Abstract
Background : Despite the publication of several studies on the subject, there is significant uncertainty regarding the burden of disease among adults in sub-Saharan Africa (sSA).
Objectives : To describe the breadth of available data regarding causes of admission to hospital, to systematically analyze the methodological quality of these studies, and to provide recommendations for future research.
Design : We performed a systematic online and hand-based search for articles describing patterns of medical illnesses in patients admitted to hospitals in sSA between 1950 and 2010. Diseases were grouped into bodily systems using International Classification of Disease (ICD) guidelines. We compared the proportions of admissions and deaths by diagnostic category using χ2.
Results : Thirty articles, describing 86,307 admissions and 9,695 deaths, met the inclusion criteria. The leading causes of admission were infectious and parasitic diseases (19.8%, 95% confidence interval [CI] 19.6–20.1), respiratory (16.2%, 95% CI 16.0–16.5) and circulatory (11.3%, 95% CI 11.1–11.5) illnesses. The leading causes of death were infectious and parasitic (17.1%, 95% CI 16.4–17.9), circulatory (16%, 95% CI 15.3–16.8) and digestive (16.2%, 95% CI 15.4–16.9). Circulatory diseases increased from 3.9% of all admissions in 1950–59 to 19.9% in 2000–2010 (RR 5.1, 95% CI 4.5–5.8, test for trend p<0.00005). The most prevalent methodological deficiencies, present in two-thirds of studies, were failures to use standardized case definitions and ICD guidelines for classifying illnesses.
Conclusions : Cardiovascular and infectious diseases are currently the leading causes of admissions and in-hospital deaths in sSA. Methodological deficiencies have limited the usefulness of previous studies in defining national patterns of disease in adults. As African countries pass through demographic and health transition, they need to significantly invest in clinical research capacity to provide an accurate description of the disease burden among adults for public health policy.
The health of adults in sub-Saharan Africa (sSA) is becoming an increasingly important priority in global health policy Citation1 Citation2. Recent improvements in the survival of children Citation3–Citation5 coupled with a reduction in total fertility mean that the proportion of the population that is adult is increasing rapidly, beginning with young adults Citation6. In any society adults are the economically productive age group. The survival of children is closely linked to that of adults and to maintain the gains made in reducing child mortality, the causes of early adult mortality need to be identified Citation7. Recent studies show that levels of adult mortality (i.e. death between the ages of 15 and 60) are 4–40 times higher in sSA than in developed countries Citation3 Citation8–Citation11.
The pattern of illnesses responsible for the high mortality among adults in sSA has not been well characterized Citation2 Citation9–Citation13. The World Health Organization (WHO) predicts that by 2020, the causes of disease and death in sSA will have undergone a significant shift towards endemic non-communicable diseases and away from infectious diseases Citation14. This shift will necessitate changes in the deployment of resources, both human and physical, to deal with new health challenges Citation15 Citation16. Currently very few health systems in low- and middle-income countries rely on research evidence for guiding policy interventions Citation17. As this transition occurs, accurate data on the burden of illnesses will be needed as there will be a double burden of endemic non-communicable and residual communicable diseases Citation2 Citation15 Citation18.
Community-based studies provide an accurate picture of the profile of the diseases of adults because they minimize the bias, inherent in hospital-based studies, of variable access to health care Citation19 Citation20. However, these surveys are expensive undertakings, and useful information could be gained from analysis of well-conducted routine population and clinical surveillance activities. There are currently substantial efforts to improve vital event registration including the introduction of verbal autopsy methods to better describe causes of death. However, the shortcomings of health facility-based studies have not been systematically analyzed in order to improve future work. Here we report a systematic review of descriptive studies of medical illnesses in adults admitted to hospitals in sSA between 1950 and 2010 to determine the causes of admission and death and to characterize the methodological features of such studies that are likely to yield useful data in the future.
Methods
Literature search
We searched PubMed, African Index Medicus, African Journals OnLine (AJOL) and EMBASE for articles describing the pattern of disease among adults admitted to hospital in Africa. The Internet search was performed on 3 July 2011 using the search filter ‘(medical OR hospital) AND admissions AND adults AND Africa’. We screened titles and abstracts of articles that met specific inclusion criteria and read those that were available online or from academic libraries that we had access to. We reviewed reference lists of selected articles to identify additional secondary articles not found during the online search. Our review was limited to articles either written in or translated into English.
Studies were eligible for inclusion in the review if they were conducted among adult patients admitted to hospitals in sSA between 1950 and 2010. We excluded studies if data on adult admissions could not be extracted from them, if the study was conducted during a period of war, if the articles focused on specific age sub-groups (e.g. adolescents, geriatrics), or if the focus of the study was on a single factor as a cause of admissions to hospital, for example, HIV, injuries or obstetric admissions.
Data extraction
We designed a data extraction form and entered the data from each paper into the form, which was later cross-checked for accuracy. The following data were collected from each study: country where the study was performed, study period, type of hospital, and number and causes of admissions and deaths. The diseases reported were grouped into body systems according to International Classification of Diseases (ICD) guidelines Citation21. We used the χ2 test to compare proportions of observations in each diagnostic category. We calculated risk ratios for disease changes over time by dividing the proportion of admissions and deaths in each category per decade by the corresponding value in the baseline period (1950–9) and we tested the trend in the sub-category with greatest changes by using the χ2 test for linear trend. p Values reported are two-sided and proportions reported with 95% confidence intervals (CIs). Data were analyzed using STATA® v11.
