Abstract
Background: Tuberculosis rates in the world remain high, especially in low- and middle-income countries. International tuberculosis (TB) policy generally recommends the use of directly observed therapy (DOT) to ensure treatment adherence.
Objective: This article examines a change in TB treatment support that occurred in 2005 in South Africa, from DOT to the enhanced TB adherence programme (ETA).
Design: Seven key individuals representing academics, policy makers and service providers involved in the development of the ETA programme or knowledgeable about the issue were purposively sampled and interviewed, and participant observation was conducted at ETA programme steering group meetings. Qualitative content analysis was used to analyse the data, drawing on the Kingdon model of agenda setting. This model suggests that three independent streams – problem, policy and politics – come together at a certain point, often facilitated by policy entrepreneurs, to provide an opportunity for an issue to enter the policy agenda.
Results: The results suggest the empowerment-oriented programme emerged through the presence of policy entrepreneurs with access to resources. Policy entrepreneurs were influenced by a number of simultaneously occurring challenges including problems within the existing programme; a perceived mismatch between patient needs and the existing TB treatment model; and the TB-HIV co-epidemic. Policy entrepreneurs saw the ART approach as a possible solution to these challenges.
Conclusions: The Kingdon model contributed to describing the process of policy change. Research evidence seemed to influence this change diffusely, through the interaction of policy entrepreneurs and academics.
More than 2 million people continue to die from tuberculosis (TB) each year. However, the international policy to combat the epidemic, Directly Observed Therapy, Short Course (DOTS), has remained largely unchanged during the last decade. A total of 202 countries worldwide reported implementing the strategy in 2008 Citation1, making it highly successful in terms of national alignment.
While DOTS has helped improve TB outcomes Citation2, DOT, one of its components, is widely contested. Researchers have suggested that DOT may not be a useful approach to treatment Citation3 Citation4, and it is seen as being dehumanizing Citation5, difficult for patients Citation6, and lacking a patient-centred approach Citation7. Although the Stop TB policy has evolved to include a focus on community participation and empowerment Citation8, the DOT component has remained relatively unchanged. However, some modifications have been made in different settings, for example in the choice of treatment observer Citation9, which in some settings may be a community-based lay health worker Citation10.
The use of DOT is also challenged by the close relationship between TB and HIV Citation11. For example, in South Africa approximately 58% of people with TB are estimated to be HIV positive Citation12 and many require treatment for both conditions. However, patients often receive TB medication through DOT and antiretroviral therapy (ART) through supported self supervision. While DOT could be seen as having a focus on the control of patients Citation13, the ART community treatment programme could be seen as facilitating the empowerment of people living with HIV/AIDS Citation14. The ART programme is reported to have achieved good outcomes in selected settings (over 90% at 6 months) Citation15. Though adherence rates to TB and ART programmes are difficult to compare directly, TB treatment programmes continue to perform poorly in similar settings (the TB treatment success rate was approximately 74% in 2006 in South Africa Citation12). An argument could therefore be made that the ART approach should be adapted for the delivery of TB treatment.
The DOTS strategy is of particular interest given its global influence, and the way in which the policy has been transferred from the WHO to most countries in the world Citation16. The DOT approach also has considerable staying power despite available research evidence suggesting that it may not improve TB treatment outcomes Citation4. It is therefore notable when a programme – the Enhanced Tuberculosis Adherence (ETA) programme – that is not strictly aligned with this approach is systematically developed and implemented, as happened in Cape Town, South Africa. Though the programme was developed and implemented at local and provincial levels, it may have implications for national and international policies on TB treatment (See for a detailed description of the programme).
Table 1. Comparison of the directly observed therapy (DOT) and enhanced tuberculosis adherence treatment programme (ETA)
An important question is why a decision was taken in 2005 to develop and implement this new TB treatment approach in Cape Town. Attempting to identify the cause for this programme change could help researchers and other stakeholders understand and influence future policy making Citation17 Citation18. Such analysis could also provide broader information on agenda setting in low- and middle-income contexts, on which there is little empirical evidence Citation19. Therefore, the aim of this study was to examine, using the Kingdon framework of agenda setting, the background to the development of the ETA programme in order to understand why this change in treatment models occurred at this time.
Methods
Theoretical framework
The Kingdon model was chosen as it examines how issues come onto policymakers’ agendas Citation20, and can help in establishing why an issue emerges at a particular point in time. This model has been used previously in analysing agenda setting in both high-income and low- and middle-income contexts Citation16 Citation21. Though the model is usually applied to agenda setting at the international and national levels, there are a number of examples of its application at a local level Citation22 Citation23. The model includes three streams: (1) the ‘problems’ stream, referring to perceptions of problems as public matters requiring attention; (2) the ‘policies’ stream (or solutions to the problem), which consists of ongoing analysis of problems and their solutions, and the debates and discussions surrounding them, and (3) the ‘politics’ stream, which includes the local and national mood, elections, or pressure from interest groups. The three streams are independent of one another, and flow in parallel Citation20. The coming together of these streams, often facilitated by ‘policy entrepreneurs’, can lead to the opening and closing of ‘policy windows’, or opportunities for shifting an issue onto an agenda Citation20.
