Abstract
Background: A number of theories have proposed possible mechanisms that may explain the high rates of comorbidity between posttraumatic stress disorder (PTSD) and persistent pain; however, there has been limited research investigating these factors.
Objective: The present study sought to prospectively examine whether catastrophizing predicted the development of PTSD symptoms and persistent pain following physical injury.
Design: Participants (N = 208) completed measures of PTSD symptomatology, pain intensity and catastrophizing during hospitalization following severe injury, and 3 and 12 months postinjury. Cross-lagged path analysis explored the longitudinal relationship between these variables.
Results: Acute catastrophizing significantly predicted PTSD symptoms but not pain intensity 3 months postinjury. In turn, 3-month catastrophizing predicted pain intensity, but not PTSD symptoms 12 months postinjury. Indirect relations were also found between acute catastrophizing and 12-month PTSD symptoms and pain intensity. Relations were mediated via 3-month PTSD symptoms and 3-month catastrophizing, respectively. Acute symptoms did not predict 3-month catastrophizing and catastrophizing did not fully account for the relationship between PTSD symptoms and pain intensity.
Conclusions: Findings partially support theories that propose a role for catastrophizing processes in understanding vulnerability to pain and posttrauma symptomatology and, thus, a possible mechanism for comorbidity between these conditions.
For the abstract or full text in other languages, please see Supplementary files under Reading Tools online
Increasing research evidence suggests that posttraumatic stress disorder (PTSD) and persistent pain are frequently comorbid. Recent reviews have reported that 10–50% of individuals with persistent pain meet diagnostic criteria for PTSD, while 21–80% of PTSD samples report the presence of comorbid pain (Otis, Pincus, & Keane, Citation2006; Villano et al., Citation2007). PTSD symptoms may develop following trauma exposure and comprise re-experiencing the trauma through unwanted thoughts, memories, and reactions; avoidance of trauma reminders, psychological numbing, and symptoms of hyperarousal (American Psychiatric Association, Citation2000). Persistent pain is often defined as pain that is ongoing for at least 3–6 months (Merskey & Bogduk, Citation1994).
Variations in prevalence rates may be influenced by differences in sampled populations, assessment methods, and criteria used to define PTSD and pain (Otis et al., Citation2006). Nevertheless, it has been consistently shown that the severity of acute PTSD symptoms predict later pain severity (Drottning, Staff, Levin, & Malt, Citation1995; Jenewein, Moergeli et al., Citation2009) and that acute pain predicts subsequent PTSD severity and diagnosis (Norman, Stein, Dimsdale, & Hoyt, Citation2008; Schnyder, Wittmann, Friedrich-Perez, Hepp, & Moergeli, Citation2008). In addition, symptoms of PTSD and pain have been proposed to mutually maintain each other and research evidence provides some support for this interaction (Jenewein, Wittmann, Moergeli, Creutzig, & Schnyder, Citation2009; CitationLiedl et al., 2010; Sharp & Harvey, Citation2001). Mechanisms that may explain vulnerability to the development of comorbidity have also received increasing theoretical attention (Asmundson, Coons, Taylor, & Katz, Citation2002; Asmundson & Katz, Citation2009; Asmundson & Taylor, Citation2006; McLean, Clauw, Abelson, & Liberzon, Citation2005; Otis, Keane, & Kerns, Citation2003; Otis et al., Citation2006).
One proposed mechanism of vulnerability, is catastrophizing defined as “an exaggerated negative orientation toward noxious stimuli” (Sullivan, Bishop, & Pivik, Citation1995, p. 524). Catastrophizing has been implicated in dominant theoretical models of both disorders. For example, the fear-avoidance model of persistent pain proposes that pain catastrophizing precipitates fear and physical arousal, resulting in avoidance of activities associated with pain and subsequent disuse, depression, and disability (Norton & Asmundson, Citation2003; Vlaeyen & Linton, Citation2000). In turn, these outcomes are hypothesized to enhance pain, triggering further catastrophic appraisals and maintaining the cycle of pathology.
Catastrophizing has also been implicated in cognitive models of PTSD. For example, Ehlers and Clark (Citation2000) proposed that “excessively negative appraisals of the traumatic event and/or its sequelae” (p. 319) perpetuate an ongoing sense of threat, triggering fear, physiological arousal and, in turn, avoidance of trauma-related stimuli. Avoidance may prevent disconfirmation of perceived danger, in addition to interfering with the effective processing of trauma memories that, in turn, perpetuates catastrophic appraisals and the cycle of fear and avoidance (Ehlers & Clark, Citation2000). Similarities between theories of PTSD and persistent pain, have lead some authors to suggest that a tendency to catastrophize the meaning of aversive experiences related to the trauma, negative reactions, and pain may predispose a vulnerability to symptomatology associated with both conditions and thus comorbidity (Otis et al., Citation2006).
Preliminary empirical evidence has supported propositions that catastrophizing presents a vulnerability to PTSD symptomatology and to increased pain severity. For example, pretrauma catastrophic self-appraisals have been found to predict subsequent PTSD severity for fire-fighting recruits following exposure to fire-fighting duties (Bryant & Guthrie, Citation2005; Bryant & Guthrie, Citation2007). Prospective research has also found that pre-existing catastrophizing predicts increased pain during childbirth and following caesarean section (Flink, Mroczek, Sullivan, & Linton, Citation2009; Strulov et al., Citation2007). These findings suggest that catastrophizing may represent a predisposition to the development of pathology, rather than a response to symptomatology.
