilateral thigh and applied onto the remaining wound bed defect. The STSG was then secured to the wound edges using staples (). A bolster dressing which consisted of a tie-over with flavin cotton wool was placed on STSG for 5 days to ensure maximal graft adherence to wound. The patient was kept non-weight bearing on the left foot for 2 weeks. Oral analgesia was prescribed with non-steroidal anti-inflammatories and paracetamol. Intravenous antibiotics were provided for 1 week due to previous infections and immunocompromised state due to poorly controlled diabetes mellitus. The wound was inspected postoperative on day 5, 10, and 14 for any wound dehiscence, flap necrosis, or infection. Sutures and staples were removed at 2 weeks postoperatively. Dressing changes over the STSG donor site were performed twice weekly thereafter until the STSG was completely incorporated.
Results
The diabetic foot wound healing was uneventful. There was no flap necrosis, secondary infections, or wound dehiscence at 2 weeks post operation. The patient returned to work after 4 weeks postoperatively. At 8 weeks follow-up, the flap was still viable and the STSG was completely incorporated (). The patient was able to walk independently without pain. There was no flap necrosis or recurrent infection. By 6 months, his wound was fully healed and the patient was compliant with his foot care instructions. There were no scar complications and no ulcerations under the remaining metatarsal heads of the left foot.
Discussion
Primary closure for diabetic foot infections is usually rarely performed due to the increased risk of postoperative skin necrosis or poor wound healing secondary to poor vascularity. Secondary wound intention or negative pressure wound therapy is commonly the preferred method, but it carries a significant amount of time and cost to patients (Citation10). Wound coverage for the diabetic foot is feasible, provided that the foot has moderately well-perfused vascularity. Suggested criteria as described by Nather and Wong for distal amputations of the foot should be adopted before performing surgical reconstruction, which includes the presence of one or two palpable pedal pulses, ABI of at least 0.8, and TBI of at least 0.7. This is to ensure good wound healing for the flap reconstruction (Citation11). Furthermore, hemoglobin levels of more than 10 g/dL and serum albumin of more than 25 g/L are important to ensure good wound healing postoperatively (Citation12).
In this case report, wound coverage over the exposed fourth MTPJ and a partial fifth ray amputation could be quite challenging. Traditionally, surgical treatment would have been either secondary intention healing or further amputation proximally. Both of these methods could lead to increased cost, treatment time, and patient morbidity. However, local or distant flap coverage is a viable alternative. The surgical technique described in this case report preserves the pedal length and also reduces donor site morbidity, accelerates wound healing, and preserves the associated metatarsal head, which is important for normal walking and foot pressure distribution. This method may also be applied to both the medial and lateral aspect of the foot with an exposed metatarsal head. Harvesting the soft tissue and creating the fillet flap by amputating the fourth toe at the MTPJ level was justified because the next surgical option in this case would have also involved amputation of the fourth toe in a more proximal site.
Aerden et al. have described a primary closure with a fillet flap for the big toe for osteomyelitis of diabetic foot via a case series (Citation7). They have shown a delayed mean healing time of 44 days with disappointing long-term results, with ulcer recurrences under the remaining metatarsal heads (Citation7). Our case report did not show any similar complications of ulceration under the remaining metatarsal heads. We postulate that this may be due to the ability of the lesser toes to distribute the weight bearing pressures leading to a better outcome as compared to the hallux fillet flap. This may also suggest that the lateral lesser toe fillet flap may be more successful than a medial fillet flap.
Kuntscher et al. have described the concept of fillet flaps in their series of 50 finger and toe fillets (Citation2). Flap necrosis was observed in patients with diabetes mellitus; however, there was no mention of patient selection in terms of vascularity, hemoglobin, and albumin levels. In our study, we opted to use strict patient selection criteria as proposed by Nather and Wong (Citation11). We believe that the strict selection criteria may have significantly improved the chances of flap survival in this case.
In conclusion, this case report describes the patient selection and surgical technique of the lateral lesser toe fillet flap for diabetic foot closure of a previously partial fifth ray amputation site. Advantages of this technique include good soft tissue durability and preventing the need for more proximal amputation for adequate soft tissue coverage. As this is a case report, more patients will be needed to further solidify the concept of lateral lesser toe fillet flaps in terms of patient selection and clinical outcomes for soft tissue closure of the diabetic foot. Randomized controlled trials comparing patient selection criteria and different methods of flap coverage for partial ray amputations in diabetic patients are needed.
Conclusion
The lateral lesser toe fillet flap reconstruction is a reproducible technique that incurs comparatively minimal technical complexity and provides a favorable option in the management of diabetic foot wounds where soft tissue coverage is required.
Conflict of interest and funding
The authors declare that they have no conflict of interest and have not received any funding or benefits from industry to write this article.
References
- Alpert BS, Buncke HJ. Multilating multidigital injuries: use of a free microvascular flap from a nonreplantable part. J Hand Surg Am. 1978; 3: 196–8. [PubMed Abstract].
- Küntscher MV, Erdmann D, Homann HH, Steinau HU, Levin SL, Germann G. The concept of fillet flaps: classification, indications, and analysis of their clinical value. Plast Reconstr Surg. 2001; 108: 885–96.
- Talbot SG, Mehrara BJ, Disa JJ, Wong AK, Pusic A, Cordeiro PG, etal. Soft-tissue coverage of the hand following sarcoma resection. Plast Reconstr Surg. 2008; 121: 534–43. [PubMed Abstract].
- Ghali S, Harris PA, Khan U, Pearse M, Nanchahal J. Leg length preservation with pedicled fillet of foot flaps after traumatic amputations. Plast Reconstr Surg. 2005; 115: 498–505. [PubMed Abstract].
- Shaw WW, Ko CY. Salvage of a below-the-knee amputation with a fillet of foot free flap: a 15-year follow-up. Ann Plast Surg. 1996; 37: 433–8. [PubMed Abstract].
- Noble-Bell G, Forbes A. A systematic review of the effectiveness of negative pressure wound therapy in the management of diabetes foot ulcers. Int Wound J. 2008; 5: 233–42. [PubMed Abstract].
- Aerden D, Vanmierlo B, Denecker N, Brasseur L, Keymeulen B, Van den Brande P. Primary closure with a filleted hallux flap after transmetatarsal amputation of the big toe for osteomyelitis in the diabetic foot: a short series of four cases. Int J Low Extrem Wounds. 2012; 11: 80–4. [PubMed Abstract].
- Kalbermatten DF, Kalbermatten NT, Haug M, Schäfer D, Pierer G. Use of a combined pedicled toe fillet flap. Scand J Plast Reconstr Surg Hand Surg. 2004; 38: 301–5. [PubMed Abstract].
- Lin CH, Wei FC, Chen HC. Filleted toe flap for chronic forefoot ulcer reconstruction. Ann Plast Surg. 2000; 44: 412–16. [PubMed Abstract].
- Nather A, Hong NY, Lin WK, Sakharam JA. Effectiveness of bridge V.A.C. dressings in the treatment of diabetic foot ulcers. Diabet Foot Ankle. 2011; 2: 5893. http://dx.doi.org/10.3402/dfa.v2i0.5893.
- Nather A, Wong KL. Distal amputations for the diabetic foot. Diabet Foot Ankle. 2013; 4: 21288. http://dx.doi.org/10.3402/dfa.v4i0.21288.
- Pinzur MS, Stuck RM, Sage R, Hunt N, Rabinovich Z. Syme ankle disarticulation in patients with diabetes. J Bone Joint Surg Am. 2003; 85-A: 1667–72. [PubMed Abstract].



