Abstract
Introduction: High blood pressure (BP) is a well-known major risk factor for cardiovascular diseases and is a leading contributor to cardiovascular mortality and morbidity worldwide. Reliable population-based BP data from low–middle income countries are sparse.
Objective: This paper reports BP distributions among adults in nine rural populations in five Asian countries and examines the association between high BP and associated risk factors, including gender, age, education, and body mass index.
Methods: A multi-site cross-sectional study of the major non-communicable disease risk factors (tobacco and alcohol use, fruit and vegetable intake, physical activity patterns) was conducted in 2005 in nine Health and Demographic Surveillance System (HDSS) sites in five Asian countries, all part of the INDEPTH Network. In addition to the self-report questions on risk factors, height and weight, and BP were measured during household visits using standard protocols of the WHO STEPwise approach to Surveillance.
Results: In all the study sites (except among men and women in WATCH and among women in Chililab), the mean levels of systolic BP were greater than the optimal threshold (115 mmHg). A considerable proportion of the study populations – especially those in the HDSS in India, Indonesia, and Thailand – had high BP (systolic BP ≥ 140 mmHg or diastolic BP ≥ 90 mmHg or on treatment with BP medications). A more conservative definition of high BP (systolic BP ≥ 160 mmHg or diastolic BP ≥ 100 mmHg) substantially reduced the prevalence rate. The marked differences in the proportion of the populations on high BP medication (range between 0.6 and 10.8%) raised problems in comparing the prevalence of high BP across sites when using the commonly used definition of high BP as in this study. In the four HDSS in Bangladesh, women had a higher prevalence of high BP than men; the reverse was true in the other sites (Chililab, Filabavi in Vietnam; Kanchanaburi, Thailand; and Vadu, India) where men experienced higher prevalence than women. Overweight and obesity were significantly associated with high BP, with odds ratio ranging from two in Chililab to five in Filabavi (both in Vietnam HDSS).
Conclusion: The patterns of BP in these nine cross-sectional surveys were complex, reflecting the fact that the Asian countries are at different stages of the epidemiological transition. Actions to prevent the rise of BP levels are urgently required. An emphasis should be placed on cost-effective interventions to reduce salt consumption in the population as an immediate priority.
Introduction
High blood pressure is a major modifiable risk factor for cardiovascular diseases (CVDs) and a leading cause of the CVD burden worldwide Citation1. The higher the blood pressure, the greater the chance of heart attack, heart failure, stroke, and kidney disease Citation2. High blood pressure is only one of several proven modifiable risk factors for CVDs and decisions about treatment need to be based on overall risk and the presence of other risk factors rather than the level of blood pressure alone. The other major risk factors include tobacco use, heavy alcohol consumption, unhealthy diet, and physical inactivity Citation3. Clustering of risk factors cause a majority of CVD events Citation4Citation5Citation6.
A recent systematic review reported that the prevalence of high blood pressure in low and middle-income countries is reaching the level in high income countries Citation7; approximately half of all CVD in low and middle-income countries is related to high blood pressure Citation8.
Asian countries are undergoing an epidemiological transition with an increasing burden of CVDs and their risk factors Citation9Citation10Citation11. Information on the pattern and trends in blood pressure in these countries is important for health professionals to direct health planning, health resourcing, and public health interventions. Taking advantage of a cross-site study on non-communicable disease risk factors conducted in 2005, this paper reports the pattern of blood pressure among adult men and women in the study settings in nine Health and Demographic Surveillance System (HDSS) sites from five Asian countries Citation12 and examines the association with gender, age, education, and body mass index. The paper also addresses the issue of treatment guidelines in the context of these resource-constrained settings.
2 Methods
The study was based on the WHO STEPwise approach to Surveillance (WHO STEPS). Details have been described elsewhere Citation12Citation13Citation14. Briefly, a cross-sectional study of the major non-communicable disease risk factors (tobacco and alcohol use, fruit and vegetable intake, physical activity patterns) was conducted in 2005 in nine HDSS sites in five Asian countries, all part of the INDEPTH Network (an International Network of field sites for continuous Demographic Evaluation of Populations and Their Health in developing countries), which was established to facilitate linkage of existing demographic field sites Citation15.