Study setting
South Africa has the third largest burden of TB in the world with an estimated incidence rate of newly diagnosed smear positive TB cases of 358/100,000 in 2007 Citation12 and high TB–HIV co-infection rates Citation12. In the City of Cape Town health district, the incidence of smear positive tuberculosis was approximately 283.4 cases per 100,000 residents in 2007 Citation24. TB control within South Africa is organised according to the internationally recommended STOP TB policy. The line of TB management goes from district health services, to provincial health, to the National Department of Health which has political oversight and responsibility Citation25, and which provides a supporting function to lower levels of health services.
The ETA programme was piloted in five primary health care clinics in Cape Town in the Western Cape Province from 2006. The TB programme in Cape Town is managed by the City Health Department, in collaboration with provincial health authorities and local non-governmental organisations (NGOs).
Materials, respondents and data collection
The lead author carried out key informant interviews approximately 3 months after the start of the intervention. Participants included one senior and one middle-level policy maker and three programme managers from the NGO and the local health authority, and two public health academics with extensive knowledge of TB policy development in South Africa. Some of the respondents had been involved in policy development on a provincial and national level. Not all respondents had been part of the development and implementation of the ETA programme, and therefore participants represented both ‘insiders’ and ‘outsiders’. Respondents were selected purposively Citation26 on the basis of being able to describe the treatment model's development or implementation in detail, and to provide a range of views regarding the research question. Further interviews were conducted with one service provider and the two academics, not included in the first round of interviews, 1 year after the start of implementation of the programme. All but one of the interviewees were female.
The initial interview schedule included open-ended questions and focused on the events leading to the development of the ETA programme; challenges and expected benefits of the model; and who the key players were and their roles. Probes were used to explore respondents’ responses. The question guide was modified after preliminary analysis using the Kingdon model. A professional transcriber transcribed the audio-recorded interviews.
SA also participated in ETA programme steering group meetings throughout the planning and implementation of the new model and was in constant contact with the services during implementation. Notes taken at these meetings, and informal discussions and observations during fieldwork, complemented the interview data and were drawn on during the analysis. This study formed part of a larger evaluation of the ETA programme, the results of which are reported elsewhere Citation27–Citation29.
Ethical permission for the study was obtained from the Medical Research Council of South Africa and the Centers for Disease Control, Atlanta, United States. Permission was also obtained from the relevant health authorities. All respondents signed consent forms.
Analysis
Analysis was both inductive and deductive in approach. After the first three interviews, SA and SL conducted preliminary analysis, following which further interviews were undertaken Citation30 and further analysis conducted by the study team. Qualitative content analysis Citation31, which assists in analysing text to identify core consistencies and meanings Citation32, was used (see for an example). The notes and minutes of steering group meetings were referred to during analysis. This, and the use of multiple researchers from different backgrounds, provided a form of triangulation and added validity. The principle of ‘fair dealing’ Citation33, where all expressed opinions were taken into account regardless of whether they conflicted with the majority view, was used during analysis, and participants’ conflicting opinions were reflected in the emerging findings. Following this data analysis, the themes were examined and organised for their relation to Kingdon's model of agenda setting Citation20. Quotes from all respondents are included in the text in order to illustrate the findings.
Table 2. An example of the analysis methods
Results
The ETA programme was developed initially through discussions between two key individuals in the health services’ TB programme. After the concept was developed, one of the main NGOs providing TB treatment support in the area was approached for consultation and participation. The City and the NGO further developed materials and guidance for the implementing clinics and established a steering committee. The concept and the programme were further refined in steering group meetings both before and during the implementation. outlines a chronology of events relating to TB control in South Africa, together with publications that may have influenced stakeholders’ views. The following section describes how the change in programme occurred, from the perspective of key informants interviewed after the development of the programme. The main themes are summarised in .
Fig. 1. Timeline of key events in TB control in South Africa from 1995 to 2010. *No calculated incidence rate was available from the WHO. ART, Antiretroviral treatment; DOT, Directly Observed Therapy; DOTS, Directly Observed Therapy, Short Course; ETA, Enhanced Tuberculosis Adherence; HIV, Human immunodeficiency virus; TB, tuberculosis.