While few studies have examined comorbidity, pain catastrophizing has been associated with increased PTSD symptoms in litigating pain patients and with PTSD symptom severity and maintenance in individuals with whiplash injury (Duckworth & Iezzi, Citation2005; Sullivan et al., Citation2009). These findings suggest that catastrophizing may mediate PTSD symptom severity in pain patients. However, participants had pre-existing pain and PTSD symptomatology and it was thus unclear whether catastrophizing had contributed to the development of symptoms or had developed in response to symptomatology. Based on cognitive-behavioral models described above (Ehlers & Clark, Citation2000; Vlaeyen & Linton, Citation2000), it could be expected that a reciprocal relationship exists, whereby catastrophizing predicts pain and PTSD symptoms, which in turn intensify catastrophizing, causing subsequent increased pain and PTSD severity and thus maintaining comorbidity.
Research investigating catastrophizing and comorbid PTSD and pain is further limited by issues concerning the definition and measurement of this construct and the narrow focus on pain catastrophizing within much of the literature. Sullivan et al. (Citation2001) noted that individuals who catastrophize pain are likely to catastrophize other stressors; however, few studies have explored the nature or consequences of catastrophizing other aversive experiences. Thus while PTSD research has indicated that catastrophizing appraisals increase vulnerability to the development and maintenance of PTSD symptoms and diagnosis, these studies often use the terminology of negative interpretations or appraisals to describe catastrophizing cognitions and do not refer specifically to catastrophizing (Bryant & Guthrie, Citation2005; Dunmore, Clark, & Ehlers, Citation2001; Ehlers, Mayou, & Bryant, Citation1998; O'Donnell, Elliott, Wolfgang, & Creamer, Citation2007). The definition and operationalization of catastrophizing within the PTSD literature is thus less consistent than that used within the pain literature, where specific catastrophizing scales such as the Pain Catastrophizing Scale (PCS; Sullivan et al., Citation1995) have been developed.
Even within the pain literature, there has been debate regarding whether catastrophizing should be considered within the framework of a schema-activation model, an appraisal model, a coping model, or as a personality trait, in addition to speculation that catastrophizing may represent the same construct as neuroticism and depression (CitationGilliam et al., 2010; Sullivan et al., Citation2001). However, a number of studies have found that catastrophizing predicts pain severity independently from neuroticism or depression, suggesting that catastrophizing is related, but distinct, from these factors (Sullivan et al., Citation2001). While catastrophizing thus appears to represent an important factor that explains vulnerability to physical and psychological pathology, further research is needed to determine how best to understand and measure this construct.
One of the few measures of non-pain-related catastrophizing is the catastrophizing subscale of the Cognitive Emotion Regulation Questionnaire (CERQ). The CERQ was designed to assess cognitive coping strategies used to regulate emotions in response to aversive experiences (Garnefski, Kraaij, & Spinhoven, 2001) and as such, can be used to assess whether the tendency to catastrophize non-pain-specific stressors contributes to the development and maintenance of symptoms of PTSD and persistent pain. Studies of the CERQ have indicated that this scale assesses cognitive coping strategies that are enduring characteristics, but less stable over time than traits (Garnefski, Kraaij, & Spinhoven, 2002). Catastrophizing, thus differs from related constructs such as negative affectivity, which is believed to represent a trait-like tendency to experience negative emotions and influences a predispositional tendency to catastrophize (Keogh & Asmundson, Citation2004). The CERQ thus appears to be a useful measure of catastrophizing, which is consistent with definitions of this construct as a coping response to aversive experiences.
This prospective study was designed to address some of the limitations of existing empirical research, particularly the lack of prospective research and narrow focus on pain catastrophizing, by investigating whether catastrophizing as measured by the CERQ, contributed to the development of PTSD symptoms and persistent pain, 3 and 12 months following severe injury. It was hypothesized that: (a) acute catastrophizing would be associated with increased pain intensity and PTSD symptoms 3 months postinjury; (b) in accordance with cognitive-behavioral models, which propose that symptoms may in turn elicit catastrophizing responses, it was predicted that acute PTSD symptoms and pain intensity would be associated with increased 3-month catastrophizing that in turn, (c) would be associated with the maintenance of PTSD symptoms and pain intensity 12 months postinjury. Finally, it was hypothesized (d) that 3-month catastrophizing would mediate the relationship between acute PTSD symptoms and 12-month pain intensity and the relationship between acute pain intensity and 12-month PTSD symptoms, thus reflecting a mutual maintenance factor.
Method
Participants
The study was nested within the Injury Vulnerability Study, which examined risk factors and psychopathology following severe injury. The current sample comprised 301 participants who were admitted to either the Alfred or Royal Melbourne hospitals, following severe injury. Patients were included in the study if they were aged between 16 and 70 years, had been hospitalized for a minimum of 24 hours, did not have moderate or severe traumatic brain injury (TBI), and had a reasonable comprehension of English. Participants were excluded if the injury was a result of self-harm, patients were actively suicidal, experiencing psychosis or cognitive impairment, were non-resident visitors to Australia, or were under police guard.
A total of 208 participants (69%) completed measures of interest during hospitalization and 3 and 12 months postinjury. Seventy-five percent of these participants were male (n=156) and the mean age was 40.25 (SD = 13.54). Mean injury severity score (ISS) was 12.72 (SD=8) and 56% of participants sustained a mild traumatic brain injury (MTBI: n = 117). Participants were hospitalized for an average of 11.5 days (SD=9.32). The majority of participants had been injured as a result of motor vehicle accident (MVA; 67.8%, n=141). Other mechanisms of injury included fall (11.5%, n = 24), assault (5.8%, n=12), workplace injury (4.3% n=9), and other types of accidents (9.1%, n=19).
Measures
Demographic and injury information, ISS and MTBI (American Congress of Rehabilitation Medicine, Citation1993) were obtained from patient files. The ISS was determined by squaring the three largest Abbreviated Injury Scale (AIS) scores allocated to injuries sustained for six body regions and adding these together (Baker, O'Neil, Haddon, & Long, Citation1974). The ISS ranges between 0 and 75.