In addition to the self-report questions on tobacco and alcohol use, fruit and vegetable intake and physical activity patterns, height and weight, and blood pressure were measured during household visits using standard protocols. Training was undertaken prior to the study start and all sites used the same automated blood pressure measuring devices (Omron M3®). Blood pressure was measured at the right arm at heart level after a period of 10 minutes of rest. Three measurements were taken and the averages of the last two readings were used in the analysis. Strict training protocols for data collectors were adhered to and quality assurance measures were employed to ensure the quality of the data collected.
Both descriptive and analytical statistics were carried out using Stata 10 software (Stata Corporation). Mean blood pressure levels (and 95%CI) were computed. Proportions of high blood pressure using different cut-off points (and their 95%CIs) stratified by age and sex were also calculated. Careful attention was paid to the levels of high blood pressure treatment to understand the comparability of data obtained in these different settings when the standard definition of hypertension was used in defining the proportion of high blood pressure. Multivariable regression modeling was performed to examine the associations between high blood pressure with age, sex, education, and body mass index. A significance level of p<0.05 was used.
2.1 Ethical considerations
The protocol of this study was approved by the Scientific Board of the INDEPTH Network and was also in accordance with the ethics codes of the respective sites. All human subjects in the study were asked for their verbal and written informed consent before data were collected, and all had the right to withdraw from the study at any time.
3 Results
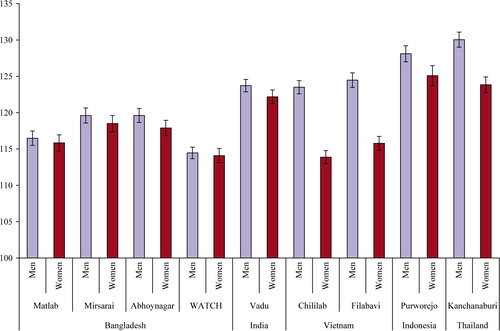
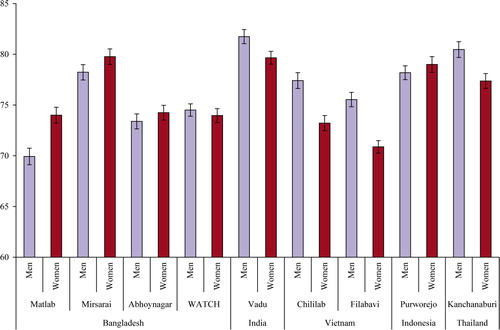
The mean levels of systolic blood pressure (SBP) and diastolic blood pressure (DBP) of the study subjects by site and sex are shown in and . Among men, mean SBP was lowest in one of the sites in Bangladesh and highest in Purworejo, Indonesia; DBP was lowest in Matlab and highest in Vadu. Among women, SBP was lowest in Chililab, Vietnam and highest in Kanchanaburi, Thailand; DBP was lowest in Filabavi, Vietnam and highest in Mirsarai, Bangladesh.
Figure 2. Distribution of diastolic blood pressure (mmHg) and its 95%CI in nine HDSS sites by gender.
The proportion of study subjects who had high blood pressure according to two different cut points are presented for men and women in . When SBP > = 140 mmHg or DBP > = 90 mmHg was used as a cut point, the overall prevalence (men and women combined) ranged from around 15 to 28% of the adult population with one exception where prevalence was 9% in one of the HDSS in Bangladesh. When a higher cut point was used (SBP ≥ 160 mmHg or DBP ≥ 100 mmHg), prevalence halved (ranging from 5 to 15%). A greater proportion of women had high blood pressure than men in the four HDSS in Bangladesh; in the other HDSS, men had a higher prevalence than women.
Table 1. Prevalence (%) of raised blood pressure (95%CI) in nine HDSS sites, by different cut points and gender
shows differences in treatment patterns for raised blood pressure according to blood pressure levels as well as overall treatment. One in 10 of the population in one of the HDSS in Bangladesh (Mirsarai) reported being on anti-hypertensive treatment. In contrast, treatment for raised blood pressure was reported in only 2% of the respondents in Vadu, India and Purworejo, Indonesia. Women reported higher levels of blood pressure treatment than men in almost in all HDSS sites except in the Vietnamese sites where more men reported receiving anti-hypertensive treatment compared with women. Of particular note is the variation in the proportion of the population on anti-hypertensive treatment whose blood pressure was controlled (<140/90). This ranged from less than 1 to 11%.