Review of methodological quality
We evaluated each paper using a uniform set of questions designed to gauge the quality of the studies. The criteria were adapted by the authors from the principles of descriptive epidemiology Citation22 Citation23 and the STROBE statement Citation24. The criteria and their justification are outlined in . Each criterion was assigned relative weights based on the authors’ assessment of their influence on study quality. We calculated the sum of all criteria scores to provide an overall methodological score for each study. We performed a methodological sensitivity analysis for the cause of death analysis by comparing the causes derived from studies ranked above the 75th percentile in their methodological score with the causes in the baseline analysis.
Table 1. Weighted criteria used in assessing methodological quality of studiesa
Results
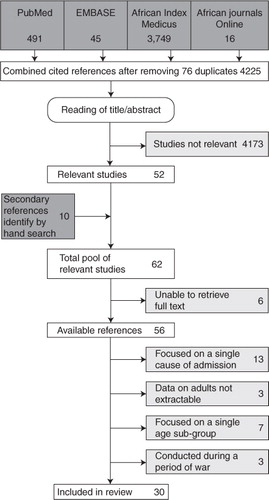
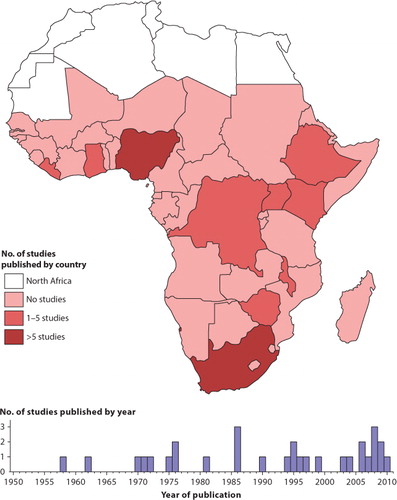
The online and hand-based search identified 56 relevant and obtainable full-text articles; 26 of these met the exclusion criteria leaving 30 full-text articles for inclusion in the review (). The geographic distribution of these studies by country and the number of studies published per year are shown in . The methodological characteristics of the studies included in the review are summarized in . The supplementary appendix () lists the studies that were excluded, with reasons.
Table 2. Characteristics of studies included in review
Table 3. Supplementary appendix Table S1. Studies excluded from review
Methodological quality
The median score for all the studies after applying weighted points to each aspect of the studies () was 55% (IQR 47.2–63.9). Only one study Citation25 satisfied all criteria on methodological quality.
Study design
Only 8 (27%) studies were prospective in nature, the most recent one having been completed in 1995 Citation25–Citation32. Five of these prospective studies were conducted in university teaching hospitals that had high-level staff and relatively advanced diagnostic facilities. However, given their urban location the results of these studies may not have been representative of the disease pattern in the majority of the population in the countries studied, a fact acknowledged by all the authors.
Use of standard case definitions
Four studies (13%) provided case definitions for the illnesses that were studied Citation25 Citation26 Citation33 Citation34. One study conducted in Uganda Citation30 provided a case definition for only one condition (anemia) but this differed from the standard WHO definition Citation35.
Use of international classification of diseases coding
All of the studies categorized illnesses into various bodily systems as a result of the multiplicity of diagnoses. However, only one third of the studies Citation25 Citation32 Citation34 Citation36–Citation41 used the WHO recommended ICD system that enables comparisons between studies and aggregation of data across different sites. In one study the coding of illnesses into ICD categories was done retrospectively Citation32.
Admission criteria
Thirteen studies mentioned the presence of admission criteria for patients to the hospitals where the studies were conducted but only five specified what these criteria were. Two of these studies were conducted in the same hospital at different time points, thus reducing the number of hospitals in which admission criteria were reported to four. In the five reports where admission criteria were described Citation25 Citation30 Citation32 Citation42 Citation43, they consisted of seriousness of the illness, referral from lower level facilities, and suitability for teaching and research with patients not meeting any of these criteria being referred to other facilities. The remaining reports did not specify what the admission criteria were.
Cadre of hospital staff
Most of the studies were conducted in hospitals that had consultants as the highest level of staff, and these were responsible for determining the final diagnosis given to patients. In four studies, all of which were conducted in rural areas, Medical Officers served as the highest cadre of medical staff Citation29 Citation34 Citation40 Citation44. In two studies, the level of training of the staff at the hospitals involved was not reported Citation45 Citation46.
Reporting on diagnostic facilities
We postulated that hospitals located in urban areas such as university teaching hospitals would have more advanced diagnostic facilities. Of the 14 studies carried out in university/teaching hospitals nine reported having class III diagnostic facilities Citation26–Citation28 Citation30 Citation42 Citation43 Citation47–Citation49. These included more advanced imaging, pathology, and biochemical tests. In three studies, autopsies were performed on more than 50% of deaths Citation30 Citation43 Citation49. Only one study carried out in a rural hospital had advanced diagnostic facilities thus limiting the range and accuracy of diagnoses for rural studies Citation40.
Reporting on case fatality rates
We found 18 (60%) studies that either reported case fatality rates for individual illnesses or overall in-hospital mortality for patients observed during the study periods. Three quarters of the studies giving mortality rates were conducted in hospitals located in urban areas.
