Background
Natural disasters result in significant numbers of disabling impairments. Paradoxically, however, the traditional health system response to natural disasters largely neglects health-related rehabilitation as a strategic intervention.
Objectives
To examine the role of health-related rehabilitation in natural disaster relief along three lines of inquiry: (1) epidemiology of injury and disability, (2) impact on health and rehabilitation systems, and (3) the assessment and measurement of disability.
Design
Qualitative literature review and secondary data analysis.
Results
Absolute numbers of injuries as well as injury to death ratios in natural disasters have increased significantly over the last 40 years. Major impairments requiring health-related rehabilitation include amputations, traumatic brain injuries, spinal cord injuries (SCI), and long bone fractures. Studies show that persons with pre-existing disabilities are more likely to die in a natural disaster. Lack of health-related rehabilitation in natural disaster relief may result in additional burdening of the health system capacity, exacerbating baseline weak rehabilitation and health system infrastructure. Little scientific evidence on the effectiveness of health-related rehabilitation interventions following natural disaster exists, however. Although systematic assessment and measurement of disability after a natural disaster is currently lacking, new approaches have been suggested.
Conclusion
Health-related rehabilitation potentially results in decreased morbidity due to disabling injuries sustained during a natural disaster and is, therefore, an essential component of the medical response by the host and international communities. Significant systematic challenges to effective delivery of rehabilitation interventions during disaster include a lack of trained responders as well as a lack of medical recordkeeping, data collection, and established outcome measures. Additional development of health-related rehabilitation following natural disaster is urgently required.
Introduction
Natural disasters result in significant mortality, morbidity, and disability due to high numbers of traumatic injuries that severely impact the health of the injured population and the overall health system of the affected country. Emergency response and recovery efforts to mitigate disaster-related disability by both host national and international responders are significantly challenged by the relative absence of health-related rehabilitation perspective. The primary objective of this paper is to examine the role of health-related rehabilitation in natural disaster relief in terms of three lines of inquiry: first, the epidemiology of injury and disability in natural disasters; second, the impact of natural disasters on health and rehabilitation systems; and lastly, the assessment and measurement of disability due to natural disasters. Selected challenges to and strategies for providing effective health-related rehabilitation following a natural disaster are also addressed.
Background: disaster, disability, and health-related rehabilitation
A natural disaster may be defined as ‘sudden ecological disruption or threat that exceeds the adjustment capacity of the affected community and requires external assistance’ Citation1 Citation2. Natural disasters include earthquakes, floods, tidal waves (tsunamis), landslides, hurricanes, volcanic eruptions, as well as droughts Citation2.
Natural disasters result in immediate, significant loss of life and long-term physical impairments such as spinal cord injuries (SCI), traumatic brain injuries (TBI), amputations, fractures, and peripheral nerve injuries Citation3; related mental health conditions including situational anxiety and post-traumatic stress disorder occur concomitantly Citation4–Citation7. In addition to acute injuries, persons also suffer exacerbations of pre-existing chronic health problems and disabilities Citation8–Citation11.
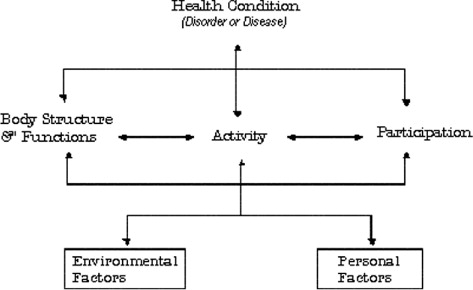
Though saving lives immediately after a natural disaster is the highest initial priority, the focus of the local and international medical response effort quickly shifts to the treatment of severe, traumatic injuries and related health problems Citation12. From the perspective of health-related rehabilitation, the primary focus is the ‘functioning’ of the surviving population. As defined by the World Health Organization's (WHO) International Classification of Functioning, Disability, and Health (ICF), ‘functioning’ is a dynamic interaction of the health and health-related domains of ‘body functions and structures’ as well as ‘activity and participation.’ ‘Disability’ is an umbrella term for impairment in body functions or structures and limitation in activity and/or restriction in participation. Since an individual's functioning and disability occurs within a larger social and individual context, the ICF also includes environmental and personal factors Citation13 (see ). Accordingly, health-related rehabilitation is a major health strategy that focuses on the functioning (i.e. functional status) of persons with physical or mental disability and considers their resources and environment Citation14 Citation15.
Fig. 1. The WHO model of the International Classification of Functioning, Disability, and Health (ICF). Source: WHO, 2001.
Health-related rehabilitation begins with the onset of injury or disease and can extend over a lifetime, often involving treatment in the hospital, community, and home settings. Since a person's functional needs require attention in the immediate living environment as well as in the greater community Citation15, a range of activities including provision of accessible and appropriate home care; housing; transportation; and educational, vocational, and social opportunities is necessary. Based on the person's unique medical needs, health-related rehabilitation is best delivered by a multi-disciplinary team including, at a minimum, a specialist in Physical and Rehabilitation Medicine (PRM), a physical therapist, an occupational therapist, and a rehabilitation nurse Citation16.