Table 2. Percent (95%CI)) of men and women on treatment by different blood pressure groups in nine HDSS sites
Multivariable logistic regression models were constructed to analyse the association of high blood pressure with age, gender, education, and body mass index (). The models show that age is a significant determinant of high blood pressure in both men and women. The models also show that while high blood pressure was shown to be significantly more common in men than in women in the two HDSS in Vietnam and Kanchanaburi in Thailand, it was significantly more prevalent in women in the four Bangladeshi sites (Matlab, Mirsarai, Abhoynagar, and WATCH). Overweight (defined as BMI ≥ 25 kg/m2) was shown to be positively associated with high blood pressure in all sites. There was a tendency for increasing levels of education to be associated with increased blood pressure in Matlab and WATCH of Bangladesh.
Table 3. Association (OR and 95%CI) between demographic variables and raised blood pressure (≥140/90 and/or on treatment) in nine HDSS sites
4 Discussions
This study provides information on the patterns of blood pressure among adult populations in countries in Asia which are undergoing the epidemiologic transition. The data are reliable and accurate as the study was conducted within well-functioning HDSSs using standardised WHO STEPS protocols Citation13. The data provide baseline mean population levels of blood pressure for men and women against which future measures of blood pressure within the HDSS framework can be compared. High blood pressure is only one of many modifiable risk factors which contribute to an increased risk of CVD Citation16.
In all the study sites (except among men and women in WATCH and among women in Chililab), the mean levels of SBP were greater than the optimal threshold (i.e. 115 mmHg; ). Suboptimal SBP level (i.e. greater than 115 mmHg) has been estimated to account for 62% of all cerebrovascular disease and 49% of all ischemic heart disease Citation5. This study showed that a considerable proportion of the study populations had raised blood pressure, especially in the sites in Vietnam, Indonesia, Thailand, and India. The overall prevalence of hypertension (blood pressure ≥ 140/90 mmHg) found in this study were higher than reported in other studies in Vietnam, Indonesia Citation17, Thailand Citation18, India Citation19, and Bangladesh Citation20. However these comparisons are hindered because of differences in age structure, variability in definition of hypertension, time of the study, urban versus rural characteristics of the population, and standardisation of blood pressure measurement instruments and procedures.
Another important consideration in comparisons between studies, and time-series studies, relates to the standard and widely used definition of hypertension (SBP ≥ 140 mmHg or DBP ≥ 90 mmHg or on anti-hypertensive treatment). Between 0.6 and 10% of people in these nine HDSS were classified as ‘hypertensive’ based on treatment alone (i.e. blood pressure levels were below 140/90 mmHg). Had these been included, the prevalence would have been up to 10% higher in some of the HDSS. The inclusion of the ‘controlled’ category in the definition of hypertension thus artificially increases prevalence, making comparisons of the burden of high blood pressure between sites/countries or across different time-points invalid, when the treatment patterns are considerably different across different settings. The more people who receive anti-hypertensive treatment and the more the treatment is successful in lowering blood pressure below 140/90 mmHg, the higher the prevalence, according to the standard definition. It is for this reason that changes in mean population levels of blood pressure offer a more accurate measure of change over time.
Our data also confirms that the burden of raised blood pressure depends on the cut-off points used. In fact, there is no clear threshold value which separates hypertensive patients who will experience future cardiovascular events from those who will not. Risk of CVD depends on blood pressure, coexistent risk factors, and whether there is hypertensive damage to target organs Citation21. It would also be inappropriate to assume that up to one-fifth of the adult population in these poor rural sites should be offered treatment. Treatment decisions need to be based on identification individuals at a high risk of disease, not on blood pressure levels alone. Another paper in this supplement shows that a substantial proportion in most study populations already have three or more risk factors for CVD Citation22.
Treatment decisions regarding hypertensive patients based on cardiovascular risk are more cost-effective than those based on blood pressure levels alone, and also improve health outcomes Citation23. Numerous methods for assessing absolute cardiovascular risk have been described Citation21Citation23. Secondary prevention through anti-hypertensive treatments solely may be hard to justify in the absence of primary intervention to promote lower salt-intake in the population aimed at shifting the population distribution of blood pressure to a lower level.