Leading causes of hospital admission
We found 27 studies reporting data on 86,307 medical admissions for the period from 1950–2010 (). The proportions of admissions and deaths by ICD diagnostic category over the period are shown in . Infectious and parasitic diseases, including malaria, bacterial diseases, and HIV disease, were the leading cause of admission over the period accounting for 19.8% (95% CI 19.6–20.1) of all admissions. Respiratory illnesses were second accounting for 16.2% (95% CI 16.0–16.5) of admissions while diseases of the circulatory system were third at 11.3% (95% CI 11.0–11.5). When we restricted the analysis to admissions from studies that ranked above the 75th percentile in the methodological score, infectious and parasitic diseases, and respiratory illnesses remained the leading causes of admission, accounting for 27.4% (95% CI 26.9–27.9) and 18.4%(95% CI 18.0–18.9) of all admissions. The remaining leading causes of admission were in descending order: digestive system 13.9% (95% CI 13.6–14.3), genitourinary system 10.6% (95% CI 10.3–11.0) and circulatory system disorders 7.4% (95% CI 7.1–7.7). The class of disease among all admissions varied with time in decades (χ2=14,000, df 30; p<0.0005). The proportion of admissions due to circulatory system disorders increased five-fold over the period from 3.9% of admissions in 1950–59 to 19.9% of admissions in 2000–2010 (RR 5.1, χ2 test for trend p<0.00005). Infectious and parasitic diseases decreased from 18.2% to 13.9% of all admissions over the period, a 24% decrease (RR 0.76, 95% CI 0.71–0.82). Respiratory illnesses decreased from 16.2% of all admissions to 7.7% (RR 0.47, 95% CI 0.44–0.51). Endocrine and nervous system disorders increased significantly over the period, although each accounted for less than 5% of all admissions (Table S2).
Fig. 3. Temporal distribution of admissions and deaths by ICD diagnostic category* A) Frequency of admissions per decade by ICD diagnostic category. B) Frequency of deaths per decade by ICD diagnostic category.
Note: For each decade the leading diagnostic categories for both admissions and deaths are shown. The width of the columns is proportional to the amount of observations available for each decade. Detailed data regarding all causes of admission and death for each period can be found in the supplementary appendix.
*Some studies compared diseases over two time periods, both periods were included. Observations for studies that were conducted over several decades were equally split over the duration of the study if the temporal distribution of admissions/deaths had not been reported.
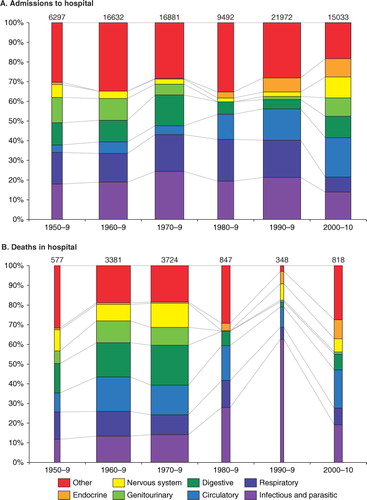
Table 4. Numbers of admissions and deaths for each decade*
Leading causes of in-hospital mortality
We obtained in-hospital cause of death data for 9,695 patients from 15 studies for the period 1950–2010 (Table S2, ). Infectious and parasitic diseases, disorders of the circulatory system, and digestive system disorders were the leading causes of death accounting for 17.1% (95% CI 16.4–17.9), 16.0% (95% CI 15.3–16.8), and 16.2% (95% CI 15.4–16.9) of all deaths, respectively. The class of disease among all deaths varied with time in decades (χ2=1100, df 30; p<0.0005). The proportion of deaths caused by disorders of the circulatory system rose from 9.7% in 1950–59 to 19.4% in 2000–2010 (RR 2.0, 95% CI 1.5–2.7, χ2 test for trend p=0.08). Deaths caused by infectious and parasitic diseases rose from 11.8% in 1950–9 to 19.2% in 2000–2010 (RR 1.6, 95% CI 1.3–2.1). Comparison of the proportion of deaths caused by digestive system disorders at the beginning of the study period and at the end showed a decrease from 14.9% to 8.1% (RR 0.54, 95% CI 0.40–0.73). Deaths due to disorders of the endocrine, nervous, and genitourinary systems all showed significant decreases (Table S2), but the combined contribution of these diagnostic categories to overall mortality was less than 20%. When we restricted the analysis of causes of death to studies that ranked above the 75th percentile on the methodological score, we observed no meaningful changes in the result.
Case fatality rates for the entire period for different disease categories could not be calculated because of inconsistent reporting on the number of patients admitted with each medical condition. Two recent retrospective studies reported case fatality rates and the diagnostic categories with the highest case fatality rates were infectious and parasitic diseases (25%) and circulatory illnesses (21%) Citation25 Citation33.
Discussion
We found 30 eligible studies conducted in 10 sub-Saharan countries and covering a 61-year time period. In most African countries in there are no published data on hospital deaths () and our illustration of research activity trends () provides no evidence that this situation is improving over time. All of this is in spite of the fact that Africa bears nearly a quarter of the world's burden of disease Citation50.