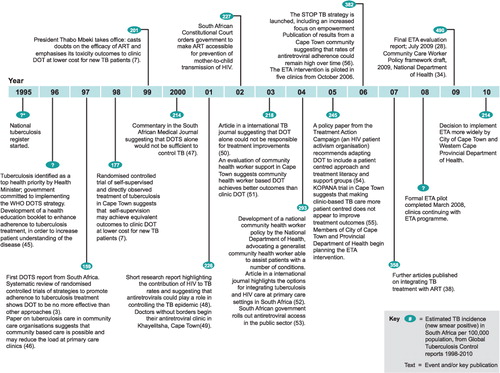
Table 3. Summary of main findings
Problems stream
Respondents noted that the ETA was developed because programme planners realised that the existing organisation of TB control was not achieving targets. The clinic environment was described as ‘chaos’, with insufficient staff and high caseloads. Many of the problems mentioned, however, were not new to the TB control programme and not specific to TB control only.
Management of the existing DOT programme
Overburdened clinics and rising caseloads were an ongoing concern. Many patients were made to come into the clinic every day to take their tablets, but had little understanding of why this was necessary. The management of a large number of lay health workers, tasked with providing community-based DOT support in the existing TB programme, was described as a ‘logistic nightmare’ (policy maker 1). In addition, it seemed that service providers felt that they were not in control of these workers due to the complex interactions between the NGOs providing the services and the health authority responsible for TB control. These and other shortcomings of the DOTS model were described at length both in interviews and steering group meetings. Though all respondents recognised that DOTS had provided good infrastructure for treatment, some also pointed out that the approach focused on technology instead of people – it was seen as a public health programme, where ‘… the group [and not the individual] is … important … and to cure all your sputum-positive patients because they're a threat to the population’ (researcher 1). Most also acknowledged that unsupervised treatment taking was taking place in any case:
It's not how the system was supposed to be, but because of the sheer volume, patients were given pills and just told to please go and drink them at home and come back next week again’. (policy maker 2)
Mismatch between patient needs and the existing TB programme
All respondents contested the benefits of observation:
And what is the real benefit of watching people? The real benefit of watching people, in my view, is not at all confirmed because I remember in some clinics where we saw the patients, passing by the clinic, waving us goodbye, and they were supposed to come to be watched swallow the medication! But they didn't come. What do you do? You go running after them? You open their mouths and stuff the tablets down their throat? (programme manager 1)
Many spoke of how DOT was useful to only a few patients, which suggested a mismatch between patient needs and the existing strategy. Respondents also felt that DOT was not implemented in the field as originally planned, as it did not focus on mentoring the patient. Instead, it had become mechanical and focused on getting the patient to swallow their tablets:
… the way DOT was working, it was very kind of mechanical. You know, just signing cards without actually being able to have the sense of overall – where are the patients and how are they doing? And that was simply because the system was overwhelmed. (policy maker 1)
TB–HIV co-epidemic changing the disease landscape
The close involvement of some of the respondents in ART programme management, and their observation of its good treatment outcomes, was also a key driver of changes in TB care:
… what is the ART programme doing that they're getting such good adherence levels, but we in the TB programme have been administering treatment for so long and we can't achieve the same things …? (policy maker 2)
Comparisons between the ART programme and DOT were also raised frequently in steering group meetings. Furthermore, respondents noted that co-infected patients were having to navigate two different forms of treatment provision during DOT: patients who self administered ART were also required to attend the clinic daily for their TB medication:
… and you know, it is difficult when you've got somebody enrolled on these drugs for months if not years, and they're doing fine and don't even have TB, and suddenly you are going to ask them to come to the clinic on a daily basis to swallow a handful of tablets. (programme manager 1)
The risk of infection of HIV positive individuals at clinics where others were taking their TB treatment in the same place was highlighted, and the poor integration of DOT and ART programmes was lamented. However, some respondents noted that there were important differences in the treatment and monitoring of HIV and TB:
I'm not convinced that TB treatment and antiretroviral (ARV) treatment should be seen in exactly the same way. I think there are fundamental differences … it's a lot easier for a patient that stops the ARVs … with TB you don't have anything that can tell you that this patient is most likely not taking the medication. (programme manager 1)
Long clinic waiting times and the sheer numbers of people on DOT were also seen to be exerting increasing pressure on staff, who were described by most respondents as angry, burnt out, exhausted and overloaded. Respondents felt that the DOT component was designed for small caseloads, but that the HIV epidemic had increased caseloads so that DOT was no longer appropriate: ‘But I am a hundred percent convinced that we can't carry on using the same old model in these new days’ (programme manager 1).
