Health impacts of climate change and the need to prevent them should be at centre stage of the ongoing debate on climate policies Citation1. We have specifically prepared this series of papers to be available for the COP15Footnote1 conference in Copenhagen, to which the world looks to agree on targets and procedures to reduce greenhouse gas (GHG) emissions on the basis of fair burden-sharing between high and low-income countries.
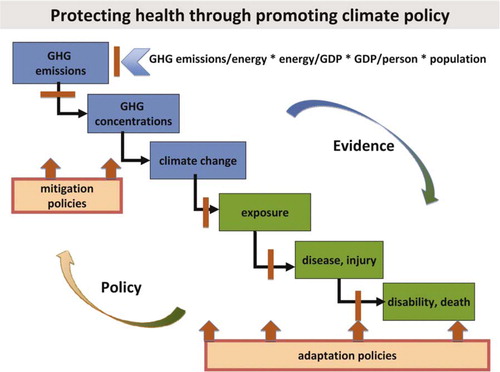
illustrates how GHG emissions, health impacts and climate policies are linked through a cascade of causes and effects. It highlights, how evidence of health impacts (top right arrow) can and should influence the debate on mitigation and adaptation (bottom left arrow).
Figure 1. Relationships between climate policy and health.
The factors in the upper part of the graph leading to GHG emissions are known as the ‘Kaya identity’, although the formula by Kaya and Yakobori Citation2 captures only energy-related emissions and was originally developed for CO2 emissions. Put in words: How can we decarbonise energy production and increase energy efficiency while protecting economic growth particularly in low and middle-income countries for a growing population?
There are three strong reasons for the climate policy community to consider health impacts:
the impacts are large, increasing and inequitably distributed;
the majority of people everywhere are concerned about the protection of their own and their children's health and are hence prepared to support mitigation policies; and
certain mitigation policies have significant positive health ‘co-benefits’, and these should be quantified and promoted to support mitigation arguments.
Health impacts are large, increasing and inequitably distributed
There are a large number of documented and imputed effects of climate change on health, operating through an even larger set of direct and indirect processes. We refer the reader to a recent review Citation8. An assessment by WHO in 2004 concluded that approximately 166,000 deaths occurred in the year 2000 due to climate changes that had occurred between 1990 and 2000 Citation3. An increase over time is very likely. Updated calculations of the global burden of disease are in progress and the Centre for Global Health Research at Umeå University will contribute to that work, which is intended to estimate current health impacts and forecast future health impacts of climate change up to 2030.
Furthermore, populations in low-income countries are the most vulnerable to adverse health effects of climate change. This raises major ethical and political concerns Citation4Citation5Citation6Citation7. There are a large number of documented and imputed effects of climate change on health, operating through an even larger set of direct and indirect processes. We refer the reader to a recent review Citation8. Here we focus on two large groups of climate-exacerbated adverse health effects: the first is a direct effect, the second largely indirect.
Important in the mitigation debate, but discussed very little, is the major contribution due to health damage to estimates of the full economic costs of climate change on human welfare under any climate scenario. Stern Citation32 included health as one of the non-market climate impacts in one of his models. When those were added to his economic model of climate change impacts, the long-term economic impact up to the year 2200 increased from 7.3 to 13.8% of GDP per capita.
Health is a potentially excellent motivator for change behaviour and policies
The concern of citizens about their own and their children's health is arguably the most powerful motivator to accept changes in lifestyle or to accept the inconvenience and costs involved with climate policies. As Jay and Marmot Citation33 recently put it: ‘Crucially for winning hearts and minds in richer countries, what is good for the climate is good for health’. Surprisingly, apart from some studies (from the high-income countries) on the individual or public willingness-to-pay (WTP) for climate policies, which reported a 50% increase in individual WTP for improved climate protection between 2003 and 2006 Citation34, we could not identify any significant literature on this issue. On the other hand, studies on the perception of climate change and individual behaviour change do exist, albeit mainly from the high-income countries Citation35.
Careful and science-based communication of the health risks of climate change and the co-benefits of climate policies may therefore be an important approach for convincing both lawmakers and the general public of the urgency of climate policy. Studies on which channels and messages might be most effective in doing so would be welcome.
Mitigation policies will generate health ‘co-benefits’
There are potentially large health co-benefits of mitigation policies, which should be entered into the economic calculations of the costs of mitigation. While such co-benefits have been amply documented to accrue in other sectors, such as agriculture, technology and forestry, the quantification of health co-benefits is at a particularly early stage and requires strong research effort and methodological development, such as proposed by Smith and Haigler Citation36. An innovative angle put forward by Yamamoto et al. Citation29 is to view policies for reducing biomass-burning for cooking as climate policies, which huge health co-benefits. It is not widely known that indoor air pollution arising from cooking currently kills far more people than the consequences of outdoor air pollution.