Despite the limitations identified in the few studies obtained, as indicated by the low methodology scores, some trends were discernible; for example, the proportion of admissions due to cardiovascular illnesses, composed mainly of stroke and heart failure, were found to have increased significantly over the study period. The proportion of admissions due to infectious and parasitic diseases decreased over the study period. However, the proportion of deaths caused by infectious and parasitic diseases increased during the period, which roughly coincides with the emergence of the HIV epidemic. HIV-related illnesses contributed the most to the burden of infectious disease over the past 10 years with a very high case fatality, suggesting that late presentation, due to limited access to HIV testing facilities, continues to be a significant problem on the continent Citation51. HIV may also increase the risk of heart diseases such as cardiomyopathy Citation52 and cancers Citation53 providing one illustration of the links between communicable and non-communicable diseases. Due to the limitations of the data, it is difficult to determine whether or not the observed trends were a result of the ongoing epidemiological transition with an increased burden of non-communicable illnesses in the continued presence of HIV and other infectious diseases. The observed changes could be due to changing hospital admission policies, improved hospital access for certain age or disease groups or new treatment availability, factors that we were unable to examine. These would be acting in concert with other explanations for the increasing burden of non-communicable disease in sSA, including demographic changes resulting in an increase in the number of children surviving to adulthood Citation4 and an increase in the prevalence of cardiovascular risk factors such as hypertension and diabetes Citation54 Citation55. Consistent with these observations as well as our results, community-based data from South Africa showed an increase in non-communicable diseases as a cause of death between 1992 and 2005 Citation56. This was also accompanied by a large increase in HIV-related deaths Citation56. However, when compared to estimates based on the global burden of disease model Citation2, which is itself imperfect Citation57, our results suggest a bigger contribution from non-communicable diseases. These contrasting results emphasize the importance of defining patterns of disease accurately as the transition proceeds in order to allocate scarce health resources. Research activities and funding also need to be guided by the burden of disease but evidence from the developing world suggests that this does not always happen Citation58 Citation59.
This review also exposes the methodological deficiencies of the few studies that have contributed data, an issue that has received little attention Citation11. The most common shortcoming was the failure to use standard case definitions for the illnesses described. This is attributable to the fact that most of the studies were retrospective in design and it would have been difficult to access records for purposes of verifying diagnoses listed in the discharge records. Without a clear, measurable, and specific definition of an illness, consumers of reports are unable to interpret, compare, and aggregate data from various studies Citation22. An example of the distortion that can arise from the use of different case definitions was the ‘surge’ in AIDS cases that arose after the Centers for Disease Control and Prevention (CDC) expanded their case definition for AIDS in 1993 Citation60. The WHO has established case definitions for the most common illnesses such as anemia Citation35, pneumonia Citation61, stroke Citation62, and diabetes mellitus Citation63. While it might be argued that some of the case definitions did not exist at the time when the earlier studies were conducted, only one of the more recent studies reviewed reported the use of case definitions Citation33. Obviously, improving the diagnostic capabilities of facilities would permit the use of more sophisticated and differentiating case definitions that rely upon test results.
The failure of two-thirds of the studies reviewed to use standard ICD coding systems also limits our capacity to compare studies or aggregate data. Stroke, for example, was classified as a neurological disorder in some studies while other studies classified it as a cardiovascular disorder in concordance with the ICD coding system. Diarrhea was listed as a digestive system illness in some studies while in others it was classified as an infectious and parasitic disease.
In many countries in sSA diagnostic facilities can only be found in large referral hospitals located in urban areas Citation64. Our analysis found that most of the studies describing medical illnesses in adults had been conducted in university teaching hospitals and referral facilities located in urban areas. These were also the facilities most likely to be operated by consultants Citation65 who, by virtue of their more advanced training, are more likely to publish research findings, potentially biasing the sample of reports available for this review. At the time that they were published, most of the population of sSA was living in rural areas with limited access to tertiary referral hospitals thus limiting the generalizability of the findings Citation20. As the pace of urbanization on the continent increases Citation66, studies conducted in urban hospitals are likely to be more representative than in the past.
The demographic transition that is driving this urbanization, with its associated increase in endemic non-communicable diseases, argues for substantial improvements in the diagnostic and curative services in adult health in sSA to enable the correct classification of disease and early initiation of control measures, especially for cardiovascular and other non-communicable chronic illnesses Citation67. Initiatives such as the WHO-supported Health Metrics Network Citation68 that aim to improve the collection of health-related data in developing countries by providing guidelines and templates need to appreciate that the quality of clinical data from hospitals in sSA will compromise the utility of these systems unless there is substantial investment in instruments and training. Adult demographic surveillance networks, such as the INDEPTH Citation69 network, could also provide adult morbidity data by linking the data from dedicated hospital surveillance teams to their population registers. Ultimately, well-conducted cohort studies will be needed, where the outcomes (and exposure variables) are compliant with international standards of disease detection and classification, in order to identify risk factors for important illnesses in sSA Citation70.
Our review had two principal limitations. Many articles publishing findings on research in Africa are not available through the Internet Citation71. Organizations such as AJOL (www.ajol.info) and HINARI (http://www.who.int/hinari/en/) have succeeded in providing substantial access to publications from Africa online. However, many publications are not available online and we were obliged to access print copies of 20 papers from the British Library and could not find a suitable source for a further six papers. Despite good electronic database we found 20% of the relevant papers through hand rather than online searching. Our exclusion of papers written in languages other than English, which were even more difficult to obtain, also potentially biased our results in favor of English-speaking countries. Despite these shortcomings we believe that the studies reviewed here are a fair representation of the research articles that have been published on the subject in the past six decades.
For some disease categories, such as neoplasms, we found extremely sparse data, which we attribute to the lack of appropriate diagnostic facilities rather than to insignificant numbers of patients with these diseases. We also observed an uneven contribution from different regions of the continent to the data through the different time periods studied, most likely due to variations in the availability of health-reporting infrastructure as a result of political or economic instability.