Policies and solutions stream
As the ART programme had achieved good adherence outcomes, it was seen as a promising model for TB control. In particular, respondents noted that it could provide a community or empowerment perspective to treatment and provide additional human resources through employing more skilled lay health workers to take on tasks previously done by nurses. In addition, they thought it could improve management by clarifying the roles of different cadres of health care provider, and free up staff time to attend to patients with problems. Some respondents also mentioned the potential of using this model to better integrate TB treatment with other treatment programmes: ‘It's too expensive to do it just for TB. It's too expensive just to do it for TB and ARVs. It should be a primary care model in which you have people visiting the homes everyday’ (researcher 1). However, respondents also recognised that though the new programme had potential, it was not the ultimate solution: ‘if you are in a dysfunctional place like [clinic name] you can't… it needs support; it needs good management; it needs to have an infrastructure before you implement something like this. It's not a cure all’ (policy maker 1). Others reported that they had had reservations about the programme prior to implementation, as it was so different from the DOT model:
… when I started with the project, I wasn't very positive about it. Because remember, I came in afterwards. I had to sit down … first before I could physically take on [the project] and understand where we were going with it. (programme manager 2)
A community empowerment perspective
A grass-roots approach to treatment was seen as important, including involving the community and the patient in treatment. Some, however, saw the change as shifting responsibility for treatment to the lay health worker and patient – and noted that this did not absolve the health system from responsibility: ‘… we can allow community people to help us take responsibility for our patients although it doesn't absolve or abdicate any responsibility that facility staff might have …’ (policy maker 2).
It was also notable that the programme was itself implemented from the senior management level, with little consultation with communities or the clinic involved:
… one of the problems [is], that the facility managers and the rest of the nursing staff were only brought onboard well into the … almost when it was ready to be implemented. (programme manager 3)
The NGO that employed and managed the lay health workers was always seen as closely involved in the implementation, and achieving a more community-based programme depended on the NGO's performance. However, the NGO was not involved from the start in discussions on possible solutions and some programme managers expressed reservations regarding the NGO's capacity to implement the programme.
Human resources
The programme's approach of having skilled lay health workers, with higher levels of literacy, and also with greater accountability both to the NGO and the health services, was also seen as a solution to the human resource crisis. However, some lamented the loss of ‘old’ lay workers, who were seen as more committed to their patients, though they had lower levels of literacy. In addition, the new programme provided an opportunity for improved teamwork, and respondents felt that this could contribute to dispelling the distrust prevailing between professional staff and lay health workers:
…I mean, we are all part of the team. If we work in this facility as a team we have to adhere to certain principles … And that will also encourage better working relationships and maybe better outcomes. (programme manager 2)
Improved management
Improved management of the programme and increased accountability to the health services was raised as a response to poor outcomes: ‘Because I think in the past, what we've done is we've come to devolve all responsibility to [the relevant NGO] – and you can't really do that. You know, the line management still kind of has to be … accountability has to lead back to the clinic’ (policy maker 1) and ‘… there were big gaps that we really needed to try and tighten up on’ (policy maker 1). Management and accountability could be improved through increasing teamwork between facility staff and lay health workers, and by asking lay health workers to document their work. Though this was seen by most as a solution to managing lay health workers, some questioned whether this was feasible in practice: ‘… do they really understand? Do we expect too much of them, especially with the paperwork? You know, the control from our side’ (programme manager 2). Respondents also raised concerns about the amount of work that was required from lay health workers, in return for low remuneration.
While patients would receive treatment support from community-based lay health workers and information from lay adherence counsellors, professional nursing staff could focus on paperwork and have more time to follow up problem cases: ‘And also, I think what we solved is the time it would free up for them to devote to the more difficult patients – so decreasing their workload’ (policy maker 2).
Politics stream
The dissident province
The new programme was made possible by key individuals – policy entrepreneurs – with access to information and resources. At the time when a new approach was being considered, programme managers were attending meetings in which the ART programme, sexually transmitted infections (STIs) treatment and voluntary counselling and testing (VCT) were being discussed. These had provided ideas for the ETA programme. Individuals participating in these meetings noted that these programmes were performing much better than the TB programme and considered what could be learnt from these, and implemented in the TB programme. The emergence of the ETA programme onto the agenda needs, however, to be seen within its local context. The Western Cape Province, according to respondents, had a history of dissenting with national and international TB policies:
… The Western Cape has always been seen, because it has more resources and it's been better managed, as a kind of odd one out. And they haven't always accepted at face value what the national department dishes up … (researcher 2).
Academics, policy makers and practitioners originating from the Western Cape had initially resisted the DOTS policy as well as South Africa's policy of DOT for the full 6 months of TB treatment. These academics had conducted evaluations that contested the effectiveness of DOT Citation4 Citation7 and the respondents were aware of this research, through interactions with academics in meetings and symposia. Respondents felt one of the reasons for the Western Cape's ability to contest national programmes was its high level of management, financial and human resources.