As an expert in disability and functioning who is also trained in the diagnosis and treatment of general health problems, the PRM physician performs a critical role in integrating rehabilitation efforts with other health strategies and providers. Physical and occupational therapists trained in neurological and orthopedic rehabilitation perform indicated interventions; a rehabilitation nurse provides overall medical case management; the rehabilitation psychologist provides impairment and bereavement counseling and also connects the patient to psychosocial supports in the community – especially critical when family members, relatives, and homes are lost Citation17. Non-medical caregivers ideally become increasingly involved in the rehabilitation process as the person's medical status and needs change. Their committed participation is essential for optimal outcomes and even survival, especially for the low functioning, highly dependent patient in the home setting.
Methods
This paper is based on a scientific literature review supplemented by secondary analysis of injury data as well as reports from the gray literature.
Literature review
A qualitative literature review was conducted including searches of the internet-based, open access databases PubMed and Google Scholar. Due to high relevance to the role of health-related rehabilitation in disaster relief, searches were performed on the epidemiology of injury and disability in natural disaster, the impact of natural disasters on health and rehabilitation systems, and the assessment and measurement of disability due to natural disasters. These lines of inquiry were chosen according to the key aspects of the MICRODIS research program on health impacts of natural disaster Citation18.
Secondary analysis of EM-DAT injury data
The WHO-sponsored Emergency Events Database EM-DAT ( www.emdat.be) served as the data source for numbers of injuries and deaths in natural disasters by year of event (1970–2010), region, and country. Absolute numbers of injuries and deaths due to natural disasters of all kinds were extracted by year and region (N=246). As regards earthquakes, we also calculated ratios of injuries to deaths for each year and country (N=568); cases in which no deaths were reported were excluded. We compared these data along 10-year periods by analyses of variance. To test for statistical significance of differences in numbers of injuries, numbers of deaths, and injuries to death ratios between time periods, we performed post hoc tests with Dunnett's T3 correction for multiple testing in the case of inhomogeneous variances between groups Citation19. Level of significance was alpha error probability (p)=.05. The Dunnett T3 correction is conservative in that the family wise error rate (i.e. the error rate for the whole set of comparisons between groups) will never exceed alpha. In the case of injuries and deaths due to all natural disasters, we performed a separate analysis for the Asian region (N=41). We supplemented the post hoc comparison of time periods with two negative binomial regressions of the number of injuries and deaths, respectively, on the year of the event. In the case of injuries to deaths ratios in earthquakes, we calculated a Generalized Estimated Equation (GEE) model, fitted to a negative binomial distribution, and using country as panel and year as time variable. All calculations were made either with Stata 11 or with SPSS 14.
Epidemiology of injury and disability following natural disasters
Incidence of injuries
The incidence of morbidity and mortality caused by natural disasters is highly variable and depends upon many environmental and human factors Citation20–Citation22. Earthquakes in the People's Republic of China from 2000 to 2009, for instance, injured 387,829 persons (0.7% of all affected persons) and killed 87,947 people (0.17%) Citation22. A higher percentage of the affected population was injured (4.4%) or killed (2.5%) in the Armenian earthquake of 1988. Adolescents and persons aged 40 and older were disproportionately injured; also, persons residing in taller buildings and higher within the buildings suffered higher incidences of injury Citation20. The 2010 earthquake in Haiti injured about 300,000 (8.8%) and killed 222,570 people (6.5%) with 3,400,000 being affected Citation22. Significant causes of this devastating effect include the proximity of the epicenter to the densely populated center of Port-au-Prince on a busy weekday afternoon and the low-quality concrete building construction. Conversely, in the United States earthquakes affected 30,619 persons from 2000 to 2009; 523 injuries (1.7%) and only 3 deaths are reported Citation22. Floods, by comparison, cause fewer injuries than earthquakes; the recent flood in Pakistan, for example, resulted in 2,327 injuries (0.00011%) and 2,021 deaths (0.00010%) reported Citation22.
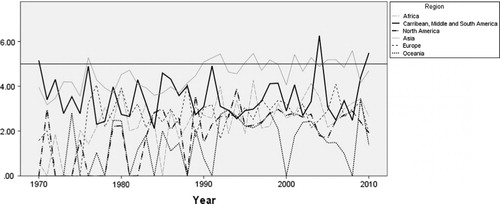
shows the absolute number of primary injuries reported globally across all natural disasters from 1970 to 2010. The Asian continent is significant for an increase in the absolute number of reported injuries despite the fact that the population of the Asia-Pacific region has been growing more slowly than that of the rest of the world since 1990, dropping from 1.5% in the early 1990s to 1.0% in 2008 Citation23.
Fig. 2. Development of the absolute number of reported injuries (logarithm to base 10) by year and world region from 1970 to 2010 over all types of natural disaster; the solid line parallel to the abscissa means 100,000 injuries (lg (100,000) = 5). Source: Own calculation based on data from www.emdat.be; numbers of injuries were extracted by year and region.
