Abstract
Background: Injured trauma victims are at risk of developing Posttraumatic Stress Disorder (PTSD) and other post-trauma psychopathology. So far, interventions using cognitive behavioral techniques (CBT) have proven most efficacious in treating early PTSD in highly symptomatic individuals. No early intervention for the prevention of PTSD for all victims has yet proven effective. In the acute psychosocial care for trauma victims, there is a clear need for easily applicable, accessible, cost-efficient early interventions.
Objective: To describe the design of a randomized controlled trial (RCT) evaluating the effectiveness of a brief Internet-based early intervention that incorporates CBT techniques with the aim of reducing acute psychological distress and preventing long-term PTSD symptoms in injured trauma victims.
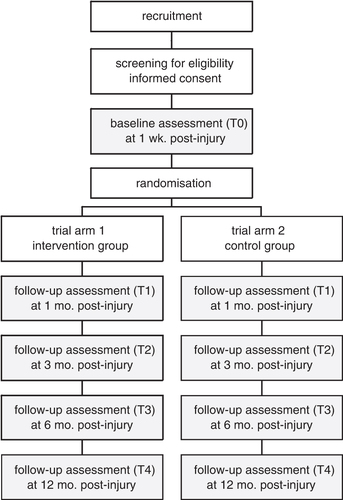
Method: In a two armed RCT, 300 injured trauma victims from two Level-1 trauma centers in Amsterdam, the Netherlands, will be assigned to an intervention or a control group. Inclusion criteria are: being 18 years of age or older, having experienced a traumatic event according to the diagnostic criteria of the DSM-IV and understanding the Dutch language. The intervention group will be given access to the intervention's website (www.traumatips.nl), and are specifically requested to login within the first month postinjury. The primary clinical study outcome is PTSD symptom severity. Secondary outcomes include symptoms of depression and anxiety, quality of life, and social support. In addition, a cost-effectiveness analysis of the intervention will be performed. Data are collected at one week post-injury, prior to first login (baseline), and at 1, 3, 6 and 12 months. Analyses will be on an intention-to-treat basis.
Discussion: The results will provide more insight into the effects of preventive interventions in general, and Internet-based early interventions specifically, on acute stress reactions and PTSD, in an injured population, during the acute phase after trauma. We will discuss possible strengths and limitations.
Victims of traumatic injury are prone to several psychiatric sequelae of their traumatic exposure. One to six months postinjury, reported rates of posttraumatic stress disorder (PTSD) vary from 17.5% to 42% (O'Donnell, Creamer, Bryant, Schnyder, & Shalev, Citation2003). Comorbidity is very prevalent, with rates of major depressive disorder (MDD) up to 53%, rates of anxiety disorder other than PTSD of 25%, and rates of substance use disorder of 20% in injured patients with a PTSD diagnosis.
So far, interventions aiming for the prevention of post-trauma psychopathology have not proven effective. One of the most frequently applied early interventions in the last decades was the trauma-focused psychological Critical Incident Stress Debriefing or Management (CISD or CISM; Mitchell, Citation1983). Research has shown that CISD is not efficacious in preventing PTSD, and can even increase the risk for PTSD symptoms (Rose, Bisson, Churchill, & Wessely, Citation2002; Sijbrandij, Olff, Reitsma, Carlier, & Gersons, 2006). It has been suggested that its emphasis on expressing emotions related to the trauma may exacerbate and sustain arousal, which may cause PTSD symptoms to escalate (Sijbrandij et al., Citation2006). Current PTSD guidelines advocate against the use of these trauma-focused early interventions for everyone involved in the traumatic event (National Institute for Clinical Excellence (NICE), Citation2005; Impact, Citation2007). Furthermore, in a recent Cochrane review, the authors found no convincing evidence that psychosocial interventions can prevent psychological, social, or physical disability after traumatic injury (De Silva et al., Citation2009).
Early psychotherapeutic treatments based on trauma-focused cognitive behavioral therapy (TF-CBT) have consistently shown efficacy in the treatment of Acute Stress Disorder (ASD) and acute PTSD (see Roberts, Kitchiner, Kenardy, & Bisson, Citation2009, for a meta-analysis). TF-CBT techniques include psychoeducation about individual reactions to traumatic events, stress management techniques, in vivo, and imaginal exposure, and cognitive restructuring. TF-CBT for ASD or acute PTSD is typically delivered after a minimum of 2 weeks postinjury and consists of 4 to 5 sessions. More recently, briefer versions of TF-CBT, aimed at the prevention of PTSD in less symptomatic individuals have been developed. A recent pilot feasibility study showed positive results in offering a single imaginal exposure therapy session to injured emergency department victims within 24 hours after trauma: compared to assessments only, patients in the intervention condition were rated lower on clinician-rated global severity of symptoms (Rothbaum et al., Citation2008). Techniques from CBT have also been successfully implemented in Internet-based preventive interventions for depressive symptoms in adolescents (Van Voorhees et al., Citation2009), mood problems in the workplace (Billings, Cook, Hendrickson, & Dove, Citation2008), and for enhancing stress management and promoting healthy behaviors in college students (Chiauzzi, Brevard, Thum, Decembrele, & Lord, Citation2008).