Conclusions and recommendations for the conduct of future studies
We found that there were very limited data on the causes of hospital admissions and death among adults in sSA, and these data had significant limitations. However, the review provides evidence to suggest that cardiovascular diseases account for a significant and increasing fraction of the causes of hospitalization among adults in sSA. As the epidemiology of adult disease in sSA transitions from infectious to non-communicable diseases, health researchers and policy makers will need to establish reliable and consistent systems for diagnosing and recording disease in adults in order to optimize treatments and preventive interventions.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
Acknowledgements
We would like to acknowledge Alex Maina of the KEMRI Wellcome Trust Research Programme, Kenya; Marie Meaden of the Nuffield Department of Clinical Medicine, University of Oxford, UK; and the British Library for providing articles not available online. We would like to thank Dr. Susan Morpeth and Dr. Andrew Brent for helpful suggestions on earlier versions of the manuscript. Dr. Etyang is funded by a grant from the PneumoADIP of Johns Hopkins School of Public Health. Dr. Scott is funded by a Wellcome Trust Fellowship (No. 081835). This paper is published with the permission of the Director, KEMRI, Kilifi.
References
- Phillips M, Feachem RG, Murray CJ, Over M, Kjellstrom T. Adult health: a legitimate concern for developing countries. Am J Public Health. 1993; 83: 1527–30. Available from: http://www.ncbi.nlm.nih.gov/pubmed/823867110.3402/gha.v6i0.19090.
- Jamison DT, Feachem RG, Malegapuru WM, Bos ER, Baingana FK, et al.. Disease and mortality in sub-Saharan Africa. Washington DC: World Bank. 2006.
- World Bank. World development report 1993 – investing in health. Washington DC: World Bank. Available from: http//:files.dcp2.org/pdf/WorldDevelopmentReport1993.pdf [cited 5 June 2011].
- Rajaratnam JK, Marcus JR, Flaxman AD, Wang H, Levin-rector A, Dwyer L, et al.. Neonatal, postnatal, childhood, and under-5 mortality for 187 countries, 1970–2010: a systematic analysis of progress towards millennium development goal 4. Lancet. 2010; 375: 1988–2008. DOI: 10.3402/gha.v6i0.19090.
- You D, Jones G, Hill K, Wardlaw T, Chopra M. Levels and trends in child mortality, 1990–2009. Lancet. 2010; 376: 931–3. DOI: 10.3402/gha.v6i0.19090.
- United Nations Department of Economic and Social Affairs. World population prospects: the 2008 revision. Geneva: United Nations. 2009. Available from: http://www.un.org/esa/population/publications/popnews/Newsltr_87.pdf [cited 5 June 2011].
- UNAIDS, WHO, UNICEF (2004). Children on the brink 2004: a joint report on orphan estimates and program strategies. Washington DC: USAID. Available from: data.unaids.org/publications/…/unicef_childrenonthebrink2004_en.pdf [cited 10 June 2011].
- Kitange HM, Machibya H, Black J, Mtasiwa DM, Masuki G, Whiting D, et al.. Outlook for survivors of childhood in sub-Saharan Africa: adult mortality in Tanzania. Adult morbidity and mortality project. BMJ. 1996; 312: 216–20. Available from http://www.ncbi.nlm.nih.gov/pubmed/8563587.
- Mathers CD, Fat DM, Inoue M, Rao C, Lopez AD. Counting the dead and what they died from: an assessment of the global status of cause of death data. Bull World Health Organ. 2005; 83: 171–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15798840.
- Rajaratnam JK, Marcus JR, Levin-rector A, Chalupka AN, Wang H, Dwyer L, et al.. Worldwide mortality in men and women aged 15–59 years from 1970 to 2010: a systematic analysis. Lancet. 2010; 375: 1704–20. DOI: 10.3402/gha.v6i0.19090.
- Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006; 367: 1747–57. DOI: 10.3402/gha.v6i0.19090.
- Koyanagi A, Shibuya K. What do we really know about adult mortality worldwide?. Lancet. 2010; 375: 1668–70. DOI: 10.3402/gha.v6i0.19090.
- Cooper RS, Osotimehin B, Kaufman JS, Forrester T. Disease burden in sub-Saharan Africa: what should we conclude in the absence of data?. Lancet. 1998; 351: 208–10. DOI: 10.3402/gha.v6i0.19090.
- WHO. Global status report on noncommunicable diseases. : Geneva: World Health Organization. 2010. Available from: http://www.who.int/nmh/publications/ncd_report2010/en/ [cited 8 June 2011].
- Maher D, Smeeth L, Sekajugo J. Health transition in Africa: practical policy proposals for primary care. Bull World Health Organ. 2010; 88: 943–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/2112472010.3402/gha.v6i0.19090.
- Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, Asaria P, et al.. Priority actions for the non-communicable disease crisis. Lancet. 2011; 377: 1438–47. DOI: 10.3402/gha.v6i0.19090.
- Law T, Lavis J, Hamandi A, Cheung A, El-Jardali F. Climate for evidence-informed health systems: a profile of systematic review production in 41 low-and middle-income countries, 1996–2008. J Health Res Policy. 2012; 17: 4–10. Available from: http://www.ncbi.nlm.nih.gov/pubmed/2196782310.3402/gha.v6i0.19090.
- Beaglehole R, Horton R. Chronic diseases: global action must match global evidence. Lancet. 2010; 376: 1619–21. DOI: 10.3402/gha.v6i0.19090.
