Abstract
Background
Studies from sub-Saharan Africa have shown high incidence of attrition due to mortality or loss to follow-up (LTFU) after initiating antiretroviral therapy (ART). India is the third largest country in the world in terms of HIV infected people, but predictors of attrition after ART initiation are not well known.
Design
We describe factors associated with attrition, mortality, and LTFU in 3,159 HIV infected patients who initiated ART between 1 January 2007 and 4 November 2011 in an HIV cohort study in India. The study included 6,852 person-years with a mean follow-up of 2.17 years.
Results
After 5 years of follow-up, the estimated cumulative incidence of attrition was 37.7%. There was no significant difference between attrition due to mortality and attrition due to LTFU. Having CD4 counts <100 cells/µl and being homeless [adjusted hazard ratio (aHR) 3.1, 95% confidence interval (CI) 2.6–3.8] were associated with a higher risk of attrition, and female gender (aHR 0.64, 95% CI 0.6–0.8) was associated with a reduced risk of attrition. Living near a town (aHR 0.82, 95% CI 0.7–0.999) was associated with a reduced risk of mortality. Being single (aHR 1.6, 95% CI 1.2–2.3), illiteracy (aHR 1.3, 95% CI 1.1–1.6), and age <25 years (aHR 1.3, 95% CI 1–1.8) were associated with an increased risk of LTFU. Although the cumulative incidence of attrition in patients diagnosed with tuberculosis after ART initiation was 47.4%, patients who started anti-tuberculous treatment before ART had similar attrition to patients without tuberculosis (36 vs. 35.2%, P=0.19) after four years of follow-up.
Conclusions
In this cohort study, the attrition was similar to the one found in sub-Saharan Africa. Earlier initiation of ART, improving the diagnosis of tuberculosis before initiating ART, and giving more support to those patients at higher risk of attrition could potentially reduce the mortality and LTFU after ART initiation.
By the end of 2011, 8 million people had started antiretroviral therapy (ART) worldwide (Citation1). The roll out of ART has added 15 million life-years in low- and middle-income countries, and it is estimated that it can reduce the HIV incidence by 17–32% (Citation1, Citation2).
With 2.1 million people living with HIV (Citation3), India has the third largest burden of HIV worldwide. The HIV epidemic in India has been considered concentrated in high-risk groups (female sex workers, men who have sex with men, transgender, and injecting drug users) who transmit the virus to the general population through a bridge population (male migrants and truckers). Targeted interventions in these groups have achieved a dramatic 57% reduction in the incidence of HIV, according to governmental data (Citation3). However, some epidemiological studies suggest a more generalised distribution of HIV in the population (Citation4–Citation7)
By December 2012, 1.7 million people living with HIV had been registered in Government ART centres, of whom 604,987 had started ART under the national programme (Citation8). Studies from sub-Saharan Africa had shown that the cumulative incidence of attrition after 3 years of follow-up can be up to 35% (Citation9). However research studies investigating predictors of mortality or loss to follow up (LTFU) after ART initiation are scarce in India (Citation10). A better understanding of the risk factors associated with attrition in India could be helpful to design interventions to reduce mortality and LTFU in patients who initiate ART. The aim of this study is to describe the attrition after ART initiation in a large cohort of patients in Anantapur, India.
Methods
Setting
The study was performed in Anantapur, a district situated in the State of Andhra Pradesh, India. In Anantapur, 72% of the population live in rural areas (Citation11), and there is >1% prevalence of HIV infection in antenatal clinics (Citation12). The HIV epidemic in Anantapur is largely driven by heterosexual transmission, and it is characterised by poor socio-economic conditions and high levels of illiteracy (Citation6). Rural Development Trust (RDT) is a non-governmental organisation that provides medical care to HIV infected people free of charge, including medicines, consultations, or hospital admission charges. In Bathalapalli RDT Hospital, CD4 count enumeration and ART are provided free of charge by the Indian Government under a public–private partnership. During the study period, ART was also provided by another ART centre in the district (Anantapur ART centre), and ART was initiated according to the Indian National Guidelines (Citation13–Citation15), so the CD4 cell count threshold for initiating ART was 250 cells/µl.
Study design
The Vicente Ferrer HIV Cohort Study is an open cohort study of all HIV infected patients who have attended RDT hospitals since June 2006. Routine clinical data from patients were collected prospectively since September 2009, and retrospectively from June 2006 to September 2009. The characteristics of the cohort have been described in detail elsewhere (Citation6).
Study population
For this study, we selected HIV infected adults (>15 years) living in Anantapur who initiated ART between 1 January 2007 and 4 November 2011. Patients transferred to other ART centres after initiating ART were not included in the analysis. The selection of patients from the database was executed on 14 September 2012 (end of the study period).