Following largescale, or even individual, traumatic incidents, adequate delivery of mental health services can be impeded by many practical, and financial factors. Especially in considering preventive mental health strategies, there is only a small time window and delivering the needed services to those affected can be time consuming and costly. The Internet may be a useful media in delivering early interventions to recently trauma-exposed populations. It is possible to use the interactivity of the Internet to tailor interventions to specific needs, and for users to access them whereever and whenever they please. With rapidly expanding evidence, e-Mental Health interventions are considered a cost-effective alternative for traditional face-to-face interventions (Kaltenthaler et al., Citation2006). Several Internet-based interventions have demonstrated feasibility (Litz, Williams, & Wang, Citation2004) and efficacy (Hirai & Clum, Citation2005; Lange et al., Citation2003) in the treatment of chronic (symptoms of) PTSD. Yet, few studies have used the Internet as a media for preventive interventions for PTSD. So far, only one pilot study of a preventive Internet-based intervention that addresses mental health (among which PTSD) and substance abuse in disaster populations is documented (Ruggiero et al., 2006). Recently, the design and content of Afterdeployment.org, a web-based self-care management program for military personnel returning from Afghanistan and their families, was published (CitationRuzek, 2011). Primarily meant to use parallel or as an addition to psychological treatment, the program could also be used in an early post-trauma context to supplement face-to-face preventive help.
We created a brief, Internet-based early intervention, named Trauma TIPS. The intervention fits within a universal prevention strategy, aimed at an unselected trauma-affected population (i.e., injured trauma victims). The main aim of Trauma TIPS is to decrease acute levels of distress, anxiety, and arousal, and thereby preventing the development of PTSD symptoms, by offering information on successful coping and instructions for selfexposure to fearful situations to prevent avoidance behavior and by providing stress management techniques to increase selfcontrol of acute arousal symptoms. Another key element of the intervention is stimulating seeking social support. Below, we will describe these elements in more detail.
Psychoeducation
Information constitutes an important element in the Trauma TIPS intervention. In many mental health interventions, patients are provided with psychoeducation to increase their knowledge of their condition and change their attitudes and skills in improving their health (Creamer & O'Donnell, Citation2008). Psychoeducation alone was not found effective in preventing PTSD (see Wessely et al., Citation2008, for a review). To explain this, it is suggested that only listing possible stress reactions after trauma could sensitise victims. Psychoeducation should entail constructive information to stimulate the expectancy of resilience and to promote help seeking (Wessely et al., Citation2008). In the Trauma TIPS intervention, psychoeducation is conveyed through patient models and in textual “tips”. The emphasis is on recovery, transferring knowledge on successful coping and how to pick up normal routine, instead of focusing on the traumatic event, or symptoms. Information is also provided where to seek contact if symptoms remain over the next weeks.
In vivo exposure
With in vivo exposure, the individual exposes himself to a frightening stimulus to diminish the anxiety response and to counteract avoidance behavior (Foa, Keane, Friedman, & Cohen, 2009). The vivo exposure has been thoroughly studied in the early treatment of injury victims with ASD and acute PTSD (Bryant, Harvey, Dang, Sackville, & Basten, 1998; Bryant, Moulds, Guthrie, & Nixon, Citation2003; Bryant, Moulds, Guthrie, & Nixon, Citation2005; Bisson, Shepherd, Joy, Probert, & Newcombe, 2004). In the Trauma TIPS intervention, tips for in vivo exposure exercises are presented in the videos: the patient models explain and show how they gradually encountered activities and situations that provoked anxiety, which decreased after a few times.
Relaxation
Relaxation therapy is not regarded as an effective stand-alone treatment for PTSD, but is used as an anxiety-reducing technique within CBT treatments for ASD and PTSD to reduce and regain control over physical arousal and distress (Bisson et al., Citation2004; Bryant et al., Citation1998; Foa et al., Citation2009; Sijbrandij et al., Citation2007). In our intervention, instructions for stress management techniques (relaxation and breathing retraining exercises) are presented in two audio clips of approximately 7 min duration each: (1) “Muscle relaxation” focuses on progressive muscle relaxation through breathing retraining; (2) “Safe place” is an exercise that focuses on decreasing stress or tension levels by imagining a safe and secure place while retraining breathing.
Social support
Perceived lack of social support is a strong predictor for chronic PTSD (Brewin, Andrews, & Valentine, Citation2000; Ozer, Best, Lipsey, & Weiss, Citation2003). Positive social support is also found to enhance psychosocial adjustment after trauma (see, among others, CitationForbes & Roger, 2011; King, King, Fairbank, Keane, & Adams, Citation1998). Promoting social support is an integral part of the Trauma TIPS intervention, both as textual coping advice (a “tips” section) and shown by the patients models (i.e., when anxious or distressed, a patient model calls a friend). The intervention also features a forum for peer support which allows patients to write to communicate with other trauma survivors about their experiences.