- Moisi JC, Nokes DJ, Gatakaa H, Williams TN, Bauni E, Levine OS, et al.. Sensitivity of hospital-based surveillance for severe disease: a geographic information system analysis of access to care in Kilifi district, Kenya. Bull World Health Organ. 2011; 89: 102–11. Available from: http://www.ncbi.nlm.nih.gov/pubmed/2134692110.3402/gha.v6i0.19090.
- Arcury TA, Gesler WM, Preisser JS, Sherman J, Spencer J, Perin J. The effects of geography and spatial behavior on health care utilization among the residents of a rural region. Health Serv Res. 2005; 40: 135–56. Available from: http://www.ncbi.nlm.nih.gov/pubmed/2134692110.3402/gha.v6i0.19090.
- WHO. International statistical classification of diseases and health related problems. Geneva: World Health Organization. 2004. Available from: http://apps.who.int/classifications/apps/icd/icd10online/ [cited 16 June 2011].
- Grimes DA, Schulz KF. Descriptive studies: what they can and cannot do. Lancet. 2002; 359: 145–9. DOI: 10.3402/gha.v6i0.19090.
- Hennekens C, Buring J. Epidemiology in medicine. Little Brown and Company. Boston MA, 1987
- Vandenbroucke JP, von Elm E, Altman DG, Gotzsche PC, Mulrow CD, Stuart J, et al.. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLoS Medicine. 2007; 4: e297. Available from: http://www.plosmedicine.org/article/info%3Adoi%2F10.1371%2Fjournal.pmed.004029710.3402/gha.v6i0.19090.
- Lester FT. The Pattern of adult medical admissions in Addis Ababa, Ethiopia. East Afr Med J. 1976; 53: 620–34. Available from: http://www.ncbi.nlm.nih.gov/pubmed/1017396.
- Amsel M, Matewos A. The changing pattern of diseases in the mid 1990's: experience of a teaching hospital in North Western Ethiopia. Ethiop J Health Dev. 1999; 13: 1–7.
- Barr RD. A two-year prospective analysis of emergency admissions to an adult medical unit at the Kenyatta National Hospital, Nairobi. East Afr Med J. 1972; 49: 772–82. Available from: http://www.ncbi.nlm.nih.gov/pubmed/4666003.
- Brown KGE. Analysis of admissions to the adult medical wards at Queen Elizabeth Central Hospital, Blantyre, Malawi. East Afr Med J. 1975; 52: 509–28. Available from: http://www.ncbi.nlm.nih.gov/pubmed/1192992.
- Edginton ME, Hodkinson J, Seftel HC. Disease patterns in a South African rural Bantu population, including a commentary on comparisons with the pattern in urbanized Johannesburg Bantu. S Afr Med J. 1972; 46: 968–76. Available from: http://www.ncbi.nlm.nih.gov/pubmed/5066429.
- Patel KM, Lwanga SK. A study of medical admissions to Mulago Hospital, Kampala. East Afr Med J. 1971; 48: 76–84. Available from: http://www.ncbi.nlm.nih.gov/pubmed/5088515.
- Turner PP. The pattern of disease as seen by medical admissions to the Coast Province General Hospital in 1960. East Afr Med J. 1962; 39: 121–135. Available from: http://www.ncbi.nlm.nih.gov/pubmed/13923226.
- Williams E, Hayes R, Smith P. Admissions to a rural hospital in the West Nile District of Uganda over a 27-year period. J Trop Med Hyg. 1986; 89: 193–211. Available from: http://www.ncbi.nlm.nih.gov/pubmed/3783813.
- Huerga H, Vasset B, Prados E. Adult and paediatric mortality patterns in a referral hospital in Liberia 1 year after the end of the war. Trans R Soc Trop Med Hyg. 2009; 103: 476–84. Available from: http://www.ncbi.nlm.nih.gov/pubmed/1924380310.3402/gha.v6i0.19090.
- Kakembo A, Walker B, Walker A. Causes of admission of African patients to Gelukspan Hospital. East Afr Med J. 1996; 73: 746–51. Available from: http://www.ncbi.nlm.nih.gov/8997867.
- McLean E, Cogswell M, Egli I, Wojdyla D, de Benoist B. Worldwide prevalence of anaemia. WHO vitamin and mineral nutrition information system, 1993–2005. Public Health Nutr. 2009; 12: 444–54. Available from: http://www.ncbi.nlm.nih.gov/pubmed/1849867610.3402/gha.v6i0.19090.
- Adekunle O, Olatunde I, Abdullateef R. Causes and pattern of death in a tertiary health institution in south western Nigeria. Niger Postgrad Med J. 2008; 15: 247–50. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19169342.
- Dean MP, Gear JS. Medical admissions to Hillbrow Hospital, Johannesburg, by discharge diagnosis. S Afr Med J. 1986; 69: 672–3. Available from: http://www.ncbi.nlm.nih.gov/pubmed/3704853.
- Marszalek J,, De Villiers PJT. Morbidity profile of admissions to GF Jooste Hospital, Manenberg, Cape Town. S A Fam Pract. 2006; 48: 15.
- Mudiayi TK, Onyanga-Omara A, Gelman ML. Trends of morbidity in general medicine at United Bulawayo Hospitals, Bulawayo, Zimbabwe. Cent Afri J Med. 1997; 43: 213–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9431757.