The need for services to adopt an empowerment approach
Respondents spoke of how, since South Africa's democratic elections in 1994, empowerment, including of users of health services, was a key theme nationally: ‘[the] whole move has been towards empowering people on the ground, and the TB system in particular was a very disempowering one …’ (researcher 2). Both the empowerment of patients and of lay health workers were reported as being central to the new programme: ‘… that for me is probably the single biggest thing – the empowerment of the patient in this whole setup’ (programme manager 3). Worker rights had also been at the forefront nationally, possibly leading to attempts to improve nurse working conditions: ‘I think politically we have gone through a phase of feeling that … I mean, workers’ rights are predominant’ (researcher 2).
The community or lay health worker policy
Shifts in policy nationally towards a ‘generalist’ lay health worker model also influenced the development of the new approach (see Citation33). As one respondent noted, there was a ‘… call from the national health department that people in organisations with vertical programmes would not be funded … had to start working as an integrated model of care where one carer would address all the problems of a particular person’ (programme manager 3). Participants also spoke of a wider, long term vision in which the ETA programme would be expanded to encompass lay health workers delivering other health promotion or treatment activities in addition to TB treatment support.
The growing ART programme
Lastly, political lobbying for universal access to ART contributed to the ETA programme's emergence. The high rate of co-infection; political lobbying for greater attention to TB among people living with HIV/AIDS; and the move towards integrating TB and ART all contributed to the programme's development. Respondents also highlighted problems of sustainability and affordability with regard to disease-specific interventions, suggesting that more integrated approaches were more sustainable: ‘… but I can't see with six million people needing ARVs in the next three to four years, how else we're going to do it … before we can even afford the ARVs’ (researcher 1).
Discussion
The decision to develop and implement the ETA was influenced by ongoing numerous problems within the TB care system, which were seen to threaten the effectiveness of the programme. It was also influenced by an available solution in terms of the ART support model; and a political climate that was amenable to change. In addition, increased pressure was being placed on services to provide TB treatment that was aligned with human rights and more patient centred approaches Citation35. Though many of these factors are interdependent, the coming together of these issues resulted in a window of opportunity. However, the results also suggest that the coming together of these factors at a particular time was facilitated by key individuals or ‘policy entrepreneurs’ within the health services, who could see both the problems and solutions, and could act as advocates for the change. These individuals also had access to resources, connections to researchers, and were able to initiate the required health systems changes.
Though the ETA could be seen to run contrary to the DOT component of the international DOTS strategy, it addressed many of the key health systems issues being discussed in South Africa at the time. As others have noted in relation to other policy changes Citation21, the political climate influenced the adoption of ideas into policy. In this case this climate included a readiness to accept a more empowering and less restrictive TB treatment programme and external pressure from interest groups such as the Treatment Action Campaign Citation35 and academics to change the TB control system Citation36. Other key issues included the new and evolving national community health worker policy Citation34 Citation37; the need for TB-HIV treatment integration Citation38; and efforts to ensure universal access to HIV treatment Citation39. In particular, the issues of empowerment and patient centredness were seen as key to the development of the ETA programme, and emerged when participants talked of the health services and communities. Agency and empowerment were important themes in this study. Despite this focus on empowerment, the implementing NGO was only brought on board after many of the key ideas had been developed, and there was little consultation with community members. Therefore, though the empowerment and grass-roots approach was discussed at length by many respondents, it is possible that the health systems challenges exerted more influence on the development of the ETA. Of course, all of the factors leading to this programme change need to be seen within the context of the larger challenges facing the health system in South Africa Citation40 Citation41 and the national TB crisis. These challenges may have expedited the decision to modify the TB programme.
It is notable that significant research over almost two decades contesting the effectiveness of DOT had been undertaken in the Western Cape and that the key individuals responsible for the programme change had interacted with researchers and were aware of these findings (e.g. Citation3 Citation7). Though informants mentioned the influence of research and researchers only in passing, it could be assumed that researchers had been part of the change, at least as ‘hidden participants’. ‘Hidden’ participants can have important influences on policy processes Citation16. The study respondents operated in the same networks as the authors of publications contesting DOT, which may have contributed toward an openness to considering alternatives to DOT. They were also resourceful and innovative individuals, willing to test new alternatives to achieve better results. Other studies have also highlighted the roles in influencing positively the uptake of research results of networks involving both key individuals in policymaking positions and researchers Citation21. However, research is said to influence policies only diffusely Citation42, and the pathways through which research influences policy are complex Citation18. This may explain in part the slow speed with which research findings were taken up by the services in the study context. The results of this study suggest that researchers, in addition to analysing problems and interacting with policy makers, should pay attention to available solutions at opportune political moments – that is, when there are ‘windows of opportunity’ Citation21 Citation43. Action research models Citation44, in which research and programme development go hand-in-hand, and policymakers, programme managers, service users and researchers collaborate in studying phenomena, may facilitate this process.
The Western Cape Province's history of challenging national and international TB control policies may also have influenced the opening of a window of opportunity for change. In contrast, another study of agenda setting at local level suggested that the extent to which a local policy is compatible with national policies was an important influence on the opening of a policy window Citation22. This highlights the complex relations, in understanding agenda setting, between national and local jurisdictions and policies as well as in the roles of factors such as service organisation and country context.