In this study, we describe the design of a RCT evaluating the effectiveness of our brief early intervention.
Method
Participants
Our study population will consist of patients receiving medical treatment for acute physical injuries at the Level-1 trauma centers of the Academic Medical Center (AMC) and Free University Medical Center (VUmc) hospitals in Amsterdam, the Netherlands. Inclusion criteria are: having sustained physical injuries from a traumatic event meeting the A1-Criterion of PTSD of the DSM-IV (American Psychiatric Association, Citation2000), aged 18 years of age or older, and mastery of the Dutch language. Exclusion criteria are: being injured due to deliberate selfharm, suffering from an organic brain condition, current psychotic symptoms, or disorder, bipolar disorder or depression with psychotic features, moderate to severe traumatic brain injury (according to the Glasgow Coma Scale score of less than 13; Teasdale & Jennett, Citation1974), and permanently residing outside the Netherlands.
Study design
In our RCT, participants will be randomized to the Trauma TIPS intervention group or a control group without the intervention. Randomization is on a 1:1 basis, stratified for center, using varying block sizes. The randomization and allocation of patients is done by an independent research worker with no further role in the data collection process. The study protocol has been reviewed and approved by the Medical Ethics Committees of the AMC hospital (registration no. 05-054# 05.17.0504) and VUmc hospital (registration no. 06/039).
Intervention
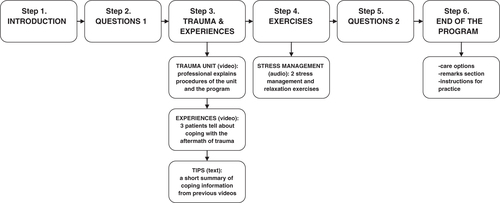
The Trauma TIPS intervention is featured on an interactive website (www.traumatips.nl), created and owned by the authors from the Research Group Psychotrauma The intervention consists of six steps (see ). Step 1, “Introduction and log-in”, highlights the goal of the program and provides basic instructions. In step 2, patients rate their current levels of anxiety and arousal on two Visual Analogue Scales (VASs). The third step, “Trauma and Experiences”, shows videos of the surgical head of the trauma center, explaining the procedures at the center and the purpose of the program, and of three patient models, who briefly tell about their experiences after their injury. Patients are free to watch any, every, or no videos. At the end of this step, a short textual summary is provided of five tips for coping with common physical and psychological reactions after injury or trauma. The tips correspond to the information and instructions in the patient videos. Step 4 presents two audio clips with instructions for stress management techniques. Patients are free to perform the exercises at will. In step 5, patients again rate their anxiety and arousal on two VASs. At the end of the program (step 6), patients can give suggestions or remarks about the program or contact the research team by email, and obtain regular contact information for assistance or professional help. Via a link to a moderated web forum, patients can share experiences for peer support. The total program takes about 30 min to complete. Elaborate descriptions of the key principles and the design of the Internet program can be found elsewhere (CitationMouthaan, Sijbrandij, & Olff, 2010; CitationMouthaan et al., 2011; Sijbrandij, Mouthaan, & Olff, Citation2008).
The patients in the control condition are not offered access to the Trauma TIPS intervention, but are allowed standard care, as are all patients in the study. Standard care consists of incidental, non-protocollized talks with trauma center personnel, or a patient's general physician (GP). The frequency of these contacts and other professional care will be registered throughout the participation process.
Procedure
Adult injury patients are selected from the hospital registries and contacted inhospital (when admitted) or via telephone (when discharged) within 72 hours postinjury to assess eligibility based on language skills and adverse medical or psychiatric conditions. After informed consent, a baseline assessment (T0) of clinically diagnosed and self-reported symptoms of PTSD, depression, and anxiety, coping behavior, and social support takes place at ca. 1 week postinjury. At 1 month (T1), 3 months (T2), 6 months (T3), and 12 months (T4) post-injury, follow-up clinical and self-report assessments of current psychopathology are performed. explores an overview of the instruments per assessment. All assessments take place at the outpatient clinic of the Center for Anxiety Disorders, AMC, at bedside (in case of hospital stay), or at the private home of the patient.
Table 1. Overview of instruments per assessment time point
Patients allocated to the intervention group to receive personal log-in codes to enter the intervention's website, along with instructions to perform the intervention at will. To test a possible practical application of the intervention in a hospital environment, hospitalized patients, and patients without access to the Internet or a personal computer are visited by research assistants with a laptop. Because we aim at preventing (rather than treating) PTSD symptoms, patients are specifically instructed to log on within the first month after their injury. All interviewers will be qualified clinicians or Masters-level psychology students, trained by the research groups who developed the Dutch versions of the clinical interviews (i.e., M.I.N.I. and CAPS, see Assessments). Patients will be instructed to withhold information regarding their randomization outcome from the interviewers to ensure blindness for condition. Any questions about the intervention or the randomization process can be addressed to the independent researcher in charge of the randomization. The independent researcher keeps track of the logins of the patients. Electronic and telephone reminders will be sent to encourage (early) login. shows the trial's flow chart.