- Walker ARP, Walker BF, Dunn MJ, Dunn SE. Causes of admissions of rural African patients to Murchison Hospital, Natal, South Africa. J R Soc Health. 1994; 114: 33–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/816424310.3402/gha.v6i0.19090.
- Pavlica D. Analysis of medical admissions to the Armed Forces Hospital in Addis Ababa from January 1966 to January 1970. Ethiop Med J. 1970; 8: 193–200. Available from: http://www.ncbi.nlm.nih.gov/pubmed/5522102.
- Adetuyibi A, Akisanya JB, Onadeko BO. Analysis of the causes of death on the medical wards of the University College Hospital, Ibadan over a 14-year period (1960–1973). Trans R Soc Trop Med Hyg. 1976; 70: 466–73. Available from: http://www.ncbi.nlm.nih.gov/pubmed/84165010.3402/gha.v6i0.19090.
- Shaper AG, Shaper L. Analysis of medical admissions to Mulago Hospital, 1957. East Afr Med J. 1958; 35: 647–77. Available from: http://www.ncbi.nlm.nih.gov/pubmed/13630217.
- Griffiths ML. A comparison of admissions to a semirural hospital between the years 1959/1960 and 1977/1978. S Afr Med J. 1981; 59: 983–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/7244910.
- Ndjeka N, Ogunbanjo G. Disease patterns in the medical wards of a rural South African hospital. SA Fam Pract. 2004; 45: 10–1.
- Reeve PA, Falkner MJ. Disease patterns in a rural black population. S Afr Med J. 1986; 69: 551–2. Available from: http://www.ncbi.nlm.nih.gov/pubmed/3704872.
- Akoria O, Unuigbe E. A 6-month review of medical admissions in a Nigerian teaching hospital. Int J Health Res. 2010; 2: 123–30.10.3402/gha.v6i0.19090.
- Ike S. The pattern of admissions into the medical wards of the University of Nigeria Teaching Hospital, Enugu (2). Niger J Clin Pract. 2008; 11: 185–92. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19140351.
- Pobee JO. A review of the causes of death in adult medical wards of Korle Bu Teaching Hospital, Accra, Ghana. Afr J Med Sci. 1976: 79–85. Available from: http://www.ncbi.nlm.nih.gov/pubmed/829710.
- WHO. Working together for health; the world health report 2006. Geneva: World Health Organization. 2006. Available from: http://www.who.int/whr/2006/en/ [cited 5 July 2011].
- Kigozi IM, Dobkin LM, Martin JN, Geng EH, Muyindike W, Emenyonu NI, et al.. Late-disease stage at presentation to an HIV clinic in the era of free antiretroviral therapy in Sub-Saharan Africa. J Acquir Immune Defic Syndr. 2009; 52: 280–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/1952124810.3402/gha.v6i0.19090.
- Barbarinia G, Barbaro G. Incidence of the involvement of the cardiovascular system in HIV infection. AIDS. 2003; 17: S46–50. Available from: http://www.ncbi.nlm.nih.gov/pubmed/1287053010.3402/gha.v6i0.19090.
- Kesselring A, Gras L, Smit C, van Twillert G, Verbon A, de Wolf F, et al.. Immunodeficiency as a risk factor for non-AIDS-defining malignancies in HIV-1-infected patients receiving combination antiretroviral therapy. Clin Infect Dis. 2011; 52: 1458–65. Available from: http://www.ncbi.nlm.nih.gov/pubmed/2162848810.3402/gha.v6i0.19090.
- Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005; 365: 217–23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15652604.
- Mbanya JC, Motala AA, Sobongwi E, Assah FK, Enoru ST. Diabetes in sub-Saharan Africa. Lancet. 2010; 375: 2254–66. Available from: http://www.ncbi.nlm.nih.gov/pubmed/2060997110.3402/gha.v6i0.19090.
- Tollman SM, Kahn K, Sartorius B, Collinson MA, Clark SJ, Garenne ML. Implications of mortality transition for primary health care in rural South Africa: a population-based surveillance study. Lancet. 2008; 372: 893–901. Available from: http://www.ncbi.nlm.nih.gov/pubmed/1879031210.3402/gha.v6i0.19090.
- Byass P. The imperfect world of global health estimates. PLoS Medicine. 2010; 7: e1001006.10.3402/gha.v6i0.19090.
- Perel P, Miranda JJ, Ortiz Z, Casas JP. Relation between the global burden of disease and randomized clinical trials conducted in Latin America published in the five leading medical journals. PLoS ONE. 2008; 3: e1696. Available from: http://www.ncbi.nlm.nih.gov/pubmed/1830177210.3402/gha.v6i0.19090.
- Sridhar D, Batniji R. Misfinancing global health: a case for transparency in disbursements and decision making. Lancet. 2008; 372: 1185–91. DOI: 10.3402/gha.v6i0.19090.
- Anonymous. Impact of the expanded AIDS surveillance case definition on AIDS case reporting – United States, first quarter, 1993. MMWR Morb Mortal Wkly. 1993; 42: 308–10. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8474424.
- International Working Group. Integrated management of adolescent and adult illness (IMAI). Geneva: World Health Organization. 2002. Available from: http://www.who.int/hiv/pub/imai/en/index.html [cited 12 July 2011].
- Hatano S. Experience from a multicenter stroke register: a preliminary report. Bull World Health Organ. 1976; 54: 541–53. Available from: http://www.ncbi.nlm.nih.gov/pubmed/1088404.