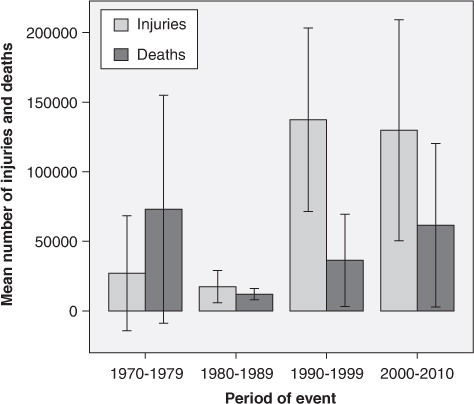
displays mean numbers of reported injuries and deaths due to all natural disasters in Asia in 10-year periods since 1970; injuries are more prominent than deaths dating from 1980 to 1989. The following differences in mean numbers of injuries were statistically significant according to Dunnett T3 post hoc tests: 1970–1979 versus 1990–1999 and 1980–1989 versus 1990–1999. The difference of the periods 1980–1989 and 2000–2010 was almost significant (p=.054). No differences in mean numbers of death reached the level of significance (see and ). This result was confirmed by the two negative binomial regressions of the numbers of injuries and deaths, respectively, on year of event (injuries: b Year = 0.064; p<0.001; deaths: b Year = 0–.003; not significant).
Fig. 3. Development of mean numbers of injuries and deaths due to all types of natural disaster from 1970 to 2010 in the Asian continent; error bars indicate 95% confidence intervals (for mathematical reasons, confidence intervals for the period 1970 to 1979 reach below zero). Source: Own calculation on the basis of data from www.emdat.be.
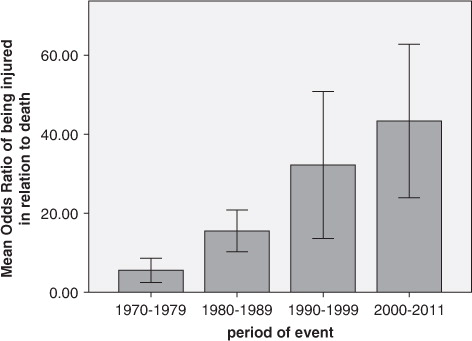
indicates the odds ratio of sustaining injury compared to death in earthquakes globally since 1970; the increasing odds of injury over time may be due to both, advances in natural disaster response and changes in definitions of injury, measurement, or reporting of data. The following differences were statistically significant according to Dunnett T3 post hoc tests: 1970–1979 versus all other periods; 1980–1989 versus 2000–2011. It is important to note that results may be different if other time periods were chosen. However, a significant trend regarding an increase in the (odds) ratio of injuries to deaths over time was also confirmed by the GEE model (b Year = 0.049, p<0.001) (see ).
Types of injuries and disabilities
Data on types of disaster-induced injury and potentially disabling conditions are less available and mostly derived from chart reviews of individual hospitals as opposed to multi-center or population-based studies Citation24. Consequently, disability in the community in developing regions is relatively unstudied. Major and potentially disabling injuries after natural disasters that have been documented include SCI, TBI, limb amputation, long bone fractures, crush injuries, and peripheral nerve injuries Citation25–Citation30. Minor injuries include conditions such as swollen feet and legs, leg pain and cramps, tendonitis/fasciitis, wound infections, and musculoskeletal strain and pain Citation31–Citation34.
Reliable data on the distribution of these injury types in disaster-affected populations are widely unavailable.
Key concepts such as definitions, even conventional, that describe the population exposed to death and injury from earthquakes have yet to be established. As a result, not only are results from different studies not comparable, denominators are inadequate even within a study, making rates and ratios suspect. Citation35
Various sources of bias in recording of injury data exist as well. Studies reflect findings in individuals who present for care at medical facilities, largely excluding those who do not, for example; even more significantly, functional health outcomes and long-term disability measures are seldom collated for analysis even if performed. Finally, aggregate population injury is rarely systematically assessed at the time of disaster when its knowledge could potentially have the most impact.
Persons with pre-existing health conditions
Persons with pre-existing physical disabilities and those with chronic physical and mental health conditions as well as very young and old people are at increased risk for suffering additional co-morbidities as a result of a natural disaster. Even when evacuated safely, the loss of medications, assistive devices, and support personnel can worsen the condition of these vulnerable persons and further impair their overall functioning and quality of life Citation10 Citation36 Citation37. Moreover, these persons often have greater difficulty meeting basic needs following a natural disaster since adequate transportation and sheltering are often not included in local disaster response plans Citation9 Citation11. Compromised basic and specialty medical care following a natural disaster also increases risk of medical complications including infection, organ failure, and even death Citation38–Citation40. According to a study after the great Hanshin-Awaji earthquake in 1995, it was found that the odds ratio (OR) of death for persons with pre-existing physical disabilities nearly doubled Citation41; a similar study after the Taiwanese earthquake in 1999 Citation40 found that the OR was 1.7 for deaths of persons with pre-existing moderate physical disability and doubled for persons with pre-existing mental conditions.