The way forward
Fill the research gaps
Many knowledge gaps have been identified, for example, in the IPCC assessment report Citation37 as well as in other reviews Citation38Citation39. The most recent international attempt to identify gaps and recommend future research was a meeting in Madrid in October 2008 organised by WHO, the United Nations Foundation, the US National Institute of Environmental Health Sciences and the Ministry of Health of Spain Citation40.
An example of an important gap is the lack of research on the impact of climate change-related increases in heat exposure on working people Citation14. Such impacts can be expected to have direct consequences for local economic development potential in exposed populations Citation9.
Although still small compared to other climate-relevant sectors, research on the climate–health nexus is rapidly evolving. Universities are beginning to move such research up their priority list and courses, both introductory and research oriented, are offered both in the high-income countries (for example at Umeå University, University of Heidelberg and Australian National University) and soon in the low and middle-income countries (for example, at BRAC University in Bangladesh). The involvement of researchers from low-income countries is still low Citation31, but growing, as reflected in this series of papers.
Develop and monitor adaptation strategies
Research evidence is still scant for answering some very policy-relevant questions, particularly in the context of developing countries: Which adaptation policies work best for which priority diseases and at what cost in a specific country context? How do we best set up early warning systems? How should we protect health infrastructures? Which drugs and vaccines need accelerated research and development? Which current health interventions need to be delivered with much more impetus in view of climate change? How can we focus health policies and interventions on the most vulnerable groups? And finally, most importantly, but very mundanely, how can we strengthen health systems in general to face yet another challenge to population health?
‘Use’ health as a driver for global climate policies
Nilsson et al. Citation41 compared the development of climate policy with that of tobacco control. The main difference between the two health threats lies in the fact that climate change has effects on the globe's entire population. Yet, victims and perpetrators of climate change suffer in very different degrees. The main lesson learnt from tobacco control for Copenhagen is: do not wait! More than 50 years elapsed between the scientific evidence that smoking has strong negative health effects and the signing of the Framework Convention for Tobacco Control. Delay to act is deadly, as each year smoking claims 5.4 million lives Citation41Citation42.
Our strong belief is that the world cannot afford to wait until all the evidence is in, as the smoking policy example has taught us. On the other hand, and opportunely for the COP15 conference, we hope to bring the argument of protecting health through mitigation closer to centre stage in the mitigation debate. The question is as simple as it is crucial:
Will the policy-makers gathering in Copenhagen later this year live up to the challenge and agree on measures to effectively and fairly reduce GHG emissions, in order to protect our our children's health?
Overview of this special volume
The 23 articles in this special volume focus on two large groups of climate-exacerbated adverse health effects: the first is a direct effect, the second largely indirect.
The effects of heat on human health. These direct effects are potentially magnified by climate change. A particular perspective is that heat and humidity do not only act on human physiology, but also reduce work productivity, particularly in developing countries Citation9. The collection of articles on ‘Heat and Health’ focuses on direct human exposures to extreme heat, which will be an increasing condition in most of the world with climate change. Excessive heat exposure is a health risk for all age groups and the paper by Jendritzky and Tinz Citation10 shows with innovative maps the extent to which different parts of the world are now at risk and will be at greater risk in 2050. Honda and Ono Citation11 have developed an improved method to quantify heat-related mortality risks, and Rocklöv and Forsberg Citation12 compare different methods for quantifying mortality impacts during heat waves. Parsons presents practical approaches for reducing health risks during heat waves Citation13. The main focus in the other articles is on the vulnerable group of adults carrying out heavy labour in hot working environments: outdoors or indoors. Kjellstrom, Holmer and Lemke Citation14 describe the physiological mechanisms behind the health and productivity effects. Examples of these types of occupational health concerns are given by Lin and Chan (Taiwan) Citation15, Ayyappan, Sankar, Rajkumar and Balakrishnan (India) Citation16 and Delgado (Nicaragua) Citation17. Crowe, van Wendel de Joode and Wesseling Citation18 discuss in detail the possibilities of investigating such concerns in Costa Rica, and Kjellstrom, Gabrysch, Lemke and Dear Citation19 present the ‘High Occupational Temperature Health And Productivity Suppression’ (Hothaps) study programme, and invite interested scientists to participate. This programme will investigate global climate change impacts on heat and occupational health, a new concept publicised for the first time via this journal.