Assessments
provides an overview of the instruments used at the individual assessments. We will describe the instruments in more detail below.
Clinical assessments
Demographic and trauma variables
Basic demographic and trauma-related information, for example, age, sex, mechanism of injury, Injury Severity Score (ISS; Baker, O'Neill, Haddon, Jr., & Long, 1974), and Glasgow Coma Scale (GCS; Teasdale & Jennett, Citation1974), are obtained from the hospital registries during the initial selection of participants. Further data on demographics, such as education and marital status, and specifics of the traumatic event will be collected during the first contact with the patients. The ISS is an anatomical scoring system that provides an overall severity score for patients with multiple injuries. The ISS index ranges from 0 (no injury) to 75 (unsurvivable injury) with a score of 16 and higher indicating severe injury (CitationCopes et al., 2011). The Glasgow Coma Scale (GCS) is a neurological scale to record level of consciousness and consists of three parameters: Best Eye Response (four grades), Best Verbal Response (five grades), Best Motor Response (six grades). Resulting scores are between 3 (deep unconsciousness) and 15 (fully conscious). In general, brain injury is classified as: Severe (GCS ≤ 8), Moderate (GCS 9-12) and Mild (GCS 13-15) (Teasdale & Jennett, Citation1974).
Clinician Administered PTSD Scale
The Clinician Administered PTSD Scale counts as the golden standard to establish a PTSD diagnosis (CAPS; Blake et al., 1995). It is a 30-item structured interview that corresponds to the DSM-IV criteria for PTSD. The CAPS can be used to make a current or life-time diagnosis or to assess symptoms over the past week. By adding frequency and intensity (both ranging from 0 to 4) of intrusion, avoidance, and hyperarousal symptoms, the symptom severity or diagnosis of PTSD as a whole can be determined. The internal consistency of the scales in the Dutch translation of the CAPS is good to excellent; with alpha's of .63 for reexperiencing, .78 for avoiding and numbing, .79 for hyperarousal and .89 for all 17 core PTSD symptoms (Hovens et al., Citation1994).
M.I.N.I. International Neuropsychiatric Interview
The M.I.N.I. International Neuropsychiatric Interview-Plus (M.I.N.I.-Plus version 5.0; Sheehan et al., Citation1998) is used to diagnose mood disorders (i.e., major depressive episode, (hypo-)manic episode), anxiety disorders (i.e., panic disorder, social phobia, generalized anxiety disorder), alcohol, and other substance abuse and psychotic disorders. Each module starts with screening questions which, if positive, lead to further examination of the criteria for a specific diagnosis. For purposes of this study, a module on ASD was created by authors JM and MS, based on DSM-IV diagnostic criteria. The M.I.N.I.-Plus has reasonable to good interrater reliability (Cohen's kappa=.43 for current drug dependence to .84 for major depressive episode) and reasonable to very good concurrent validity with the SCID-P (Cohen's kappa=.43 for current drug dependence to .90 for major anorexia; (Sheehan et al., Citation1998). Research on the validation of the Dutch translation of the M.I.N.I.-Plus is currently being performed (Van Vliet & De Beurs, Citation2007).
Self-report measures
Impact of Events Scale-Revised
The Impact of Events Scale-Revised (IES-R; Weiss & Marmar, Citation1997) is a 22-item questionnaire that assesses the severity of PTSD symptoms of intrusion (eight items), avoidance (eight items), and hyperarousal (six items). Items are scored on a 5-point scale, from 0 (not at all) to 4 (extremely), corresponding to how distressing each item has been in the last week. Total scores range from 0 to 88 with higher scores representing more severe symptoms. The subscales were found to have a high degree of intercorrelation (r's=.52–87) and high internal consistency (Intrusion: Cronbach's alpha=.87–94; Avoidance: Cronbach's alpha=.84–87; Hyperarousal: Cronbach's alpha=.79–91; (Weiss & Marmar, Citation1997; Creamer, Bell, & Failla, Citation2003). The validation of the Dutch version of the IES-R is currently in preparation for publication by the authors JM, MS and MO.
Hospital Anxiety and Depression Scale
The severity of depressive and anxiety symptoms is assessed using the Hospital Anxiety and Depression Scale (HADS; Zigmond & Snaith, Citation1983). The items in the two subscales depression (seven items) and anxiety (seven items) are scored on a 4-point scale from 0 to 3. Total scores per subscale range from 0 to 21, with higher scores indicating greater symptomatology. The test-retest reliability of the two scales is high (Pearson's r's=.86 and .91; Spinhoven et al., Citation1997).