- World Health Organization (2006). Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia: a report of a WHO/IDF consultation. Geneva: World Health Organization. Available from: http://whqlibdoc.who.int/publications/2006/9241594934_eng.pdf [cited 12 July 2011]..
- Adeyi OA. Pathology Services in developing countries: the west African experience. Arch Pathol Lab Med. 2011; 135: 183–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21284434.
- Lemiere C, Herbst CH, Jahanshahi N, Smith E. Reducing geographical imbalances of health workers in Sub-Saharan Africa: a labor market perspective on what works, what does not, and why. Washington DC: World Bank. 2011. Available from: http://www-wds.worldbank.org/external/default/WDSContentServer/WDSP/IB/2011/01/07/000333038_20110107020314/Rendered/PDF/588430NWP0Heal101public10BOX353816B.pdf [cited 22 July 2011].
- UN Habitat. State of the world's cities: trends in sub-Saharan Africa. Nairobi: United Nations Human Settlements Program. 2004. Available from http://ww2.unhabitat.org/mediacentre/sowckit.asp [cited 22 July 2011].
- Damasceno A, Cotter G, Dzudie A, Sliwa K, Mayosi BM. Heart failure in sub-Saharan Africa: time for action. J Am Coll Cardiol. 2007; 50: 1688–93. Available from: http://www.ncbi.nlm.nih.gov/pubmed/1795015210.3402/gha.v6i0.19090.
- WHO/Health Metrics Network. Framework and standards for country health information systems. 2nd ed. Geneva: World Health Organization. 2008. Available from: http://www.who.int/healthmetrics/documents/hmn_framework200803.pdf [cited 12 July 2011].
- Kowal P, Kahn K, Ng N, Naidoo N, Abdullah S, Bawah A, et al.. Ageing and adult health status in eight lower-income countries: the INDEPTH WHO-SAGE collaboration. Glob Health Action. 2011; 3: 11–22. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20959878.
- Holmes MD, Dalal S, Volmink J, Adebamowo CA, Njelekela M, Fawzi F, et al.. Non-communicable diseases in Sub-Saharan Africa: the case for cohort studies. PLoS Medicine. 2010; 7: e1000244. Available from: http://www.ncbi.nlm.nih.gov/pubmed/2048548910.3402/gha.v6i0.19090.
- Pakenham-Walsh N, Priestley C. Towards equity in global health knowledge. QJM. 2002; 95: 469–73. Available from: http://www.ncbi.nlm.nih.gov/pubmed/1209615210.3402/gha.v6i0.19090.
- Reyburn H, Mbatia R, Drakeley C, Carneiro I, Mwakasungula E, Mwerinde O, et al.. Overdiagnosis of malaria in patients with severe febrile illness in Tanzania: a prospective study. BMJ. 2004; 329: 1212. Available from: http://www.ncbi.nlm.nih.gov/pubmed/1554253410.3402/gha.v6i0.19090.
- WHO. Manual of the international statistical classification of diseases, injuries, and causes of death. Bull World Health Org. 1953; 7: 1–55. Available from: http://www.ncbi.nlm.nih.gov/pubmed/13032790.
- Mullan F, Frehywot S, Omaswa F, Buch E, Chen C, Greysen SR, et al.. Medical schools in sub-Saharan Africa. Lancet. 2010; 6736: 1–9. DOI: 10.3402/gha.v6i0.19090.
- Rich EC, Gifford G, Luxenberg M, Dowd B. The relationship of house staff experience to the cost and quality of inpatient care. JAMA. 1990; 263: 953–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/229976210.3402/gha.v6i0.19090.
- Mullan F, Frehywot S. Non-physician clinicians in 47 sub-Saharan African countries. Lancet. 2007; 370: 2158–63. DOI: 10.3402/gha.v6i0.19090.
- Agomuoh DI, Unachukwu CN. Pattern of diseases among medical admissions in Port Harcourt, Nigeria. Niger Med Pract. 2008; 51: 45–50.
- Bardgett HP, Beeching NJ. Increase in hospital mortality from non-communicable disease and HIV-related conditions in Bulawayo, Zimbabwe, between 1992 and 2000. Trop Doct. 2006; 36: 129–31. Available from: http://www.ncbi.nlm.nih.gov/pubmed/1688461210.3402/gha.v6i0.19090.
- Gill GV. Changing patterns of medical disease in Soweto, South Africa 1981–1990. Trop Doct. 1995; 25: 171–2. Available from: http://www.ncbi.nlm.nih.gov/pubmed/7502326.
- Harries AD, Richard S, Wirima J. Medical admissions to Kamuzu Central Hospital, Lilongwe Malawi in 1986: comparison with admissions to Queen Elizabeth Central Hospital, Blantyre in 1973. Trop Geogr Med. 1990; 42: 274–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/2293437.
- Odenigbo C, Oguejiofor O. Pattern of medical admissions at the Federal Medical Centre, Asaba – a two year review. Niger J Clin Pract. 2009; 12: 395–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20329679.
- Osuafor TO, Ele PU. The pattern of admissions in the medical wards of Nnamdi Azikiwe University Teaching Hospital (NAUTH) Nnewi. Orient J Med. 2004; 16: 11–5.10.3402/gha.v6i0.19090.
- Tambwe M, Mbala M, Lusamba DN, M'buyamba-Kabangu JR. Morbidity and mortality in hospitalised Zairean adults. S Afr Med J. 1995; 85: 74. Available from: http://www.ncbi.nlm.nih.gov/pubmed/7597537.