Effectiveness of health-related rehabilitation interventions
There are few studies that evaluate the effectiveness of rehabilitation interventions following a natural disaster. Since prospective, randomized controlled trials of specific interventions following disaster are not feasible, retrospective analyses of hospital cohorts, observational studies, and surveys are performed to measure the clinical impact of physical rehabilitation on disaster-induced disability. For example, it was demonstrated following the 2005 earthquake in Pakistan that patients under the care of PRM physicians had reduced lengths of hospital stay, fewer complications, and better clinical outcomes than patients in centers with no physiatrist supervision Citation42 Citation43. Conversely, it was noted that although early rehabilitation of SCI survivors in major provincial hospitals following the 2008 Sichuan Earthquake showed generally positive results, post-discharge follow-up resulted in a reverse of functional gains as well as secondary complications in some patients due primarily to insufficient long-term, community-based rehabilitation (CBR) resources Citation44.
Impact of natural disasters on health and rehabilitation systems
The significant negative health consequences of natural disasters usually overwhelm the affected society including the health system Citation45, especially in low-resourced regions of the world where most natural disasters occur Citation46. Moreover, health professionals and their families may be affected themselves, thereby limiting medical facility and professional organization response as well as disrupting overall societal function Citation47. Destruction or weakening of pre-existing rehabilitation services translates into minimal rehabilitative strategy being practiced during the immediate emergency response, further burdening an already challenged post-disaster health system. Poor functional outcomes and long-term negative consequences for the individual, community, and society result. The unexpected death or disability of an earning family member, for instance, can impoverish the family Citation36. Efficient use of rehabilitative strategies will not only help unburden the challenged health system by mobilizing patients, but will also facilitate recovery of the post-disaster society by facilitating victims’ access to education and employment opportunities.
Challenges to providing post-disaster rehabilitation
Regrettably, the provision of rehabilitative services is extremely limited during the immediate emergency response due to surgical bias of responding teams and the general lack of rehabilitation knowledge of team members. The lack of host rehabilitation and health services infrastructure compounds the lack of rehabilitation perspective; often few or no rehabilitation services or professional providers, especially PRM physicians, exist in areas affected by natural disasters Citation10 Citation48–Citation50. To compensate for this lack of expertise, rehabilitation training strategies are required Citation50 Citation51. Foreign rehabilitation responders can provide focused training to fellow team members as well as to local rehabilitation and non-rehabilitation providers in the field, hospital, and community settings throughout the disaster response. This expertise results in improved patient outcomes and also builds local rehabilitation infrastructure capacity.
Ideally, rehabilitation providers participate in victim triage, consult peri-operatively, and assist with post-operative care. Lack of rehabilitation expertise post-operatively, for example, can result in pressure sores and wound infections in mobility-limited persons Citation10. In an extreme case, SCI patients were found to be waiting for a cure and had not begun rehabilitative measures 8 months after the 2003 earthquake in Bam, Iran Citation52. Missed critical, injury-specific therapeutic windows result in longer hospital lengths of stay and translate to suboptimal functional outcomes with long-term negative consequences for the individual and the society Citation36. Besides making critically needed hospital beds available, effective rehabilitative strategies also help return family members to work producing income to sustain the family and reconstruct the post-disaster society.
Foreign responding organizations with rehabilitation personnel face significant challenges to effective deployment within the disaster zone. Individual rehabilitation providers must be properly qualified, the team deployment-ready, travel arranged, and on-scene assignment confirmed with the host country responsible organization(s). On arrival in the host country, travel to the deployment areas can be complicated by vehicle terrain and uncertainty.
Even if effectively deployed, however, international service providers must be aware that rehabilitation service coordination between the host organization, local Disabled persons organizations (DPOs), the central disaster rehabilitation response authority, and collaborating rehabilitation non-governmental organizations (NGOs) may be limited Citation3 Citation48 Citation53. Unfortunately, since ‘disability’ is considered a ‘cross-cutting issue’ Citation54 within the humanitarian response framework (i.e. as opposed to specifically identified areas of coordination including ‘food,’ ‘education,’ and ‘health’), disability issues appear at risk for more inefficient communication, coordination, and resource allocation Citation55. Consequently, responding foreign teams must assume responsibility for coordinating directly with other rehabilitation providers to ensure that appropriate interventions are performed in the acute care setting initially and subsequently in community follow-up.
Also, closely held cultural beliefs about health-related rehabilitation and disability Citation36 Citation52 sometimes limit the potential impact of rehabilitative services. Often, disability is viewed as a static rather than as a dynamic condition Citation56. For example, in many low-resourced countries it is believed that persons with permanent impairments such as SCI will depend on their families and be an object of charity their entire life. Disability is alsocommonly believed to be contagious and therefore to affect the entire family Citation54 Citation57.
Strategies for providing rehabilitation following natural disaster
Severe traumatic injuries sustained in a natural disaster require specialized management from the onset to reduce mortality and morbidity and to optimize individual functioning including social participation. Delay in treatment reduces effectiveness of rehabilitative therapies, resulting in poorer outcomes. Both TBI and SCI victims require immediate evacuation from the disaster zone to tertiary care facilities as opposed to nearby temporary shelters, field hospitals, or community hospitals. Spinal cord patients require specialized transport/transfer protocols and expert consultation for decision-making on definitive management (conservative vs. surgical) Citation48 Citation49.