PTSD
The PTSD symptoms were assessed using the Clinician Administered PTSD Scale for DSM-IV (CAPS-IV; Blake et al., Citation1998). The CAPS is a structured clinical interview that assesses the frequency and intensity of each of the DSM-IV criteria required to meet a PTSD diagnosis (American Psychiatric Association, Citation2000). The 17 items that comprise PTSD criteria are measured by 5-point scales that assess the frequency and intensity of each symptom, ranging from 0 (never) to 4 (daily or almost every day) and 0 (none) to 4 (extreme), respectively. The CAPS has demonstrated excellent reliability and validity (Weathers, Keane, & Davidson, Citation2001).
In accordance with previous studies examining PTSD outcomes following severe injury, psychogenic amnesia was excluded from the CAPS total, due to difficulties differentiating psychogenic from organic amnesia (O'Donnell, Creamer, Bryant, Schnyder, & Shalev, Citation2006). CAPS totals were determined by summing frequency and intensity scores to obtain a total score ranging between 0 and 128.
Pain intensity
Pain intensity at the time of hospital assessment was measured using an 11-point Visual Analogue Scale (VAS; Huskisson, Citation1974; Scott & Huskisson, Citation1974). At 3- and 12-month follow-up, participants rated the average pain that they had experienced during the previous 2 weeks. The VAS is one of the most commonly used measures of perception of pain intensity (Sherman & Ohrbach, Citation2006) and provides a reliable and change-sensitive measurement of subjective experience of pain (Jensen, Karoly, & Braver, Citation1986; Price, McGarath, Rafii, & Buckingham, Citation1983).
Catastrophizing
Catastrophizing was assessed using the catastrophizing subscale from the 36-item CERQ (Garnefski et al., Citation2001). The catastrophizing subscale is comprised of four items (e.g., “I often think that what I have experienced is the worst that can happen to a person”) measured on a 5-point Likert scale, ranging from 1 ([almost] never) to 5 ([almost] always). The acute questionnaire asked participants to describe their general approach to stressful situations, while the 3-month questionnaire directed them to consider how frequently they engaged in the process in response to the trauma. The English version of the CERQ was developed from the original Dutch version, using a back-translation procedure.
The CERQ has demonstrated good factorial validity and reliability across a range of populations (Garnefski et al., Citation2001Citation2002; Martin & Dahlen, Citation2005). The catastrophizing subscale has demonstrated acceptable to good internal reliability of 0.68–0.80 (Garnefski et al., Citation2002; Jermann, Van der Linden, d'Acremont, & Zermatten, Citation2006). Test-retest correlations of 0.62 over a 14-month period suggest that catastrophizing represents a stable cognitive style over time (Garnefski et al., Citation2002). An internal consistency alpha of 0.74 has been reported for the catastrophizing subscale of the English version of the CERQ (Martin & Dahlen, Citation2005).
Procedure
Participants were randomly selected using an automated procedure over an 18-month period. The CAPS was administered prior to hospital discharge and the VAS and CERQ were included in a self-report booklet that participants completed following the interview. Interviews were conducted on average 6.1 days (SD=6.23) from the time of admission.
CAPS interviews were conducted by telephone at 3 and 12 months postinjury. Telephone interviews using the CAPS have been found to reliably assess PTSD symptoms (Aziz & Kenford, Citation2004). The self-report booklet containing the VAS and CERQ was posted to participants and returned via mail. All CAPS interviews were audio recorded. Inter-rater reliability was undertaken for 5% of the entire sample of the Injury Vulnerability Study. Diagnostic consistency between assessors was 0.99 for the whole sample across the three time points.
Data analysis
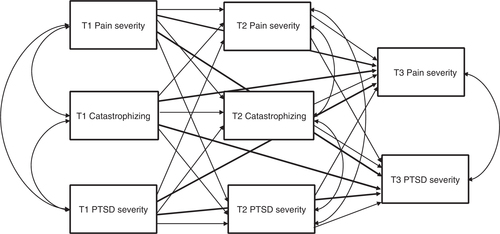
Path analysis examined the direct effects of catastrophizing on subsequent PTSD symptoms and pain intensity, the direct effects of acute symptoms for 3-month catastrophizing and the indirect effect of 3-month catastrophizing in mediating between acute and 12-month symptoms. A saturated, cross-lagged path model was assessed using the AMOS 16 statistical package (Arbuckle, Citation2007) and is displayed in . Preacher and Hayes (Citation2008) noted that including several mediators (i.e., 3-month PTSD symptoms, 3-month pain, and 3-month catastrophizing) within the same model, provides the opportunity to compare competing theories. Thus the current analysis enabled examination of whether acute and 3-month catastrophizing predicted symptoms of PTSD and pain, while controlling for the effects of acute and 3-month symptomatology.
Figure 1. Saturated model containing all possible pathways. T1 = acute period (M = 6.1 days postinjury, SD=6.23); T2 = 3 months postinjury; T3 = 12 months postinjury). Bold lines represent direct effects from time one to time three variables.
Examination of sample distributions indicated that the data were positively skewed. To address this issue, a bootstrapping method was selected as unlike maximum likelihood estimation, bootstrapping does not make assumptions about sampling distributions (Nevitt & Hancock, Citation2001; Preacher & Hayes, Citation2008). Furthermore bootstrapping procedures have been recommended when testing indirect effects, as the sampling distribution of indirect effects is rarely normal (Preacher & Hayes, Citation2008). Bootstrapping involves resampling the data to create n number of bootstrap samples, the same size as the original sample with replacement. This process establishes an empirical approximation of the sampling distribution. An observation from the original sample may appear once, multiple times, or not at all within each bootstrap sample. Backward elimination was used to trim non-significant paths based on bias-corrected 95% confidence intervals using n=5,000 bootstrap samples (MacKinnon, Lockwood, & Williams, Citation2004; Preacher & Hayes, Citation2008). The Bollen Stine bootstrap was used to obtain a corrected chi square statistic, using n=250 bootstrap samples (Nevitt & Hancock, Citation2001).