Quality of life and functional status
Quality of life and functional status will be assessed using the World Health Organization Quality of Life-Abbreviated scale (WHOQOL-Bref; WHOQOL GROUP, 1998) and the Euroqol 6-Dimensions (EQ-6D; Hoeymans, Van, & Westert, 2005). The WHOQOL-Bref is a 26-item questionnaire measuring QOL on four domains: physical health (seven items), psychological health (six items), social relationships (three items), and environment (eight items). Items are scored on 5-point scales from 1 (worse outcome) to 5 (best outcome). Total scores range from 4 to 20 with higher scores indicating better QOL. The EQ-6D is based on the earlier EQ-5D (Brooks, Citation1996), a generic measure of health status that provides a simple descriptive profile. The original EQ-5D dimensions of mobility, selfcare, usual activities, pain/discomfort, and anxiety/depression are supplemented by a dimension on cognitive functioning (memory, concentration, and coherence, IQ). All dimensions are single items with three possible answers. The EQ-5D provides an index value for health states. It is a valid and frequently used instrument for assessing generic QOL and health status (Dolan, Citation1997).
Coping
The Dutch questionnaire “Utrechtse Coping Lijst” (UCL; Schreurs, Van De Willege, Tellegen, & Graus, 1993) assesses coping behavior when confronted with problems or demanding events. It has 47 items in seven scales: active approach (seven items), palliative reaction (eight items), avoidance (eight items), seeking social support (six items), passive reaction pattern (seven items), expression of emotions (three items), and reassuring thoughts (five items). All items are rated on 4-point scales from 1 (seldom or never) to 4 (very often). High scores correspond with making use of the concerning coping styles. The internal consistencies of the scales are good, with Cronbach's alpha's from 0.64 to 0.82 (Schreurs et al., Citation1993).
Social support
Social support is measured using the Dutch questionnaire “Sociale Steun Lijst-Discrepanties’ (SSL-d; CitationVan Sonderen, 2011). It assesses satisfaction with received social support, more specific the extent to which the received support equals the needs of the individual. The SSL-d features 34 items in six subscales: everyday emotional interactions (four items), emotional support during problems (eight items), appreciation support (six items), instrumental interactions (seven items), social companionship (five items), and informative support (four items). Answers ranged from 1 (would like it to happen more often) to 4 (happens too often, would like less). Items are summed for total scale scores (range 0–136), with high scores corresponding to more satisfaction with experienced social support. The reliability of the scales is good (Cronbach's alpha's: 0.83–0.96; CitationVan Sonderen, 2011).
Costs associated with psychiatric illness
The TiC-P (Trimbos/iMTA questionnaire for Costs associated with Psychiatric illness; Hakkaart-Van Roijen, Van Straten, Donker, & Tiemens, 2002) is administered to compare direct and indirect costs of possible psychopathology between groups. Direct costs are measured by assessing the frequency of contacts with mental health care professionals (i.e., GP, psychologist, and social worker). Medication and hospital or clinic admissions for mental health problems are also part of direct costs. Indirect costs are calculated as production losses due to the effects of psychological problems by the Short Form Health and Labor Questionnaire (SF-HLQ; Van Roijen, Essink-Bot, Koopmanschap, Bonsel, & Rutten, Citation1996), which includes absence from paid work, production losses without absence from paid work, and hindrance in paid and unpaid work.
Online assessments
Pre- and post-intervention anxiety and arousal
Anxiety and arousal during the intervention are assessed using two pre- and two post-intervention VASs featured in the intervention (see subparagraph intervention). Patients in the intervention condition are asked to indicate their current levels of anxiety and arousal from 0 (no anxiety or arousal) to 100 (worst anxiety or arousal).
Web-related behavior
Every step or click made in the intervention is automatically logged for the purpose of evaluating the influence of web-related behavior on the effectiveness of the program. Besides the number of logins, we also register the total time logged in, and the number of times and total time spent on the videos and the exercises.
Sample size
The main outcome measure to assess the intervention's effectiveness in preventing PTSD symptoms is the difference in the total CAPS score between the intervention and control condition at 12 months post-injury. We expect to find a small to medium effect size of Cohen's d=.35, which is equivalent to a difference of 5.5 points on the CAPS. To demonstrate this difference, we require a total of 134 patients or more in each group (alpha = 5%, power = 80%). This calculation is based on a standard deviation (SD) of 16 for CAPS scores, derived from a published study using the CAPS as a continuous outcome in a similar research population (Conlon, Fahy, & Conroy, Citation1999). Anticipating possible attrition of study participants, we aim for 150 patients in each group.
Data analysis
Descriptive statistics will be used to describe and examine differences in demographic, trauma related, and baseline clinical characteristics between the two intervention arms. The main analysis to assess the intervention's effectiveness on preventing PTSD is the difference in CAPS scores between the two arms of the trial. Differences in scores at 12 months will be compared using an analysis of covariance with the baseline assessment as a covariate. In addition, a repeated measurement analysis will be performed in which the CAPS scores at 1, 3 and 6 months will be included to describe trends over time. All analyses will be on an intention-to-treat basis. Results are expressed as differences in scores between the two arms together with 95% confidence intervals (CI). Reductions on the VASs are measured by scoring the differences on arousal and anxiety prior to and after the intervention (VAS scores before – VAS scores after). All analyses will be performed using SPSS 18.0.