The effects on infectious diseases. These are indirect effects of climate change. Using a decidedly global lens, we report on increases in various infectious diseases both in the Arctic (Evengård and Parkinson Citation20, Rydén et al. Citation21 and Evander and Ahlm Citation22) and in tropical countries (Yé et al. Citation23, Palmgren Citation24, Ling et al. Citation25, Tourre et al. Citation26, Emmelin et al. Citation27 and Dambach et al. Citation28). The authors examine a wide range of diseases of parasitic, bacterial and viral origin. The focus, however, is on action for health systems: (i) assessing the dynamic, magnitude and nature of health impacts Citation22Citation23; (ii) identifying most vulnerable populations Citation20Citation26Citation27; and (iii) contributing to the development of new tools for health systems for surveillance and early warning Citation21Citation23Citation25Citation26Citation28 The paper by Yamamoto et al. Citation29 examines the link between climate change and indoor air pollution, two seemingly unrelated public health threats. Evengård and Sauerborn Citation30 ‘connect the dots’ by pointing to a set of six common scientific and policy challenges in the Arctic and the tropics with regard to climate-sensitive infectious diseases. These papers thus stress common ground in research and policy challenges in what otherwise are extremely different settings: the cold high-income countries and the warm low and middle-income countries. Byass Citation31 finally reviews and portrays the dearth of research on climate change and health in Africa and looks at ways of stimulating more work in this field, particularly by African scientists.
Notes
1. COP means ‘Conference of the Parties’ and was created by Article 7 of the United Nations Framework Convention on Climate Change (UNFCCC), signed in Rio de Janeiro in 1992 and ratified by 193 countries. The COP is the ‘supreme body of this convention’ and mandated ‘to review the implementation of the Convention and any legal instrument…and shall make…the decisions necessary to promote the effective implementation of the Convention’. The conference convened in Copenhagen between December 8th and 19th 2009 will be the 15th such conference, hence COP15.
References
- Lim V, Stubbs JW, Nahar N, et al.. Politicians must heed health effects of climate change (Letter). BMJ. 2009; 339: b3672.
- Kaya Y, Yokobori K. Environment, energy, and economy: strategies for sustainability. United Nations University Press. TokyoJapan, 1998
- McMichael AJ, Campbell-Lendrum DH, Corvalan CF, Ebi KL, Githeko A, Scheraga JD, et al. Climate change and human health – risks and responses. Geneva: WHO. 2003.
- McMichael AJ, Campbell-Lendrum D, Kovats A, Edwards S, Wilkinson P, Wilson T, et al.Global climate change. Comparative quantification of health risks. Global burden of diseases attributable to selected major risk factors. Ezzati M, Lopez AD, Rodgers A, Murray CJLWorld Health Organization. Geneva, 2004
- Friel S, Marmot M, McMichael AJ, Kjellstrom T, Vågerö D. Global health equity and climate stabilization: a common agenda. Lancet. 2008; 373: 1677–82.
- Patz J, Campbell-Lendrum D, Gibbs H, Woodruff R. Health impact assessment of global climate change: expanding on comparative risk assessment approaches for policy making. Annu Rev Public Health. 2008; 29: 27–39.
- Campbell-Lendrum D, Corvalán C, Neira M. Global climate change: implications for public health policy. Bull World Health Organ. 2007; 85: 161–244.
- Costello A, Abbas M, Allen A, Ball S, Bell S, Bellamy R, et al.. Managing the health effects of climate change: Lancet and University College London Institute for Global Health Commission. Lancet. 2009; 373: 1693–733.
- Kjellstrom T. Climate change, direct heat exposure, health and well-being in low and middle-income countries. Global Health Action. 2009. DOI: 10.3402/gha.v2i0.1958.
- Jendritsky G, Tinz B. The thermal environment of the human being on the global scale. Global Health Action. 2009. DOI: 10.3402/gha.v2i0.2005.
- Honda Y, Ono M. Issues in health risk assessment for current and future heat extremes. Global Health Action. 2009. DOI: 10.3402/gha.v2i0.2043.
- Rocklöv J, Forsberg B. Comparing approaches for studying the effects of climate extremes – a case study of hospital admissions in Sweden during an extremely warm summer. Global Health Action. 2009. DOI: 10.3402/gha.v2i0.2034.
- Parsons K. Maintaining health, comfort and productivity in heat waves. Global Health Action. 2009. DOI: 10.3402/gha.v2i0.2057.
- Kjellstrom T, Holmer I, Lemke B. Workplace heat stress, health and productivity – an increasing challenge for low and middle-income countries during climate change. Global Health Action. 2009. DOI: 10.3402/gha.v2i0.2047.
- Lin R-T, Chan C-C. Effects of heat on workers’ health and productivity in Taiwan. Global Health Action. 2009. DOI: 10.3402/gha.v2i0.2024.
- Ayyappan R, Sankar S, Rajkumar P, Balakrishnan K. Work-related heat stress concerns in automotive industries: a case study from Chennai. , India. Global Health Action. 2009. DOI: 10.3402/gha.v2i0.2060.
- Delgado CO Heat stress assessment among workers in a Nicaraguan sugarcane farm. Global Health Action. 2009. DOI: 10.3402/gha.v2i0.2069.