Once stabilized and managed in the appropriate inpatient setting, these patients can be transferred to either a less acute care setting or to their home where they will benefit from treatment provided by their caregiver, a community-based facility, or a mobile rehabilitation service depending on specific needs. These services would also identify and treat disaster victims who may not have received care as well as those with pre-existing disability who could benefit from rehabilitative therapies. Optimal rehabilitative and medical care initiated following a natural disaster, however, results in a higher incidence of survivors with a significant physical disability (i.e. SCI) that can require significant long-term rehabilitative care. Lesser impaired individuals will also require necessary rehabilitation.
Patients can be trained in the use adaptive technologies, assistive devices, and mobility aids depending on their level of functional need. Medical equipment, however, must be compatible with the technological standards and physical environment of the affected community Citation58; powered wheelchairs are difficult to operate and maintain in developing countries, for example Citation59.
Assessment and measurement of disability in natural disasters
Significant injuries and associated surgical and rehabilitative care are often poorly documented during the immediate response to a natural disaster due to the emergent focus on saving and salvaging lives amidst chaotic, austere conditions. The loss of host facilities and personnel combined with the influx of international teams with varying recordkeeping practices can compromise recordkeeping further. Even well-established teams, however, may maintain substandard records and not provide them to receiving facilities on transfer or to patients upon discharge unless directly instructed by the host institution or government. Independently functioning international teams that do keep adequate records may not provide them to the national hosts on departure. This fragmentation and inconsistency of medical recordkeeping compromises surgical-rehabilitation continuity of care, especially as patients are transferred to the community, resulting in poorer patient outcomes.
Incomplete medical recordkeeping also limits further analysis since epidemiological data of post-disaster injury is usually extracted from individual hospital chart reviews and therefore may not accurately represent the affected population. (Also, facility records only reflect injured persons who present for care, as indicated earlier.) Consequently, comprehensive data following a natural disaster from which long-term delivery of rehabilitative services can be planned is not generally available.
Compounding incomplete disaster baseline and vital statistics, measurement of the impact of disaster-induced disability is further challenged by the lack of availability of appropriate standard indicators. The Disability Adjusted Life Year (DALY) is the main indicator of cost-effectiveness of risk control measures and widely used by WHO and the World Bank Citation60; however, its use is limited in national health services. The DALYs are based on an individual's underlying medical diagnosis and therefore they do not reflect the change in functional status or well-being due to rehabilitation services. Moreover, DALYs may be unreliable since they do not adjust for personal or environmental factors Citation61 Citation62. Other functional status measures Citation63 such as the Functional Independence Measure (FIM) Citation64 Citation65 are employed in research and clinical settings. Unfortunately, their use is generally restricted to the inpatient setting in developed countries and field use is impractical as these instruments require trained administration and are time-consuming to administer. Moreover, their inter-cultural validity as well as suitability for largely illiterate populations is questionable, indicating use of language independent assessment tools Citation66.
To answer the call for more effective assessment of the impact of rehabilitative interventions on the lives of persons with disabilities, several measures have been proposed based on the WHO's International Classification of Functioning, Disability, and Health (ICF). The WHO Disability Assessment Schedule (WHODAS 2.0) is an example of open resource instrument that can be used in population surveys Citation67. Regardless of what measure and indicators are developed, however, the humanitarian health community must readily adopt these evidence-based approaches in order to better measure the impact of its rehabilitation programming and to reduce the delayed health impact on the affected population Citation68.
System impacts of disability and rehabilitation after a natural disaster can foreseeably be modeled with cost-effectiveness analyses (CEA). These CEAs are economic evaluations widely used in developed countries to assess the relative value of one intervention over another for a given problem or condition. Their use in developing countries is relatively uncommon, although WHO has published standard guidelines for CEAs. One present rehabilitation-related use in the post-trauma setting is that of physiotherapy associated with evaluation of an orthopedic procedure Citation69. Rehabilitation procedures are more amenable to CEAs than therapeutic treatments. A wider use of existing measurement and assessment measures in addition to the development of new ones is required to more effectively measure the impact of physical rehabilitation strategies on disaster-induced disability in individuals and populations following a natural disaster.
Conclusion
This focused review has examined the role of health-related rehabilitation in disaster relief in terms of the epidemiology of injury and disability in natural disasters, the impact of natural disasters on health and rehabilitation systems, and the assessment of disability due to natural disasters. Selected challenges to and strategies for providing health-related rehabilitation following a natural disaster were addressed.
Although significant mortality, severe disabling injuries, and long-term disability have been demonstrated in natural disasters, health-related rehabilitation is only marginally employed as a disaster planning and response strategy. The necessity of more comprehensive baseline disaster disability statistics and more effective measurement of rehabilitation outcomes in disaster is emphasized. This focused review is intended to guide further inquiry into the role of health-related rehabilitation in disaster relief with the aim of strengthening the rehabilitation perspective in the response to natural disaster.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
Acknowledgements
We gratefully acknowledge the members of the Rehabilitation Disaster Relief Committee of the ISPRM and other members of the international rehabilitation community for their advocacy of the role of health-related rehabilitation in disaster relief.
References
- World Health Organization. Emergency care in natural disasters. Views of an international seminar. WHO Chron. 1980; 34: 96–100.
- Lechat MF. Disasters and public health. Bull World Health Organ. 1979; 57: 11–17.