The study is based on key-informant interviews and the results relate to the specific context from which they were drawn. Though the study included only seven key informants, the in-depth nature of the interviews resulted in the collection of a very rich dataset. Additional interviews at higher management levels, such as in the National Department of Health, could have provided different perspectives. However, none of the respondents identified the National Department of Health as an important stakeholder in this process. We would argue that the approach used provided sufficient information to address the research question. A potential limitation is that respondents were asked, during the period in which the programme was already running, to recall issues leading to the earlier development of the programme. They may therefore have highlighted issues that they saw as important at the time of implementation rather than during the development of the programme. However, the recall period was fairly short (approximately 1 year), and interviews were complemented by information gathered at steering group meetings.
Our results contribute to understanding the complexities of agenda setting and programme and policy change in settings with considerable health system challenges, and suggest that well placed individuals, or ‘policy entrepreneurs’, are central to changing programmes and policies. The Kingdon model Citation20 offered a framework with which to understand the agenda setting process in this context. A challenge in applying this model to a programme change such as the ETA is identifying the appropriate level at which to consider the influences of the political climate (the politics stream). DOTS is an international policy and there are complex interactions between the local, national and international political and policy environments in terms of its implementation. Further examination of the impact of these different policy levels on agenda setting in different contexts could be useful.
Conclusion
Despite considerable research evidence being available for some time that DOT is no more effective than other treatment support strategies for TB Citation4, policies in the study setting, as elsewhere, had not shifted significantly towards a more patient empowerment-based approach prior to the development of the ETA programme. This study suggests that the availability of research evidence may not be sufficient to change policies, and that interactions between policymakers, programme managers and researchers are necessary to translate evidence into new policy initiatives. As postulated by Kingdon Citation20, there was a coming together of a number of factors at a particular time, facilitated by key individuals or policy entrepreneurs in a well resourced setting that enabled the development of the new programme.
Authors’ contributions
SA and SL conceptualized the study and designed data collection instruments. SA collected the data. SA analysed the data with consultation from SL, AT and KCR. SA drafted the first manuscript, and all authors contributed to revising and editing the manuscript.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
Acknowledgements
This study was funded by the Medical Research Council, South Africa, and Centers for Disease Control, Atlanta, US. We would like to thank all the researchers, policy makers and programme managers from the City of Cape Town and TB-HIV Care who planned and managed the programme, and took part in the interviews that form the basis of this work. To protect the anonymity of those who participated in interviews, none of the individuals who were part of the programme implementation or design are named here. We would also like to thank the lay health workers, healthcare staff and patients who made the programme possible.
References
- Lönnroth K, Gastro KG, Chakaya JM, Chauhan LS, Floyd K, Glaziou P, et al.. Tuberculosis control and elimination 2010–2050: cure, care and social development. Lancet. 2010; 375: 1814–28. 10.3402/gha.v5i0.14385.
- Garner P, Smith H, Munro S, Volmink J. Promoting adherence to tuberculosis treatment. Bull World Health Organ. 2007; 855: 404–06. 10.3402/gha.v5i0.14385.
- Volmink J, Garner P. Systematic review of randomised controlled trials of strategies to promote adherence to tuberculosis treatment. BMJ. 1997; 31: 1403–6. 10.3402/gha.v5i0.14385.
- Volmink J, Garner P. Directly observed therapy for treating tuberculosis. Cochrane Database of Systematic Reviews. 2007; (Suppl. 4): Art. No.: CD003343. DOI: 10.3402/gha.v5i0.14385.
- Noyes J, Popay J. Directly observed therapy and tuberculosis: how can a systematic review of qualitative research contribute to improving services? A qualitative meta-synthesis. J Adv Nurs. 2007; 57: 227–43. 10.3402/gha.v5i0.14385.
- Munro S, Lewin S, Smith H, Engel M, Fretheim A, Volmink J. Patient adherence to tuberculosis treatment: a systematic review of qualitative research. PLoS Med. 2007; 4: e238.10.3402/gha.v5i0.14385.
- Zwarenstein M, Schoeman JH, Vundule C, Lombard CJ, Tatley M. Randomised controlled trial of self-supervised and directly observed treatment of tuberculosis. Lancet. 1998; 352: 1340–3. 10.3402/gha.v5i0.14385.
- Stop TB Partnership. The global plan to stop TB 2011–2015: transforming the fight – towards elimination of tuberculosis. Geneva: World Health Organization. 2010.
- Macq JCM, Theobald S, Dick J, Dembele M. An exploration of the concept of directly observed treatment (DOT) for tuberculosis patients: from a uniform to a customised approach. Int J Tuberc Lung Dis. 2003; 7: 103–9.