High-risk intervention against CVDs is available for low-resource settings Citation27. Scaling up a multidrug regimen (a statin, aspirin, and two blood-pressure-lowering medicines) could avert 17.9 million deaths worldwide from CVD. This intervention would be directed at people on the basis of overall risk and would include those who have already suffered a heart attack, stroke, or Transient Ischemic Attack (TIA) as well as those whose overall risk is 15% or greater over 10 years. It assumes opportunistic screening, not population screening, and treatment through existing primary health care systems. This intervention, if widely applied, would cost from $0.43 to $0.90 per person per year in low and middle-income countries and meet three-quarters of the proposed global chronic disease goal with only a moderate increase in health expenditure Citation23. Ideally, a combination of population-wide and high-risk preventive strategies need to be implemented Citation24.
This study also revealed that the rates of control of high blood pressure in the study populations appeared to be low. Similar findings have also been reported for in other studies in the region (Citation23Citation25). Factors that may contribute to these poor rates of control include inadequate or inappropriate treatment, unavailability of drugs, insufficient advice from health-care providers, and lack of follow-up Citation25. In many of the countries included in this study, out-of-pocket payments are made for drugs and many are unable to sustain long-term costs. Appropriate guidelines, adapted to local settings are required. The WHO CVD-risk management package for low and medium-resource settings is particularly appropriate for this purpose Citation18. It has been designed for assessment and management of individuals with elevated blood pressure but can also be applied for smoking Citation16.
The strong associations between high blood pressure and gender, age, education, and body mass index have been confirmed in these rural HDSS. Our study also confirmed that overweight and obesity increase the risks of high blood pressure. These findings are in line with many other studies Citation25Citation26Citation27.
In summary, our findings showed that blood pressure in Asian INDEPTH sites is a problem, both because of its high prevalence, high mean levels, and the low rates of control in the population. The patterns of blood pressure from these nine HDSSs are complex to interpret but may reflect that the Asian countries are at different stages of the epidemiological transition. Greater attention to actions to prevent CVD and other chronic diseases in these setting are required. The highest priorities should be the implementation of cost-effective population-wide approaches to lowering the average level of blood pressure in the population. Population-wide interventions to promote less salt-intake in the population will shift the population distribution of blood pressure to lower levels. Individual high-risk approach is also feasible when treatment decisions are based on the risk of disease, rather than on the level of a single risk factor blood pressure. It is to be hoped that the information from this study will help in making planning and policy decisions more rational.
5 Conflict of interest
The authors have declared no conflict of interest
Acknowledgements
The authors would like to acknowledge the INDEPTH Network for financing this work, Dr. Anand Krishnan and Dr. S.K. Kapoor from Ballabgarh HDSS for organising training workshop for this project, the Umeå Centre for Global Health Research, Umeå University, Sweden for supporting the coordination of this supplement, and Dr. Ruth Bonita, who as guest editor for this series of papers, provided substantial and critical scientific input into earlier drafts of this paper.
References
- Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJL. Comparative risk assessment collaborative group: selected major risk factors and global and regional burden of disease. Lancet. 2002; 360: 1347–60.
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JLJr, et al.. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003; 289: 2560–72.
- Poulter N. Global risk of cardiovascular disease. Heart. 2003; 89: 2–5.
- Yu D, Huang J, Hu D, Chen J, Cao J, Li J, Gu D. Association between prehypertension and clustering of cardiovascular disease risk factors among Chinese adults. J Cardiovasc Pharmacol. 2009. May; 53(5):388–400.
- World Health Organization. World Health Report 2002: Reducing Risks, Promoting Healthy Life. Geneva: 2002.
- Kaufman JS , Asuzu MC , Mufunda J , Forrester T , Wilks R , Luke A , et al.. The relationship between blood pressure and body mass index in lean populations. Hypertension. 1997; 30: 1511–6.
- Pereira M, Lunet N, Azevedo A, Barros H. Differences in prevalence, awareness, treatment and control of hypertension between developing and developed countries. J Hypertens. 2009; 27: 963–75.
- Gaziano TA, Reddy KS, Paccaud F, Horton S, Chaturvedi V. Cardiovascular disease. Disease control priorities in developing countries2nd edn. Jamison DT, Measham AR, Breman JB, Alleyene G, Claeson M, Evans DB, Jha P, Mills A, Musgrove POxford University Press. New York, 2006; 645–662.