All other comparisons (e.g., between completers and non-completers) were conducted using SPSS 15.0. Non-parametric analyses were used to address violations of normality. Thus chi square analyses compared outcomes for dichotomous data and continuous variables were analyzed using Mann–Whitney tests with Monte Carlo bootstrapping (n=5,000). Spearman's Rank Order Correlation was used to assess bivariate correlations between factors included in the model.
Results
Sample characteristics
displays mean scores for the CAPS, CERQ, and VAS totals. Completers were on average significantly older (Mdn=40.5) than non-completers (Mdn=31), U = 6608, z=–4.274, p < .001, but did not differ significantly on any other demographic, injury severity, or acute outcome measures. MTBI and ISS were not found to influence PTSD or pain outcomes.
Table 1. Mean PTSD, pain and catastrophizing severity scores (n=208)
Correlation matrix
The correlation matrix for all bivariate relations between variables is presented in . Significant relations were found between all factors, with the exception of acute catastrophizing and 12-month pain.
Table 2. Correlation matrix of variables included in path analysis
Path analysis
Figure 2 displays the final model containing path coefficients between outcomes across all three assessment time points. Coefficients are presented in standardized form to enable comparison between paths. Following backward elimination of non-significant paths, statistical tests indicated that the model fit the data well: Bollen Stine χ2 p=.307, CFI=.988, GFI=.981, and RMSEA=.053.
Standardized path coefficients reflect the degree to which an increase in 1 standard deviation (SD) from the mean of the predictor variable is associated with an increase in the SD of the dependent variable (Kline, Citation2005). For example, examination of , indicates that an increase of 1 SD above the mean in acute catastrophizing will predict an increase of .20 SDs above the mean for 3-month PTSD severity. Likewise, an increase of 1 SD for acute PTSD severity is associated with an increase of .40 SDs for 3-month PTSD severity. Thus the standardized effect of acute PTSD severity for 3-month PTSD severity is approximately twice as great as the effect of acute catastrophizing. Such high temporal stability of symptoms of PTSD, pain, and catastrophizing across the three time periods supports the use of a saturated model to control for prior levels of outcome variables. All factors were also significantly correlated cross-sectionally, however, causative influences cannot be established for cross-sectional measures.
Figure 2. Final model following backward elimination of non-significant pathways. N=208. The figure displays standardized path coefficients between measures of PTSD, catastrophizing and pain severity. T1 = acute (M = 6.1 days postinjury, SD=6.23); T2 = 3 months postinjury; T3 = 12 months postinjury. Bold line represents direct effects from T1 to T3 variables. All correlations (not shown) were significant (T1 PTSD severity–T1 catastrophizing, β=.28**; T1 PTSD severity–T1 pain severity, β=.24**; T1 catastrophizing–T1 pain severity, β=.27**; T2 PTSD severity–T2 catastrophizing, β=.28**; T2 PTSD severity–T2 pain severity, β=.18*; T2 catastrophizing–T2 pain severity, β=.22**; T3 PTSD severity–T3 pain severity, β=.17**). p<.05; **p<.01
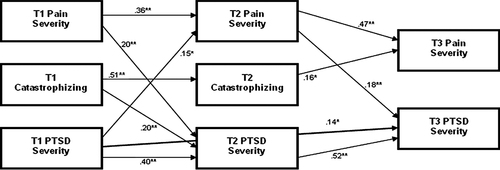
The model indicates that acute catastrophizing significantly predicted PTSD symptoms, but not pain intensity 3-months postinjury. Conversely, acute PTSD and pain intensity did not predict 3-month catastrophizing. Three-month catastrophizing significantly predicted 12-month pain intensity but did not predict 12-month PTSD symptoms. Of note, a significant indirect relationship was also found between acute catastrophizing and 12-month PTSD symptomatology (β=.10, p < .01), which was mediated via 3-month PTSD symptoms. These effects may be interpreted in the same way as path coefficients. Thus an increase in 1 SD of the mean for acute catastrophizing, is associated with an increase of .10 SDs for 12-month PTSD, via the impact of acute catastrophizing on 3-month PTSD and in turn, 3-month PTSD for 12-month PTSD (Kline, Citation2005). Likewise, 3-month catastrophizing was found to mediate the relationship between acute catastrophizing and 12-month pain intensity (β=.08, p < .05). However, 3-month catastrophizing did not mediate relations between acute pain and 12-month PTSD or between acute PTSD and 12-month pain.
The exploration of the longitudinal relationship between symptoms of specific-PTSD and specific-pain was not a central aim of the current study; however, the design of the research enabled an examination of this relationship. It is worth describing the relationship between symptoms of these disorders, as it further informs the longitudinal relationship that may explain high rates of comorbidity between PTSD and pain.
The model shows that acute PTSD symptoms predicted 3-month pain intensity and also indirectly predicted 12-month pain intensity (β=.07, p < .05), mediated via 3-month pain. However 3-month PTSD symptoms did not directly predict 12-month pain intensity. Likewise acute pain intensity predicted 3-month PTSD symptoms and indirectly predicted 12-month PTSD symptoms, mediated via 3-month PTSD symptoms (β=.10) and 3-month pain intensity (β=.07), respectively (total indirect effect: β=.17, p < .001). Three-month pain intensity also directly predicted 12-month PTSD symptoms and contributed to the indirect effects between acute PTSD symptoms and 12-month PTSD symptoms (β =.03), which was also mediated via 3-month PTSD symptoms (β=.21; total indirect effect: β=.24, p < .01). The total effect of acute PTSD symptoms for 12-month PTSD symptoms was thus β=.38, p < .001. Likewise a significant indirect relationship was found between acute pain symptoms and 12-month pain intensity, mediated via 3-month pain (β=.17, p < .05).