- Dick J, Schoeman JH, Mohammed A, Lombard C. Tuberculosis in the community I: evaluation of a volunteer health worker programme to enhance adherence to anti-tuberculosis treatment. Tuber Lung Dis. 1996; 77: 274–9. 10.3402/gha.v5i0.14385.
- Hanekom WA, Lawn SD, Dheda K, Whitelaw A. Tuberculosis research update. Trop Med Int Health. 2010; 15: 981–9. 10.3402/gha.v5i0.14385.
- World Health Organisation. South Africa: tuberculosis profile. Geneva: World Health Organization. 2010.
- Harper I. Extreme condition, extreme measures?’ Compliance, drug resistance, and the control of tuberculosis. Anthropol Med. 2010; 17: 201–14. 10.3402/gha.v5i0.14385.
- Gruskin S, Ferguson L, Bogecho DO. Beyond numbers: using rights-based approaches to enhance antiretroviral treatment scale-up. AIDS. 2007; 21(Suppl. 5):S13–9. 10.3402/gha.v5i0.14385.
- Pienaar D. Determinants of adherence amongst patients established on antiretroviral therapy in Cape Town, South Africa. University of Cape Town. Cape Town, 2008
- Ogden J, Walt G, Lush L. The politics of ‘branding’ in policy transfer: the case of DOTS tuberculosis control. Soc Sci Med. 2003; 57: 179–88. 10.3402/gha.v5i0.14385.
- Walt G, Gilson L. Reforming the health sector in developing countries: the central role of policy analysis. Health Policy Plan. 1994; 9: 353–70. 10.3402/gha.v5i0.14385.
- Buse K, Mays N, Walt G. Making health policy. Open University Press. London, 2005
- Lavis J, Davies H, Oxman A, Denis JL, Golden-Biddle K, Ferlie E. Towards systematic reviews that inform health care management and policy making. J Health Serv Res Policy. 2005; 10: 35–48. 10.3402/gha.v5i0.14385.
- Kingdon JW. Agendas, alternatives and public policies2nd ed. Longman. New York, 2003
- Daniels K, Lewin S. The Practice Policy Group. Translating research into maternal health care policy: a qualitative case study of the use of evidence in policies for the treatment of eclampsia and pre-eclampsia in South Africa. Health Research Policy and Systems. 2008; 6(12):. DOI: 10.3402/gha.v5i0.14385. Website: http://www.health-policy-systems.com/content/6/1/12/ [cited 12 December 2011].
- Liu X, Lindquist E, Vedlitz A, Vincent K. Understanding local policymaking: policy elites’ perceptions of local agenda setting and alternative policy selection. Policy Stud J. 2010; 38: 69–91. 10.3402/gha.v5i0.14385.
- Ridde V. Policy implementation in an African state: an extension of Kingdon's multiple streams approach. Public Adm. 2009; 87: 938–54. 10.3402/gha.v5i0.14385.
- Loveday M. Section 5.2: Tuberculosis. In: CDay, FMonticelli, ESello, District health barometer 2007/08. Durban: Health Systems Trust. 2009, pp. 93–105.
- Atkins S, Chopra M. Chapter 3: Health systems. Primary health care: fresh perspectives. Pearson Education Publishers. Cape Town, 2009; 49–79.
- Green J, Thorogood N. Qualitative methods for health research. Sage. London, 2004
- Atkins S, Biles D, Lewin S, Ringsberg KC, Thorson A. Patient experiences of an intervention to support tuberculosis treatment adherence in Cape Town, South Africa. J Health Serv Res Policy. 2010; 15: 163–70. 10.3402/gha.v5i0.14385.
- Final evaluation report: enhanced tuberculosis adherence programme [database on the Internet]. Cape Town: Medical Research Council. 2009. Available from: http://www.mrc.ac.za/healthsystems/finalr.pdf [cited 29 November 2009].
- Atkins S, Lewin S, Jordaan E, Thorson A. Lay health worker supported tuberculosis treatment adherence in South Africa: an interrupted time series study. Int J Tuberc Lung Dis. 2011; 15: 84–9.
- Glaser BG, Strauss AL. The discovery of grounded theory: strategies for qualitative research. Aldine de Gruyter. New York, 1967
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and methods to achieve trustworthiness. Nurse Educ Today. 2004; 24: 105–12. 10.3402/gha.v5i0.14385.
- Patton MQ. Qualitative research and evaluation methods. Sage. LondonUK, 2002
- Mays N, Pope C. Qualitative research in health care: assessing quality in qualitative research. BMJ. 2000; 320: 50–2. 10.3402/gha.v5i0.14385.
- National Department of Health and Department of Social Development. Community care worker policy management framework (Draft version 6.0). PretoriaSA: RSA Department of Health & Department of Social Development. 2009.