- Crowe J, van Wendel de Joode B, Wesseling C. A pilot field evaluation on heat stress in sugarcane workers in Costa Rica: what to do next?. Global Health Action. 2009. DOI: 10.3402/gha.v2i0.2062.
- Kjellstrom T, Gabrysch S, Lemke B, Dear K. The ‘Hothaps’ programme for assessing the impacts of climate change on occupational health: an invitation to carry out field studies. Global Health Action. 2009. DOI: 10.3402/gha.v2i0.2082.
- Parkinson AJ, Evengård B. Climate change, its impact on human health in the Arctic and the public health response to threats of emerging infectious diseases. Global Health Action. 2009. DOI: 10.3402/gha.v2i0.2075.
- Rydén P, Sjöstedt A, Johansson A. Effects of climate change on tularaemia disease activity in Sweden. Global Health Action. 2009. DOI: 10.3402/gha.v2i0.2063.
- Evander M, Ahlm C. Milder winters in northern Scandinavia may contribute to larger outbreaks of hemorrhagic fever virus. Global Health Action. 2009. DOI: 10.3402/gha.v2i0.2020.
- Ye Y, Hoshen M, Kyobutungi C, Louis VR, Sauerborn R. Local scale prediction of Plasmodium falciparum malaria transmission in an endemic region using temperature and rainfall. Global Health Action. 2009. DOI: 10.3402/gha.v2i0.1923.
- Palmgren H . Meningococcal disease and climate. Global Health Action. 2009. DOI: 10.3402/gha.v2i0.2061.
- Ling HY , Rocklöv J , Ng N , Sauerborn R , Siang TC , Yin PF . Climate variability and increase in intensity and magnitude of dengue incidence in Singapore. Global Health Action. 2009. DOI: 10.3402/gha.v2i0.2036.
- Tourre YM , Lacaux J-P , Vignolles C , Lafaye M . Climate impacts on environmental risks evaluated from space: a conceptual approach to the case of Rift Valley Fever in Senegal. Global Health Action. 2009. DOI: 10.3402/gha.v2i0.2053.
- Emmelin A , Fantahun M , Berhane Y , Wall S , Byass P . Vulnerability to episodes of extreme weather: Butajira, Ethiopia, 1998–1999. Global Health Action. 2008. DOI: 10.3402/gha.v1i0.1829.
- Dambach P , Sié AN , Lacaux JP , Vignolles C , Machault V , Sauerborn R . Using high-spatial resolution remote sensing for risk mapping of malaria occurrence in the Nouna district, Burkina Faso. Global Health Action. 2009. DOI: 10.3402/gha.v2i0.2094.
- Yamamoto S , Sié A , Sauerborn R . Cooking fuels and the push for cleaner alternatives: a case study from Burkina Faso. Global Health Action. 2009. DOI: 10.3402/gha.v2i0.2088.
- Evengård B, Sauerborn R. Climate change influences infectious diseases both in the Arctic and in the tropics: connecting the dots. Global Health Action. 2009. DOI: 10.3402/gha.v2i0.XXXX.
- Byass P . Climate change and population health in Africa: where are the scientists?. Global Health Action. 2009. DOI: 10.3402/gha.v2i0.2065.
- Stern N. The economics of climate change. Cambridge University Press. Cambridge, 2007
- Jay M, Marmot MG. Health and climate change (editorial). BMJ. 2009; 339: b3669.
- Curry TE . A survey of public attitudes towards climate change and climate change mitigation technologies in the United States: analysis of 2006 results. CambridgeMA: MIT., Laboratory for Energy and the Environment, Publication No LFEE 2007-01-WP; 2007.
- Semenza JC, Hall DE, Wilson DJ, Bontempo BD, Sailor DJ, George LA. Public perception of climate change voluntary mitigation and barriers to behavior change. Am J Prev Med. 2008; 35: 479–87.
- Smith KR, Haigler E. Co-benefits of climate mitigation and health protection in energy systems: scoping methods. Ann Rev Pub Health. 2008; 29: 11–25.
- Inter-Governmental Panel on Climate change. Fourth Assessment Report IPCC, Volume 2: Impacts, Adaptation and Vulnerability. GenevaCambridge: Cambridge University Press. 2007. Available from: www.ipcc.ch.
- McMichael T. Environmental change, climate and population health: a challenge for inter-disciplinary research. Environ Health Prev Med. 2008; 13: 183–6.
- Sauerborn R. Global environmental change-an agenda for research and teaching in public health – invited editorial. Scand J Public Health. 2007; 35: 561–3.
- Neira M Foreword. Global Health Action. 2009. DOI: 10.3402/gha.v2i0.2109.
- Nilsson M, Beaglehole R, Sauerborn R. Climate policy: lessons from tobacco control. Lancet. 2009; submitted.
- WHO report on the global tobacco epidemic, The MPOWER package. Geneva: World Health Organization. 2008.