Discussion
There has been growing interest in the mechanisms that may increase vulnerability to both PTSD symptoms and persistent pain. The present study was the first to examine whether one proposed factor, catastrophizing, was associated with increased risk of these symptoms following severe injury. The findings of the current study partially supported hypothesis (a) that catastrophizing would predict worse outcomes for PTSD symptoms. Contrary to this hypothesis however, acute catastrophizing did not predict 3-month pain intensity. Likewise, contrary to hypothesis (b), acute PTSD and pain symptoms were not associated with increased 3-month catastrophizing. The findings partially supported hypothesis (c) that 3-month catastrophizing would be associated with 12-month pain intensity. However, they did not support the hypothesis that catastrophizing would be associated with the maintenance of PTSD symptoms. Finally, the findings did not support hypothesis (d) that catastrophizing would directly mediate the relationship between pain and PTSD symptoms. As few prospective studies have examined the relationship between catastrophizing and the development of either symptoms of PTSD or pain, these findings provide important insight into how catastrophizing may influence these conditions after injury and, in particular, how this relationship may change over time.
Catastrophizing appeared to be a relatively stable response across the first 3 months postinjury, possibly reflecting a pre-existing cognitive coping approach to stress and trauma. Accordingly, the results suggest that while a tendency to catastrophize may remain fairly stable, the influence of catastrophizing on pain and PTSD symptoms varies according to the period of recovery. It is also notable that acute catastrophizing was associated with worse 12-month PTSD and pain outcomes, mediated via 3-month PTSD symptom severity and catastrophizing, respectively, as these findings suggest that acute catastrophizing may represent a vulnerability to ongoing pathology.
Although acute catastrophizing did not predict pain intensity 3 months postinjury, it was associated with the development of persistent pain (between 3 and 12 months postinjury). It is possible that as the participants involved in this study had experienced serious injury, physical recovery factors may have had a more profound impact on pain intensity during the initial months postinjury compared to cognitive factors (i.e., catastrophizing). Following this period of healing, ongoing catastrophizing may disrupt further recovery, perhaps by triggering fear-avoidance behavior in excess of injury factors (Vlaeyen & Linton, Citation2000).
Likewise, the relationship between catastrophizing and PTSD symptoms appeared to change over time. Thus while catastrophizing was associated with the development of PTSD symptoms, the findings are inconsistent with studies that have implicated catastrophic appraisals in the maintenance of PTSD symptomatology (Dunmore et al., Citation2001; Ehlers et al., Citation1998; O'Donnell, Elliott, Wolfgang, & Creamer, Citation2007). One explanation for these inconsistencies may concern the operationalization of catastrophizing. The present study examined catastrophizing as a coping strategy in response to trauma, rather than examining the specific types of catastrophizing appraisals (e.g., regarding oneself or of trauma sequelae) that have been found to maintain PTSD symptomatology (Dunmore et al., Citation2001; Ehlers et al., Citation1998; O'Donnell et al., 2007). It is possible that catastrophizing as a cognitive coping strategy may increase perceptions of ongoing threat and disrupt initial recovery possibly by influencing catastrophic appraisals. This process however, may differ from the processes involved in appraising specific aspects of oneself, trauma and sequelae in a catastrophic manner, and the interaction of such appraisals with other factors in maintaining PTSD symptoms.
Finally, while the findings suggested that catastrophizing increased vulnerability to the development of PTSD symptoms and persistent pain thus increasing risk of comorbidity, this factor did not represent a direct mediator in the maintenance of PTSD symptoms and pain, suggesting that other factors may be involved in this process. In their mutual maintenance model of comorbid PTSD and persistent pain, Sharp and Harvey (Citation2001) have suggested seven broad mechanisms that may maintain comorbidity and it is possible that one of these factors such as avoidance may become increasingly prominent in the maintenance of PTSD symptoms and pain. These findings highlight the need for further examination of the processes represented by the components described within complex, multidimensional, cognitive-behavioral models, and the interrelationships between these components.
While the study was not designed to examine the relationship between PTSD and persistent pain, it is also worth briefly noting the changing nature of the relationship between these disorders during the course of the study. PTSD and pain symptomatology were found to mutually influence each other during the initial months postinjury, but PTSD did not appear to maintain pain between 3 and 12 months postinjury. One interpretation of these findings is the involvement of recovery factors. Mild symptoms of PTSD are not uncommon following severe injury and for the majority of individuals subside over the first 3 months (Koren, Arnon, & Klein, Citation1999). During this period, PTSD symptoms of hyperarousal may increase pain while individuals are physically recovering from injury as arousal has a strong relationship with pain intensity (CitationLiedl et al., 2010; Norton & Asmundson, Citation2003). In turn, pain may have maintained PTSD symptoms by serving as a reminder of the trauma, triggering other trauma-related memories, associated arousal responses, and exacerbating avoidance (Sharp & Harvey, Citation2001).
As with any research, there are some limitations that should be noted. Firstly, men were overrepresented within the sample and the predominant mechanism of injury was MVA. Participants also had very low levels of PTSD, pain, and catastrophizing symptomatology. These sample characteristics and levels of pathology are similar to those reported in other, non-clinical samples following severe injury (CitationdeRoon-Cassini, Mancini, Rusch, & Bonnano, 2010; Jenewein, Wittmann et al., 2009). However younger participants were also less likely to complete follow-up measures. Thus, while these results may inform relationships between catastrophizing, PTSD symptoms, and pain intensity in severe injury populations, further research is needed to determine generalizability to broader trauma populations and younger injury survivors.