- Treatment Action Campaign. Letter from international health and human rights experts to Mbeki and Zuma on the need for a human rights approach to TB. Cape Town: Treatment Action Campaign. 2008. [updated 13 December 2010]. Available from: http://www.tac.org.za/community/node/2384 [cited 13 December 2010].
- Maher D, Harries A, Getahun H. Tuberculosis and HIV interaction in sub-Saharan Africa: impact on patients and programmes; implications for policies. Trop Med Int Health. 2005; 10: 734–42. 10.3402/gha.v5i0.14385.
- Schneider H, Hlophe H, van Rensburg D. Community health workers and the response to HIV/AIDS in South Africa: tensions and prospects. Health Policy Plan. 2008; 23: 179–87. 10.3402/gha.v5i0.14385.
- Wood R. The case for integrating tuberculosis and HIV treatment services in South Africa. J Infect Dis. 2007; 196: S497–9. 10.3402/gha.v5i0.14385.
- National Department of Health. HIV & AIDS and STI strategic plan for South Africa 2007–2011. 2007. Available from: http://www.doh.gov.za/docs/misc/stratplan-f.html [cited 14 December 2010].
- Colvin CJ, Fairall L, Lewin S, Georgeu D, Zwarenstein M, Bachmann M, et al.. Expanding access to ART in South Africa: the role of nurse initiated treatment. S Afr Med J. 2010; 100: 210–2.
- Coovadia H, Jewkes R, Barron P, Sanders D, McIntyre D. The health and health system of South Africa: historical roots of current public health challenges. Lancet. 2009; 374: 817–34. 10.3402/gha.v5i0.14385.
- Gilson L, McIntyre D. The interface between research and policy: experience from South Africa. Soc Sci Med. 2008; 67: 748–59. 10.3402/gha.v5i0.14385.
- Lavis JN, Wilson MG, Oxman AD, Lewin S, Fretheim A. Support tools for evidence-informed health policymaking (STP) 4: using research evidence to clarify a problem. Health Res Policy Syst. 2009; 7(Suppl. 1):S4.10.3402/gha.v5i0.14385.
- Cornwall A, Jewkes R. What is participatory research?. Soc Sci Med. 1995; 41: 1667–76. 10.3402/gha.v5i0.14385.
- Dick J, Van der Walt H, Hoogendoorn L, Tobias B. Development of a health education booklet to enhance adherence to tuberculosis treatment. Tuber Lung Dis. 1996; 77: 173–7. 10.3402/gha.v5i0.14385.
- Maher D, Hausler H, Raviglione M, Kaleeba N, Aisu T, Fourie B, et al.. Tuberculosis care in community care organizations in sub-Saharan Africa: practice and potential. Int J Tuberc Lung Dis. 1997; 1: 276–83.
- Collins T. TB – are we losing the battle?. S Afr Med J. 2000; 90: 237–8.
- Bekker L, Wood R. Does antiretroviral therapy have a role to play in the control of tuberculosis in South Africa?. S Afr Med J. 2001; 91: 650–1.
- Médecins Sans Frontières. Khayelitsha 2001–2011: activity report – 10 years of TB/HIV care at primary health care level. Cape Town: Médecins Sans Frontières. 2001.
- Pope DS, Chaisson RE. TB treatment: as simple as DOT?. Int J Tuberc Lung Dis. 2003; 7: 611–5.
- Dudley L, Azevedo V, Grant R, Schoeman J, Dikweni L, Maher D. Evaluation of community contribution to tuberculosis control in Cape Town, South Africa. Int J Tuberc Lung Dis. 2003; 7(Suppl. 1):S48–55.
- Coetzee D, Hildebrandt K, Goemaere E, Matthys F, Boelaert M. Integrating tuberculosis and HIV care in the primary care setting in South Africa. Trop Med Int Health ; : a. 2004; 9: 11–5. 10.3402/gha.v5i0.14385.
- El-Khatib Z. Virologic failure and HIV-1 drug resistance among antiretroviral therapy recipients in an urban resource-limited setting – the South African Virologic Evaluation (SAVE) study. Karolinska Institutet. Stockholm, 2011
- Treatment Action Campaign. Steering the storm: TB and HIV in South Africa. 2005. Available from: http://www.tac.org.za/Documents/TBPaperForConference-1.pdf [cited 14 December 2010].
- Lewin S, Dick J, Zwarenstein M, Lombard CJ. Staff training and ambulatory tuberculosis treatment outcomes: a cluster randomized controlled trial in South Africa. Bull World Health Organ. 2005; 83: 250–9.
- Bekker L, Myer L, Orrell C, Lawn S, Wood R. Rapid scale-up of community-based HIV treatment service: programme performance over 2 consecutive years in Guguletu, South Africa. S Afr Med J. 2006; 96: 315–20.