Discussion
This RCT represents a unique study of an Internet-based early intervention aimed at reducing acute distress levels and preventing the development of PTSD symptoms. We expect that it will generate new scientific information on the effectiveness of preventive interventions in general, Internet-based interventions, and CBT techniques specifically, in the acute phase following trauma, targeted at a trauma-affected sample with varying levels of injury.
From a practical standpoint, several possible limitations may affect the trial. Patients can encounter technical difficulties in performing the Internet intervention. We anticipated for these difficulties by pilot testing the functionality of the program and its individual steps (CitationMouthaan et al., 2011). At the end of the intervention, patients can (electronically or otherwise) contact the research team about the content or working of the program. The research team will also hold weekly updates of the functionality of the program, to ensure that any problems with the website are resolved quickly. Another problem may be the accessibility of our web program. An unknown proportion of patients do not own a personal computer with private access to the Internet. These patients will be visited by a research assistant to perform the intervention on a laptop. Finally, some patients will not be capable to perform the intervention, such as patients with insufficient understanding of the Dutch language, patients with little computer skills, or patients who are physically unable to perform a computerized intervention (e.g., severely injured Intensive Care patients).
As a result of the information and advice provided in the intervention, it is possible that patients in the intervention condition will actually show more use of mental health care for psychological symptoms after their injury than control patients. It could also be that the intervention increases awareness of psychological well-being after trauma, which could possibly result in higher symptomatology within the intervention group. Although our pilot results indicated that the intervention did not aggravate acute anxiety or stress symptoms in recently injured trauma victims (CitationMouthaan et al., 2011), the RCT will show us the longer-term effects.
A particular strength of the trial is that it is embedded within a larger ongoing prospective cohort study (Trauma TIPS) which started in 2005 with the general aim to study the incidence and prediction of psychiatric symptoms in 2,000 injured trauma victims. Advantageously, many of the practical necessities are already arranged, such as having trained staff for the inclusion of research participants, and for performing the assessments. In addition, we are better able to realistically predict the rate of inclusion and the amount of time needed. A steady 15 patients per center per month are included in the prospective trial. Because in the RCT patients have to be open to randomization to either the intervention or the control group and be able to participate within the first month after trauma, we expect to realistically include 10 patients per center per month, with a total inclusion time of 15 months.
If the intervention proves effective in counteracting early distress symptoms and consequently preventing PTSD, it may be implemented in the standard care for trauma patients in Level-1 trauma centers and at emergency departments. In addition, the general public will be informed about the availability of the intervention via posters and leaflets in hospital casualty and emergency departments and in GP waiting rooms and possibly via the media or cross links on other relevant websites. Further, it might be worthwhile to adapt the intervention to other trauma populations, especially considering the current lack of effective interventions available for all trauma survivors irrespective of their symptom levels. The low--threshold nature, easy application, possibilities for wide distribution, and low burden on financial and personnel costs make e-Mental Health solutions promising for the acute psychosocial care for trauma victims. We expect the results of the RCT at the end of 2011.
Conflict of interest and funding
There is no conflict of interest in the present study for any of the authors. Funding for this study is provided by the Netherlands Organization for Health Research and Development (ZonMw), Grant no. 62300038, and by the Achmea Foundation for Victims and Society (Stichting Achmea Slachtoffer en Samenleving).
Dutch full text
Download PDF (203.8 KB)French abstract
Download PDF (16.3 KB)Italian abstract
Download PDF (32.5 KB)German abstract
Download PDF (15 KB)Polish abstract
Download PDF (100.6 KB)Russian abstract
Download PDF (49.2 KB)Spanish abstract
Download PDF (16.1 KB)Turkish abstract
Download PDF (68.6 KB)Ukranian abstract
Download PDF (93.2 KB)References
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders. ( Revised 4th ed.). WashingtonDC: American Psychiatric Association.
- Baker, S. P. O'Neill, B., Haddon, W., Jr., & Long, W. B. (1974). The injury severity score: A method for describing patients with multiple injuries and evaluating emergency care. Journal.of Trauma. 14, 187–196.
- Billings D. W. Cook R. F. Hendrickson A. Dove D. C. A web-based approach to managing stress and mood disorders in the workforce. Journal of Occupational and Environmental Medicine. 2008; 50: 960–968.
- Bisson J. I. Shepherd J. P. Joy D. Probert R. Newcombe R. G. Early cognitive-behavioural therapy for post-traumatic stress symptoms after physical injury. Randomised controlled trial. British Journal of Psychiatry. 2004; 184: 63–69.
- Blake D. D. Weathers F. W. Nagy L. M. Kaloupek D. G. Gusman F. D. Charney D. S, et al.. The development of a clinician-administered PTSD Scale. Journal of Traumatic Stress. 1995; 8: 75–90.
- Brewin C. R. Andrews B. Valentine J. D. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000; 68: 748–766.
- Brooks R. EuroQol: The current state of play. Health Policy. 1996; 37: 53–72.