- Eldar R. Preparedness for medical rehabilitation of casualties in disaster situations. Disabil Rehabil. 1997; 19: 547–51. 10.3402/gha.v4i0.7191.
- Fan F, Zhang Y, Yang Y, Mo L, Liu X. Symptoms of posttraumatic stress disorder, depression, and anxiety among adolescents following the 2008 Wenchuan earthquake in China. J Trauma Stress. 2011; 24(1): 44–53. [Epub ahead of print].10.3402/gha.v4i0.7191.
- Huang MJ, Guo LT, Li J, Sun XL, Zhang BZ, Yi QM, et al.. Epidemiological investigation on major depressive disorder in the most heavily damaged areas from Wenchuan earthquake in 2008 [in Chinese]. Zhonghua Liu Xing Bing Xue Za Zhi. 2010; 31: 167–70.
- Li S, Rao LL, Ren XP, Bai XW, Zheng R, Li JZ, et al.. Psychological typhoon eye in the 2008 Wenchuan earthquake. PLoS One. 2009; 4: e4964.10.3402/gha.v4i0.7191.
- Yun K, Lurie N, Hyde PS. Moving mental health into the disaster-preparedness spotlight. N Engl J Med. 2010; 363: 1193–5. 10.3402/gha.v4i0.7191.
- Chan EY, Griffiths S. Comparison of health needs of older people between affected rural and urban areas after the 2005 Kashmir, Pakistan earthquake. Prehosp Disaster Med. 2009; 24: 365–71.
- Mori K, Ugai K, Nonami Y, Kirimura T, Kondo C, Nakamura T, et al.. Health needs of patients with chronic diseases who lived through the great Hanshin earthquake. Disaster Manag Response. 2007; 5: 8–13. 10.3402/gha.v4i0.7191.
- WHO. Disasters, disability and rehabilitation. Geneva: Author. ; 2005. Available from: http://www.who.int/violence_injury_prevention/other_injury/disaster_disability2.pdf [cited 10 September 2010].
- Chan EY, Sondorp E. Medical interventions following natural disasters: missing out on chronic medical needs. Asia Pac J Public Health. 2007; 19: 45–51.
- Wisner B, Adams J, Environmental health in emergencies and disasters: a practical guide. Geneva: World Health Organization. ; 2003. Available from: http://www.who.int/water_sanitation_health/hygiene/emergencies/emergencies2002/en.
- WHO. International classification of functioning, disability and health. Geneva: Author; 2001.
- Stucki G, Melvin J. The international classification of functioning, disability and health: a unifying model for the conceptual description of physical and rehabilitation medicine. J Rehabil Med. 2007; 39: 286–92. 10.3402/gha.v4i0.7191.
- Stucki G, Cieza A, Melvin J. The international classification of functioning, disability and health (ICF): a unifying model for the conceptual description of the rehabilitation strategy. J Rehabil Med. 2007; 39: 279–85. 10.3402/gha.v4i0.7191.
- King JC, Nelson TR, Blankenship KJ, Turturro TC, Beck AJ. Chapter 46: rehabilitation team function and prescriptions, referrals, and order writing. In: DeLisa JA, Physical medicine and rehabilitation: principles and practice. PhiladelphiaPA: Lippincott Williams & Wilkins. 2005, pp. 1051–72.
- Armenian HK, Morikawa M, Melkonian AK, Hovanesian AP, Haroutunian N, Saigh PA, et al.. Loss as a determinant of PTSD in a cohort of adult survivors of the 1988 earthquake in Armenia: implications for policy. Acta Psychiatr Scand. 2000; 102: 58–64. 10.3402/gha.v4i0.7191.
- MICRODIS. 2007–2011. MICRODIS international symposium on health and health system impacts of natural disasters. Available from: http://www.microdis-eu.be/sites/default/files/UKL-HD%20Microdis%20symposium_Call%20for%20Papers.pdf [cited 1 April 2011].
- Dunnett CW. Pairwise multiple comparisons in the unequal variance case. J Am Stat Assoc. 1980; 75: 796–800. 10.3402/gha.v4i0.7191.
- Armenian HK, Melkonian A, Noji EK, Hovanesian AP. Deaths and injuries due to the earthquake in Armenia: a cohort approach. Int J Epidemiol. 1997; 26: 806–13. 10.3402/gha.v4i0.7191.
- Armenian HK, Melkonian AK, Hovanesian AP. Long term mortality and morbidity related to degree of damage following the 1998 earthquake in Armenia. Am J Epidemiol. 1998; 148: 1077–84.
- Centre for Research on the Epidemiology of Disasters (CRED). EM-DAT: the international disaster database. Brussels: Author; 2011. Available from: http://www.emdat.be [cited 21 January 2011].
- United Nations ESCAP. Statistical yearbook for Asia and the Pacific 2009. Thailand: ESCAP; 2010. Available from: http://www.unescap.org/stat/data/syb2009/1-Demographic-trends.asp [cited 30 March 2011].
- Phalkey R, Reinhardt JD, Marx M. Injury epidemiology after the 2001 Gujarat earthquake in India: a retrospective chart review of in-patients treated at a hospital in the Kutch district immediately after the disaster. GHA 2011; tbd(tbd): tbd.