A number of measurement issues should also be noted. Firstly, while the VAS has been shown to be a change-sensitive measure of pain perception (Scrimshaw & Maher, Citation2001), inclusion of a scale that assesses other cognitive, physical, emotional, and behavioral elements of pain may have further elucidated the relationship between pain, catastrophizing, and PTSD symptomatology. Secondly, while the CERQ was selected as a validated measure of catastrophizing that is not specific to pain, the scale contained only a limited number of catastrophizing items and measured catastrophizing in response to stress generally and trauma subsequently. It is possible that the nature of the stressors that participants were directed to consider may have influenced the strength of the relationship between catastrophizing and outcomes.
This issue relates to inconsistencies concerning the definition and measurement of catastrophizing previously noted. Further research is thus required to investigate the nature of the cognitive processes represented by catastrophizing and the measurement of this multifaceted construct. For example, while rumination is considered to represent a subcomponent of catastrophizing within the pain literature and is included as a subscale in the PCS (Sullivan et al., Citation1995), psychometric research of the CERQ suggests that rumination may represent a related but distinct construct to catastrophizing (Garnefski et al., Citation2001). Given these limitations, the current study was designed as a preliminary exploration of the role of catastrophizing in the development of PTSD and persistent pain symptomatology. Accordingly, the model could not contain the range of possible factors that may contribute to the development and maintenance of these conditions. Future studies could further examine how injury and trauma-related factors as well as longitudinal factors affect the relationship between catastrophizing and PTSD and pain outcomes in addition to investigating other possible mechanisms of comorbidity (Asmundson & Katz, Citation2009; Otis et al., Citation2006; Sharp & Harvey, Citation2001).
Conclusions
The present study is the first to prospectively examine catastrophizing as a factor predisposing vulnerability to the development of PTSD symptoms and persistent pain following severe injury. The findings provide partial support for emerging theories that catastrophizing may increase vulnerability to PTSD symptoms and pain, as well as the development of comorbid pathology. Trauma-focused interventions including cognitive therapy have been recommended for individuals who display acute stress disorder or PTSD reactions 2 weeks posttrauma (Australian Centre for Posttraumatic Mental Health, Citation2007). In such cases, targeting catastrophic reactions may enhance recovery and reduce vulnerability to the development of long-term physical and psychological pathology.
Conflict of interest and funding
There is no conflict of interest in the present study for any of the authors.
French abstract
Download PDF (82.5 KB)German abstract
Download PDF (63.7 KB)Italian abstract
Download PDF (50.7 KB)Polish abstract
Download PDF (85.2 KB)Russian abstract
Download PDF (58.3 KB)Spanish abstract
Download PDF (11.7 KB)Turkish abstract
Download PDF (38.1 KB)Ukranian abstract
Download PDF (125.7 KB)Acknowledgements
This study was supported by an NHMRC Program Grant (300304), a Victorian Trauma Foundation grant (#V-11), and a National Health and Medical Research Council Australian Clinical Research Fellowship (359284).
References
- American Congress of Rehabilitation Medicine. (1993). Definition of mild traumatic brain injury. Journal of Head Trauma Rehabilitation. , 8 (3), 86–87. DOI: http://ovidsp.tx.ovid.com.ezp.lib.unimelb.edu.au/.
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders. (4th ed.)—Text revision. ArlingtonVA: American Psychiatric Association.
- Arbuckle J. L. Amos 16.0 user's guide. SPSS Inc. Chicago, 2007
- Asmundson, G. J., Coons, M. J., Taylor, S., & Katz, J. (2002). PTSD and the experience of pain: Research and clinical implications of shared vulnerability and mutual maintenance models. The Canadian Journal of Psychiatry/La Revue canadienne de psychiatrie. , 47. (10), 930–937. DOI: https://ww1.cpa-apc.org/Publications/Archives/CJP/2002/december/asmundson.pdf.
- Asmundson, G. J., & Katz, J. (2009). Understanding the co-occurrence of anxiety disorders and chronic pain: State-of-the-art. Depression & Anxiety. 26 (10), 888–901. 10.3402/ejpt.v2i0.5652.
- Asmundson, G. J., & Taylor, S. (2006). PTSD and chronic pain: Cognitive-behavioral perspectives and practical implications. In: G. Young, A. W. Kane, & K. Nicholson. Psychological knowledge in court: PTSD, pain, and TBI. (pp. 225–241.). New York: Springer Science & Business Media.
- Australian Centre for Posttraumatic Mental Health. (2007). Australian guidelines for the treatment of adults with posttraumatic stress disorder and acute stress disorder. Melbourne: ACPMH. Retrieved from http://www.acpmh.unimelb.edu.au/resources/resources-guidelines.html. Accessed: 2nd May 2010.
- Aziz, M. A., & Kenford, S. (2004). Comparability of telephone and face-to-face interviews in assessing patients with posttraumatic stress disorder. Journal of Psychiatric Practice. 10(5), 307–313. DOI: 10.3402/ejpt.v2i0.5652.
- Baker, S. P., O'Neil, B., Haddon, W., & Long, W. B. (1974). The injury severity score: A method for describing patients with multiple injuries and evaluating emergency care. Journal of Trauma. 14(2), 187–196. DOI: 10.3402/ejpt.v2i0.5652.
- Blake D. D. Weathers F. W. Nagy L. M. Kaloupek D. G. Charney D. S. Keane T. M. Clinician-administered PTSD scale for DSM-IV. National Center for Posttraumatic Stress Disorder. Boston, 1998
- Bryant, R. A., & Guthrie, R. M. (2005). Maladaptive appraisals as a risk factor for posttraumatic stress: A study of trainee firefighters. Psychological Science. 16(10), 749–752. DOI: 10.3402/ejpt.v2i0.5652.
- Bryant, R. A., & Guthrie, R. M. (2007). Maladaptive self-appraisals before trauma exposure predict posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 75(5), 812–815. DOI: 10.3402/ejpt.v2i0.5652.