- Bryant R. A. Harvey A. G. Dang S. T. Sackville T. Basten C. Treatment of acute stress disorder: A comparison of cognitive-behavioral therapy and supportive counseling. Journal of Consulting and Clinical Psychology. 1998; 66: 862–866.
- Bryant R. A. Moulds M. Guthrie R. Nixon R. D. Treating acute stress disorder following mild traumatic brain injury. American Journal of Psychiatry. 2003; 160: 585–587.
- Bryant R. A. Moulds M. L. Guthrie R. M. Nixon R. D. The additive benefit of hypnosis and cognitive-behavioral therapy in treating acute stress disorder. Journal of Consulting and Clinical Psychology. 2005; 73: 334–340.
- Chiauzzi E. Brevard J. Thum C. Decembrele S. Lord S. MyStudentBody-Stress: An online stress management intervention for college students. Journal of Health Communication. 2008; 13: 555–572.
- Conlon L. Fahy T. J. Conroy R. PTSD in ambulant RTA victims: A randomized controlled trial of debriefing. Journal of Psychosomatic Research. 1999; 46: 37–44.
- Copes W. S. Champion H. R. Sacco W. J. Lawnick M. M. Gann D. S. Gennarelli T, et al.. Progress in characterizing anatomic injury. Journal of Trauma. 1990; 30: 1200–1207.
- Creamer M. Bell R. Failla S. Psychometric properties of the Impact of Event Scale-revised. Behavioral Research Therapy. 2003; 41: 1489–1496.
- Creamer M. O'Donnell M. The pros and cons of psychoeducation following trauma: too early to judge?. Psychiatry. 2008; 71: 319–321.
- De Silva, M., Maclachlan, M., Devane, D., Desmond, D., Gallagher, P., Schnyder, U, et al.(2009). Psychosocial interventions for the prevention of disability following traumatic physical injury. Cochrane.Database.System.Review. , CD006422.
- Dolan P. Aggregating health state valuations. Journal of Health Service Research Policy. 1997; 2: 160–165.
- Foa E. B. Keane T. M. Friedman M. J. Cohen J. A. Effective treatments for PTSD. Practice guidelines from the International Society for Traumatic Stress Studies2nd ed. The Guilford Press. New York, 2009
- Forbes A. Roger D. Stress, social support, and fear of disclosure. British Journal of Health Psychology. 2011; 4: 165–179.
- Hakkaart-Van Roijen L. van Straten A. Donker M. Tiemens B. Handleing Trimbos/iMTA questionnaire for Costs associated with Psychiatric illness (TiC-P). instituut voor Medische Technology Assessment, Erasmus Universiteit Rotterdam. Rotterdam, 2002
- Hirai M. Clum G. A. An Internet-based self-change program for traumatic event related fear, distress, and maladaptive coping. Journal of Traumatic Stress. 2005; 18: 631–636.
- Hoeymans N. Van L. H. Westert G. P. The health status of the Dutch population as assessed by the EQ-6D. Quality of Life Research. 2005; 14: 655–663.
- Hovens J. E. Van der Ploeg H. M. Klaarenbeek M. T. Bramsen I. Schreuder J. N. Rivero V. V. The assessment of posttraumatic stress disorder: With the Clinician Administered PTSD Scale: Dutch results. Journal.of Clinical. Psychology. 1994; 50: 325–340.
- Impact. Multidisciplinaire richtlijn voor vroegtijdige psychosociale opvang na rampen, terrorisme en andere schokkende gebeurtenissen. Trimbos-instituut. Utrecht the Netherlands, 2007
- Lange A. van de Ven J. P. Schrieken B. Interapy: treatment of post-traumatic stress via the internet. Cognitive Behavioral Therapy. 2003; 32: 110–124.
- Litz B.T. Williams L. Wang J. A therapist-assisted Internet self-help program for traumatic stress. Professional Psychiatric Research Practice. 2004; 35: 628–634.
- Kaltenthaler, E., Brazier, J., De, N. E., Tumur, I., Ferriter, M., Beverley, C, et al.(2006). Computerised cognitive behaviour therapy for depression and anxiety update: A systematic review and economic evaluation. Health Technology.Assessment. 10, iii, xi–iii,168.
- King L. A. King D. W. Fairbank J. A. Keane T. M. Adams G. A. Resilience-recovery factors in post-traumatic stress disorder among female and male Vietnam veterans: Hardiness, postwar social support, and additional stressful life events. Journal of Personality and Social Psychology. 1998; 74: 420–434.
- Mitchell J. T. When disaster strikes...the critical incident stress debriefing process. Journal of Emergency Medicine. 1983; 8: 36–39.
- Mouthaan J. Sijbrandij M. Olff M. Trauma TIPS: A brief Internet-based early intervention for the Prevention of Posttraumatic Stress Disorder (PTSD) in injured trauma patients. Internet use in the aftermath of trauma. Brunet A. Ashbaugh A. R. Herbert C. F. IOS Press. Amsterdam, 2010; 213–228.