- Li W, Qian J, Liu X, Zhang Q, Wang L, Chen D, et al.. Management of severe crush injury in a front-line tent ICU after 2008 Wenchuan earthquake in China: an experience with 32 cases. Crit Care. 2009; 13: R178.10.3402/gha.v4i0.7191.
- Qiu J, Liu GD, Wang SX, Zhang XZ, Zhang L, Li Y, et al.. Analysis of injuries and treatment of 3,401 inpatients in 2008 Wenchuan earthquake—based on Chinese Trauma Databank. Chin J Traumatol. 2010; 13: 297–303.
- Rathore MF, Rashid P, Butt AW, Malik AA, Gill ZA, Haig AJ. Epidemiology of spinal cord injuries in the 2005 Pakistan earthquake. Spinal Cord. 2007; 45: 658–63. 10.3402/gha.v4i0.7191.
- Yang C, Wang HY, Zhong HJ, Zhou L, Jiang DM, Du DY, et al.. The epidemiological analyses of trauma patients in Chongqing teaching hospitals following the Wenchuan earthquake. Injury. 2009; 40: 488–92. 10.3402/gha.v4i0.7191.
- Zhang L, Liu Y, Liu X, Zhang Y. Rescue efforts management and characteristics of casualties of the Wenchuan earthquake in China. Emerg Med J. 2011; 28: 618–22. 10.3402/gha.v4i0.7191.
- Redmond AD, Li J. The UK medical response to the Sichuan earthquake. Emerg Med J. 2011; 28: 516–20. 10.3402/gha.v4i0.7191.
- Bai XD, Liu XH. Retrospective analysis: the earthquake-injured patients in Barakott of Pakistan. Chin J Traumatol. 2009; 12: 122–24.
- Chiou-Tan FY, Bloodworth DM, Kass JS, Li X, Gavagan TF, Mattox K, et al.. Physical medicine and rehabilitation conditions in the Astrodome clinic after hurricane Katrina. Am J Phys Med Rehabil. 2007; 86: 762–69. 10.3402/gha.v4i0.7191.
- Nufer KE, Wilson-Ramirez G, Shah MB, Hughes CE, Crandall CS. Analysis of patients treated during four disaster medical assistance team deployments. J Emerg Med. 2006; 30: 183–87. 10.3402/gha.v4i0.7191.
- Centers for Disease Control and Prevention (CDC). Post-earthquake injuries treated at a field hospital—Haiti, 2010. MMWR Morb Mortal Wkly Rep 2011; 59: 1673–7.
- Guha-Sapir D, Vos F. Chapter 2: earthquakes, an epidemiological perspective on patterns and trends. In: Spence R, So E, Scawthorn C, Human casualties in earthquakes: progress in modelling and mitigation. New York: Springer. 2011, pp. 13–24.
- Priestley M, Hemingway L. Disability and disaster recovery: a tale of two cities?. J Soc Work Disabil Rehabil. 2006; 5: 23–42. 10.3402/gha.v4i0.7191.
- Ke X, Liu C, Li N. Social support and quality of life: a cross-sectional study on survivors eight months after the 2008 Wenchuan earthquake. BMC Public Health. 2010; 10: 573.10.3402/gha.v4i0.7191.
- Takahashi A, Watanabe K, Oshima M, Shimada H, Ozawa A. The effect of the disaster caused by the great Hanshin earthquake on people with intellectual disability. J Intellect Disabil Res. 1997; 41: 193–6. 10.3402/gha.v4i0.7191.
- Tanida N. What happened to elderly people in the great Hanshin earthquake. BMJ. 1996; 313: 1133–5.
- Chou YJ, Huang N, Lee CH, Tsai SL, Chen LS, Chang HJ. Who is at risk of death in an earthquake?. Am J Epidemiol. 2004; 160: 688–95. 10.3402/gha.v4i0.7191.
- Osaki Y, Minowa M. Factors associated with earthquake deaths in the Great Hanshin-Awaji Earthquake, 1995 [in Japanese]. Nippon Koshu Eisei Zasshi. 1999; 46: 175–83.
- Rathore MF, Butt AW, Aasi MH, Farooq F. Re: complications in patients with spinal cord injuries sustained in an earthquake in northern Pakistan. J Spinal Cord Med 2008; 31: 118; author reply 118.
- Rathore MF, Farooq F, Butt AW, Gill ZA. An update on spinal cord injuries in October 2005 earthquake in Pakistan. Spinal Cord. 2008; 46: 461–2. 10.3402/gha.v4i0.7191.
- Gosney JE. Physical medicine and rehabilitation: critical role in disaster response. Disaster Med Public Health Prep. 2010; 4: 110–12. 10.3402/gha.v4i0.7191.
- Kelen GD, Kraus CK, McCarthy ML, Bass E, Hsu EB, Li G. Inpatient disposition classification for the creation of hospital surge capacity: a multiphase study. Lancet. 2006; 368: 1984–90. 10.3402/gha.v4i0.7191.