- deRoon-Cassini, T. A., Mancini, A. D., Rusch, M. D., & Bonnano, G. A. (2010). Psychopathology and resilience following traumatic injury: A latent growth mixture model analysis. Rehabilitation Psychology. 55(1), 1–11. DOI: 10.3402/ejpt.v2i0.5652.
- Drottning, M., Staff, P. H., Levin, L., & Malt, U. F. (1995). Acute emotional response to common whiplash predicts subsequent pain complaints: A prospective of 107 subjects sustaining whiplash injury. Nordic Journal of Psychiatry. 49(4), 293–299. DOI: 10.3402/ejpt.v2i0.5652.
- Duckworth, M. P., & Iezzi, T. (2005). Chronic pain and posttraumatic stress symptoms in litigating motor vehicle accident victims. Clinical Journal of Pain. 21(3), 251–261. DOI: 10.3402/ejpt.v2i0.5652.
- Dunmore, E., Clark, D. M., & Ehlers, A. (2001). A prospective investigation of the role of cognitive factors in persistent posttraumatic stress disorder (PTSD) after physical or sexual assault. Behaviour Research and Therapy. 39(9), 1063–1084. DOI: 10.3402/ejpt.v2i0.5652.
- Ehlers, A., & Clark, D. M. (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy. 38(4), 319–345. DOI: 10.3402/ejpt.v2i0.5652.
- Ehlers, A., Mayou, R. A., & Bryant, B. (1998). Psychological predictors of chronic posttraumatic stress disorder after motor vehicle accidents. Journal of Abnormal Psychology. 107(3), 508–519. DOI: 10.3402/ejpt.v2i0.5652.
- Flink, I. K., Mroczek, M. Z., Sullivan, M. J. L., & Linton, S. J. (2009). Pain in childbirth and postpartum recovery: The role of catastrophizing. European Journal of Pain: EJP. 13(3), 312–316. DOI: 10.3402/ejpt.v2i0.5652.
- Garnefski, N., Kraaij, V., & Spinhoven, P. (2001). Negative life events, cognitive emotional regulation, and emotional problems. Personality & Individual Differences. 30(8), 1311–1327. DOI: 10.3402/ejpt.v2i0.5652.
- Garnefski N. Kraaij V. Spinhoven P. Manual for the use of the Cognitive Emotion Regulation Questionnaire. Liederdorp. The Netherlands, 2002
- Gilliam, W., Burns, J. W., Quartana, P., Matsuura, J., Nappi, C., & Wolff, B. (2010). Interactive effects of catastrophizing and suppression on responses to acute pain: A test of an appraisal x emotion regulation model. Journal of Behavioral Medicine. 33(3), 191–199. DOI: 10.3402/ejpt.v2i0.5652.
- Huskisson, E. C. (1974). Measurement of pain. Lancet. 2(7889), 1127–1131. DOI: 10.3402/ejpt.v2i0.5652.
- Jenewein, J., Moergeli, H., Wittmann, L., Buchi, S., Kraemer, B., Schnyder, U, et al.. (2009). Development of chronic pain following severe accidental injury. Results of a 3-year follow-up study. Journal of Psychosomatic Research. 66(2), 119–126. DOI: 10.3402/ejpt.v2i0.5652.
- Jenewein, J., Wittmann, L., Moergeli, H., Creutzig, J., & Schnyder, U. (2009). Mutual influence of posttraumatic stress disorder symptoms and chronic pain among injured accident survivors: A longitudinal study. Journal of Traumatic Stress. 22(6), 540–548. DOI: 10.3402/ejpt.v2i0.5652.
- Jensen, M. P., Karoly, P., & Braver, S. (1986). The measurement of clinical pain intensity: A comparison of six methods. Pain. 27(1), 117–126. DOI: 10.3402/ejpt.v2i0.5652.
- Jermann, F., Van der Linden, M., d'Acremont, M., & Zermatten, A. (2006). Cognitive Emotion Regulation Questionnaire (CERQ): Confirmatory factor analysis and psychometric properties of the French translation. European Journal of Psychological Assessment. 22(2), 126–131. DOI: 10.3402/ejpt.v2i0.5652.
- Keogh E. Asmundson G. J. G. Negative affectivity, catastrophizing and anxiety sensitivity. Understanding and treating fear of pain. Asmundson G. J. G. Vlaeyen J. W. S. Crombez G. Oxford University Press. Oxford, 2004; 91–115.
- Kline R. Principles and practice of structural equation modeling2nd ed. Guilford Press. New York, 2005
- Koren D. Arnon I. Klein E. Acute stress response and posttraumatic stress disorder in traffic accident victims: A one-year prospective, follow-up study. American Journal of Psychiatry. 1999; 156(3): 367–373.
- Liedl, A., O'Donnell, M., Creamer, M., Silove, D., McFarlane, A., Knaevelsrud, C, et al.. (2010). Support for the mutual maintenance of pain and post-traumatic stress disorder symptoms. Psychological Medicine. 40(7), 1215–1223. DOI: 10.3402/ejpt.v2i0.5652.
- MacKinnon, D. P., Lockwood, C. M., & Williams, J. (2004). Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 39(1), 99–128. DOI: 10.3402/ejpt.v2i0.5652.
- Martin, R. C., & Dahlen, E. R. (2005). Cognitive emotion regulation in the prediction of depression, anxiety, stress, and anger. Personality and Individual Differences. 39(7), 1249–1260. DOI: 10.3402/ejpt.v2i0.5652.
- McLean, S. A., Clauw, D. J., Abelson, J. L., & Liberzon, I. (2005). The development of persistent pain and psychological morbidity after motor vehicle collision: Integrating the potential role of stress response systems into a biopsychosocial model. Psychosomatic Medicine. 67(5), 783–790. DOI: 10.3402/ejpt.v2i0.5652.