- Mouthaan J. Sijbrandij M. Reitsma J.B. Luitse J.S.K. Goslings J.C. Olff M. Trauma TIPS: an internet-based intervention to prevent posttraumatic stress disorder in injured trauma patients. Journal of Cybertherapy and Rehabilitation. 2011; 4(3): 331–340.
- National Institute for Clinical Excellence (NICE). (2005). Post-traumatic stress disorder; the management of PTSD in adults and children in primary and secondary care. London: Gaskell and the British Psychological Society.
- O'Donnell M. L. Creamer M. Bryant R. A. Schnyder U. Shalev A. Posttraumatic disorders following injury: An empirical and methodological review. Journal of Clinical Psychology Review. 2003; 23: 587–603.
- Ozer E. J. Best S. R. Lipsey T. L. Weiss D. S. Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin. 2003; 129: 52–73.
- Roberts, N. P., Kitchiner, N. J., Kenardy, J., & Bisson, J. (2009). Multiple session early psychological interventions for the prevention of post-traumatic stress disorder. Cochrane Database Systematic Review. , CD006869.
- Rose, S., Bisson, J., Churchill, R., & Wessely, S. (2002). Psychological debriefing for preventing post traumatic stress disorder PTSD. Cochrane.Database.System.Review. , CD000560.
- Rothbaum B. O. Houry D. Heekin M. Leiner A. S. Daugherty J. Smith L. S, et al.. A pilot study of an exposure-based intervention in the ED designed to prevent posttraumatic stress disorder. American Journal of Emergency Medicine. 2008; 26: 326–330.
- Ruzek, J. I. (2011). Bringing Internet-based education and intervention into mental health practice: After deployment.org. European Journal of Psychotraumatology. , 10.3402/ejpt.v2i0.8294.
- Schreurs P. J. G. Van De Willege J. F. Tellegen B. Graus G. M. H. De Utrechtse coping Lijst: UCL Omgaan met problemen en gebeurtenissen. Swets en Zeitlinger. Lisse, 1993
- Sheehan D. V. Lecrubier Y. Sheehan K. H. Amorim P. Janavs J. Weiller E, et al.. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998; 59(Suppl. 20): 22–33.
- Sijbrandij M. Mouthaan J. Olff M. Trauma-TIPS: Eine internetgestützte Intervention zur Prävention von Posttraumatischen Belastungsstörungen bei Patienten mit körperlichen Verletzungen. E-Mental-health: Neue medien in der psychosozialen Versorgung. Bauer S. Kordy H. Springer Publishers. 2008; 51–59.
- Sijbrandij M. Olff M. Reitsma J. B. Carlier I. V. De Vries M. H. Gersons B. P. Treatment of acute posttraumatic stress disorder with brief cognitive behavioral therapy: A randomized controlled trial. American Journal of Psychiatry. 2007; 164: 82–90.
- Sijbrandij M. Olff M. Reitsma J. B. Carlier I. V. Gersons B. P. Emotional or educational debriefing after psychological trauma. Randomised controlled trial. British Journal of Psychiatry. 2006; 189: 150–155.
- Spinhoven P. Ormel J. Sloekers P. P. Kempen G. I. Speckens A. E. van Hemert A. M. A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychological Medicine. 1997; 27: 363–370.
- Teasdale G. Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974; 2: 81–84.
- Van Roijen L. Essink-Bot M. L. Koopmanschap M. A. Bonsel G. Rutten F. F. Labor and health status in economic evaluation of health care. The Health and Labor Questionnaire. International Journal of Technology Assessment Health Care. 1996; 12: 405–415.
- Van Sonderen, E. (2011). Het meten van sociale steun met de Sociale Steun Lijst-Interacties (SSL-i) en Sociale Steun Lijst Discrepanties (SSL-d): een handleiding. Groningen: Noordelijk Centrum voor Gezondheidsvraagstukken.
- Van Vliet I. M. De Beurs E. [The MINI-International Neuropsychiatric Interview. A brief structured diagnostic psychiatric interview for DSM-IV en ICD-10 psychiatric disorders]. Tijdschrift voor de Psychiatrie. 2007; 49: 393–397.
- Van Voorhees B. W. Fogel J. Reinecke M. A. Gladstone T. Stuart S. Gollan J, et al.. Randomized clinical trial of an Internet-based depression prevention program for adolescents (Project CATCH-IT) in primary care: 12-week outcomes. Journal of Developmental and Behavioural Pediatrics. 2009; 30: 23–37.
- Weiss D. S. Marmar C. R. The Impact of Event Scale-Revised. Assessing psychological trauma and PTSD. Wilson J. P. Keane T. M. Guilford Press. New York, 1997; 399–411.
- Wessely S. Bryant R. A. Greenberg N. Earnshaw M. Sharpley J. Hughes J. H. Does psychoeducation help prevent post traumatic psychological distress?. Psychiatry. 2008; 71: 287–302.
- WHOQOL GROUP. (1998). Development of the World Health Organization WHOQOL-BREF Quality of Life Assessment. Psychological Medicine. 28, 551–558.
- Zigmond A. S. Snaith R. P. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica. 1983; 67: 361–370.