- Singh RB, Suh IL, Singh VP, Chaithiraphan S, Laothavorn P, Sy RG, et al.. Hypertension and stroke in Asia: prevalence, control and strategies in developing countries for prevention. J Hum Hypertens. 2000; 14: 749–63.
- Minh HV, Byass P, Chuc NT, Wall S. Gender differences in prevalence and socioeconomic determinants of hypertension: findings from the WHO STEPs survey in a rural community of Vietnam. J Hum Hypertens. 2006; 20: 109–15.
- Hoang VM, Byass P, Dao LH, Nguyen TK, Wall S. Risk factors for chronic disease among rural Vietnamese adults and the association of these factors with sociodemographic variables: findings from the WHO STEPS survey in rural Vietnam, 2005. Prev Chronic Dis. 2007; 4: A22.
- Ng N , Minh HV , Juvekar S , Razzaque A , Bich TH , Kanungsukkasem U , et al. Using the INDEPTH HDSS to build capacity for chronic non-communicable disease risk factor surveillance in low and middle income countries. Global Health Action Supplement 1. , 2009, 10.3402/gha.v2i0.1984.
- World Health Organization. WHO STEPS surveillance manual: the WHO STEPwise approach to chronic disease risk factor surveillance. Geneva: World Health Organization. 2005.
- Bonita R, de Courten M, Dwyer T, Jamrozik K, Winkelmann R, Armstrong T. Surveillance of risk factors for noncommunicable diseases: The WHO STEPwise approach. World Health Organization. Geneva, 2002
- INDEPTH Network. Population and health in developing countries. OttawaCanada: INDEPTH Network., IDRC; 2002.
- World Health Organization. WHO CVD– risk management package for low- and medium-resource settings. Geneva: WHO. 2002.
- Ng N, Minh HV, Tesfaye F, Bonita R, Byass P, Stenlund H, et al.. Combining risk factors and demographic surveillance: potentials of WHO STEPS and INDEPTH methodologies for assessing epidemiological transition. Scand J Public Health. 2006; 34: 199–208.
- Ministry of Public Health of Thailand. The report of Thailand Population Health Examination Survey III, 2003–2004. Bangkok: Ministry of Public Health. 2006.
- Bharucha NE, Kuruvilla T. Hypertension in the Parsi community of Bombay: a study on prevalence, awareness and compliance to treatment. BMC Public Health. 2003; 3: 1.
- Sayeed MA, Mahtab H, Khanam PA, Begum R, Banu A, Azad Khan AK. Diabetes and hypertension in pregnancy in a rural community of Bangladesh: a population-based study. Diabet Med. 2005; 22: 1267–71.
- Padwal R, Straus SE, McAlister FA. Evidence based management of hypertension. Cardiovascular risk factors and their effects on the decision to treat hypertension: evidence based review. BMJ. 2001; 322: 977–80.
- Ahmed SM , Hadi A , Razzaque A , Ashraf A , Juvekar S , Ng N , et al. Clustering of chronic non-communicable disease risk factors among selected Asian populations: levels and determinants. Global Helath Action Supplement 1, 2009. DOI: 10.3402/gha.v2i0.1986.
- Lim SS, Gaziano TA, Gakidou E, Reddy KS, Farzadfar F, Lozano R, et al.. Prevention of cardiovascular disease in high-risk individuals in low-income and middle-income countries: health effects and costs. Lancet. 2007; 370: 2054–62.
- Magnus P, Beaglehole R. The real contribution of the major risk factors to the coronary epidemics: time to end the “only-50%” myth. Arch Intern Med. 2001; 161: 2657–60.
- Mendis S, Abegunde D, Oladapo O, Celletti F, Nordet P. Barriers to management of cardiovascular risk in a low-resource setting using hypertension as an entry point. J Hypertens. 2004; 22: 59–64.
- INCLEN Multicenter Collaborative Group. Body mass index and cardiovascular disease risk factors in seven Asian and five Latin American centers: data from the International Clinical Epidemiology Network (INCLEN). Obese Res. 1996; 4: 221–228.
- Tesfaye F, Ng N, Minh HV, Byass P, Berhane Y, Bonita R, Wall S. Association between body mass index and blood pressure across three populations in Africa and Asia. Journal of human hypertension. 2007; 21(1):28–37.