- Merskey H. Bogduk N. Classification of chronic pain: Descriptions of chronic pain syndromes and definitions of pain terms2nd ed. IASP Press. Seattle WA, 1994; 2007
- Nevitt, J., & Hancock, G. R. (2001). Performance of bootstrapping approaches to model test statistics and parameter standard error estimation in structural equation modeling. Structural Equation Modeling. 8(3), 353–377. DOI: 10.3402/ejpt.v2i0.5652.
- Norman, S. B., Stein, M. B., Dimsdale, J. E., & Hoyt, D. B. (2008). Pain in the aftermath of trauma is a risk factor for post-traumatic stress disorder. Psychological Medicine. 38(4), 533–542. DOI: 10.3402/ejpt.v2i0.5652.
- Norton, P. J., & Asmundson, G. J. (2003). Amending the fear-avoidance model of chronic pain: What is the role of physiological arousal?. Behavior Therapy. 34(1), 17–30. DOI: 10.3402/ejpt.v2i0.5652.
- O'Donnell, M. L., Creamer, M., Bryant, R., Schnyder, U., & Shalev, A. (2006). Posttraumatic stress disorder following injury: Assessment and other methodological considerations. In G. Young, A. Kane, & K. Nicholson. Psychological knowledge in court: PTSD, pain, and TBI. (pp. 70–84.). New York: Springer.
- O'Donnell, M. L., Elliott, P., Wolfgang, B. J., & Creamer, M. (2007). Posttraumatic appraisals in the development and persistence of posttraumatic stress symptoms. Journal of Traumatic Stress. 20(2), 173–182. DOI: 10.3402/ejpt.v2i0.5652.
- Otis, J. D., Keane, T. M., & Kerns, R. D. (2003). An examination of the relationship between chronic pain and post-traumatic stress disorder. Journal of Rehabilitation Research and Development. 40(5), 397–405. DOI: 10.3402/ejpt.v2i0.5652.
- Otis J. D. Pincus D. B. Keane T. M. Comorbid chronic pain and posttraumatic stress disorder across the lifespan: A review of theoretical models. Psychological knowledge in court: PTSD, pain, and TBI. Young G. Kane A. W. Nicholson K. Springer Science & Business Media. New York, 2006; 242–268.
- Preacher, K. J., & Hayes, A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behaviour Research Methods. 40(3), 879–891. DOI: 10.3402/ejpt.v2i0.5652.
- Price, D. D., McGarath, P. A., Rafii, A., & Buckingham, B. (1983). The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain. 17, 45–56. DOI: 10.3402/ejpt.v2i0.5652.
- Schnyder, U., Wittmann, L., Friedrich-Perez, J., Hepp, U., & Moergeli, H. (2008). Posttraumatic stress disorder following accidental injury: Rule or exception in Switzerland?. Psychotherapy and Psychosomatics. 77(2), 111–118. DOI: 10.3402/ejpt.v2i0.5652.
- Scott, J. C., & Huskisson, E. C. (1974). Graphic representation of pain. Pain. 2(2), 175–184. DOI: 10.3402/ejpt.v2i0.5652.
- Scrimshaw, S. V., & Maher, C. G. (2001). Responsiveness of visual analogue and McGill Pain Scale Measures. Journal of Manipulative and Physiological Therapeutics. 24(8), 501–504. DOI: 10.3402/ejpt.v2i0.5652.
- Sharp, T. J., & Harvey, A. G. (2001). Chronic pain and posttraumatic stress disorder: Mutual maintenance?. Clinical Psychology Review. 21(6), 857–877. DOI: 10.3402/ejpt.v2i0.5652.
- Sherman, J. J., & Ohrbach, R. (2006). Objective and subjective measurement of pain: Current approaches for forensic applications. In: G. Young, A. W. Kane, & K. Nicholson. Psychological knowledge in court: PTSD, pain, and TBI. (pp. 193–211.). New York: Springer Science & Business Media.
- Strulov, L., Zimmer, E. Z., Granot, M., Tamir, A., Jakobi, P., & Lowenstein, L. (2007). Pain catastrophizing, response to experimental heat stimuli, and post-cesarean section pain. The Journal of Pain. 8(3), 273–279. DOI: 10.3402/ejpt.v2i0.5652.
- Sullivan, M. J., Bishop, S. R., & Pivik, J. (1995). The Pain Catastrophizing Scale: Development and validation. Psychological Assessment. 7(4), 524–532. DOI: 10.3402/ejpt.v2i0.5652.
- Sullivan, M. J., Thibault, P., Simmonds, M. J., Milioto, M., Cantin, A. P., & Velly, A. M. (2009). Pain, perceived injustice and the persistence of post-traumatic stress symptoms during the course of rehabilitation for perceived whiplash injuries. Pain. 145(3), 325–331. DOI: 10.1016/j.pain.2009.06.031
- Sullivan, M. J., Thorn, B., Haythornthwaite, J. A., Keefe, F. J., Martin, M., Bradley, L. A, et al.. (2001). Theoretical perspectives on the relation between catastrophizing and pain. Clinical Journal of Pain. 17(1), 52–64. DOI: 10.3402/ejpt.v2i0.5652.
- Villano, C. L., Rosenblum, A., Magura, S., Fong, C., Cleland, C., & Betzler, T. F. (2007). Prevalence and correlates of posttraumatic stress disorder and chronic severe pain in psychiatric outpatients. Journal of Rehabilitation Research and Development. 44(2), 167–177. DOI: 10.3402/ejpt.v2i0.5652.
- Vlaeyen, J. W., & Linton, S. J. (2000). Fear-avoidance and its consequences in chronic musculoskeletal pain: A state of the art. Pain. 85(3), 317–332. DOI: 10.3402/ejpt.v2i0.5652.
- Weathers, F. W., Keane, T. M., & Davidson, J. (2001). Clinician-administered PTSD scale: A review of the first ten years of research. Depression and Anxiety. 13(3), 132–156. DOI: 10.3402/ejpt.v2i0.5652.