- Smith K, Petley DN. Environmental hazards: assessing risk and reducing disaster5th ed. Routledge. New York, 2009
- Teal GE, Barnes SM, Moeller WA, Fabrizio RA, Phostole V, Kaplan BM. Training requirements for postattack adaptive behavior. Report prepared for the USA Army Office of Civil Defense. 1965. Available from: http://www.dtic.mil/dtic/tr/fulltext/u2/624870.pdf [cited 25 July 2011].
- Rathore FA, Farooq F, Muzammil S, New PW, Ahmad N, Haig AJ. Spinal cord injury management and rehabilitation: highlights and shortcomings from the 2005 earthquake in Pakistan. Arch Phys Med Rehabil. 2008; 89: 579–85. 10.3402/gha.v4i0.7191.
- Tauqir SF, Mirza S, Gul S, Ghaffar H, Zafar A. Complications in patients with spinal cord injuries sustained in an earthquake in Northern Pakistan. J Spinal Cord Med. 2007; 30: 373–7.
- Haig AJ, Im J, Adewole D, Nelson V, Krabak B. The practice of physical medicine and rehabilitation in sub-Saharan Africa and Antarctica: a white paper or a black mark?. J Rehabil Med. 2009; 41: 401–5.; Eur J Phys Rehabil Med 45: 185–91; PM & R 1: 421–6; Disabil Rehabil 31: 1031–7; Chinese J Rehabil Med 24: 385–9.10.3402/gha.v4i0.7191.
- Tinney M, Chiodo A, Haig A, Wiredu E. Medical rehabilitation in Ghana. Disabil Rehabil. 2007; 29: 921–7. 10.3402/gha.v4i0.7191.
- Raissi GR, Mokhtari A, Mansouri K. Reports from spinal cord injury patients: eight months after the 2003 earthquake in Bam, Iran. Am J Phys Med Rehabil. 2007; 86: 912–17. 10.3402/gha.v4i0.7191.
- Raissi GR. Earthquakes and rehabilitation needs: experiences from Bam, Iran. J Spinal Cord Med. 2007; 30: 369–72.
- OCHA ROMENACA. Humanitarian response—Haiti. Port au Prince: OCHA. ; 2010. Available from: http://haiti.humanitarianresponse.info/Default.aspx?tabid = 68 [cited 1 March 2010].
- Majchrzak A, Jarvenpaa SL, Hollingshead AB. Coordinating expertise among emergent groups responding to disasters. Organ Sci. 2007; 18: 147–61. 10.3402/gha.v4i0.7191.
- Ingstad B, Reynolds Whyte S, Disability and culture. Berkley: University of California Press. 1995.
- Rathore F, New P, Iftikhar A. A report on disability and rehabilitation medicine in Pakistan: past, present, and future directions. Arch Phys Med Rehabil. 2011; 92: 161–6. 10.3402/gha.v4i0.7191.
- Iezzoni LI, Ronan LJ. Disability legacy of the Haitian earthquake. Ann Intern Med. 2010; 152: 812–14.
- WHO. Guidelines on the provision of manual wheelchairs in less resourced settings. . Geneva: Author. ; 2008. Available from: http://www.who.int/disabilities/publications/technology/English%20Wheelchair%20Guidelines%20(EN%20for%20the%20web).pdf [cited 8 February 2011].
- Murray CJL, Lopez AD, Global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. The global burden of disease and injury. Vol. 1. Boston: Harvard University Press. 1990.
- Mont D. Measuring health and disability. Lancet. 2007; 369: 1658–63. 10.3402/gha.v4i0.7191.
- Grosse SD, Lollar DJ, Campbell VA, Chamie M. Disability and disability-adjusted life years: not the same. Public Health Rep. 2009; 124: 197–202.
- Cohen ME, Marino RJ. The tools of disability outcomes research functional status measures. Arch Phys Med Rehabil. 2000; 81: S21–S29. 10.3402/gha.v4i0.7191.
- Heinemann AW, Linacre JM, Wright BD, Hamilton BB, Granger C. Relationships between impairment and physical disability as measured by the functional independence measure. Arch Phys Med Rehabil. 1993; 74: 566–73. 10.3402/gha.v4i0.7191.
- Keith RA, Granger CV, Hamilton BB, Sherwin FS. The functional independence measure: a new tool for rehabilitation. Adv Clin Rehabil. 1987; 1: 6–18.
- Loar J, Haig AJ, Yamakawa KS, Baljinnyam A. Construct validation of the language independent functional evaluation versus the Barthel index in a Mongolian community. Disabil Rehabil. 2011; 33: 319–25. 10.3402/gha.v4i0.7191.
- WHO. WHODAS 2.0—World Health Organization disability assessment schedule 2.0. Geneva: World Health Organization. ; 2009. Available from: http://www.unescap.org/stat/disability/census-ws/WHODAS-English.pdf [cited 15 February 2011].
- de Ville de Goyet C. Editorial comments—“But for the hurricane”; measuring natural disaster mortality over the long term. Prehosp Disaster Med. 2007; 22: 152–3.
- Gosselin RA, Heitto M, Zirkle L. Cost effectiveness of replacing skeletal traction by interlocked intramedullary nailing for femoral shaft fractures in a provincial trauma hospital in Cambodia. Int Orthopedics. 2009; 33: 1445–8. 10.3402/gha.v4i0.7191.