Patients’ LTFU were routinely searched for by phone calls and home visits by a group of 31 outreach workers distributed throughout the district, and in those patients who had died, relatives were asked the date of death of the patients.
Definitions
Designation of the community of patients was performed by self-identification. Scheduled caste community is marginalised in the traditional Hindu caste hierarchy and, therefore, suffers social and economic exclusion and disadvantage (Citation16). Scheduled tribe community is generally geographically isolated with limited economic and social contact with the rest of the population (Citation16). Scheduled castes and scheduled tribes are considered socially disadvantaged communities and are supported by positive discrimination schemes operated by the Government of India (Citation17). Patients were considered as living near an ART centre if they lived in a mandal (administrative subdivision of districts in Andhra Pradesh; e.g. Anantapur district has 64 mandals) with an ART centre, or lived next to a mandal with an ART centre. Patients were considered as living near a town when they lived in a mandal containing a town with a population >100,000 people. Towns have better communications than rural areas. Poverty was defined as living with less than 1,000 Indian rupees per month (approximately US$18 as of May 2013). Illiteracy was defined as not being able to read or write.
Ethics statement
The study was approved by the Ethical Committee of the Rural Development Trust Hospital. Written informed consent was given by patients or caretakers for their information to be stored in the study database and used for research.
Statistical analysis
Statistical analysis was performed using Stata Statistical Software (Stata Corporation. Release 11. College Station, TX, USA). To investigate predictors of attrition, time-to-event methods were used. Time was measured from ART initiation to death. Patients who did not die during the study period were censored at their last visit to the clinics. Patients who did not come to the clinics for at least 180 days after their last scheduled appointment were considered LTFU (Citation18). Attrition, mortality, and LTFU rates were calculated by summing the number of patients who experienced the event (attrition, death, or LTFU) during a particular period of time divided by the total number of years of follow-up during this period. Multivariable analysis was performed by Cox regression proportional hazard models. The proportional hazard assumption was assessed performing log–log survival curves based on Schoenfeld residuals (Citation19). Missing values were imputed using multiple imputations by chained equation assuming missing at random (Citation20). The variables that were imputed were poverty (33 missing values), homelessness (46 missing values), illiteracy (4 missing values), and marital status (6 missing values). We used Kaplan–Meier survival estimates to calculate cumulative incidences of attrition. Cumulative incidences of mortality and LTFU were calculated using competing risk analysis (stcompet command in Stata) (Citation21).
Results
We identified 3,159 patients who initiated ART. Baseline characteristics of the patients and rates of attrition, mortality, and LTFU are described in . Forty-one percent of patients were women, two thirds were married, and the median age was 33.8 years [interquartile range (IQR) 28–40). One fourth belonged to socially disadvantaged communities, more than half were illiterate, 7% were homeless, and more than one third had a monthly income <1,000 Indian rupees. One third of patients were living near an ART centre, and 44% were living near a town. The median CD4 cell count was 140 cells/µl (IQR 84–195). Thirteen percent were diagnosed with tuberculosis within 3 months before ART initiation, and 7.5% within 3 months after ART initiation.
Table 1 Baseline characteristics and rates of attrition, mortality, and loss to follow up of patients initiating antiretroviral therapy
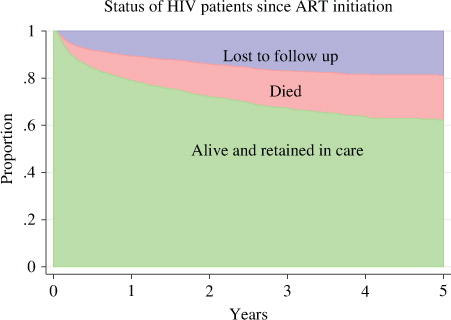
The study included 6,852 person-years (PY) with a mean follow-up of 2.17 years (standard deviation 1.5); 478 (15.1%) patients died, and 489 (15.5%) were LTFU. The overall attrition rate was 14.1 per 100 PY, the mortality rate was 7 per 100 PY, and the LTFU rate was 7.1 per 100 PY. The median time to death was 0.52 years (IQR, 0.18–1.3), and the median time to be LTFU was 0.45 years (0.16–1.38). presents a stacked graph of the status of HIV patients since ART initiation. The attrition rate after ART initiation was 34.8 per 100 PY during the first semester (0–6 months), 12.9 per 100 PY during the second semester (6–12 months), 9.1 per 100 PY during the second year (12–24 months), 6.9 per 100 PY during the third year (24–36 months), 5.8 per 100 PY during the fourth year (36–48 months), and 2.4 per 100 PY during the fifth year (48–60 months). The cumulative incidence of attrition, mortality, and LTFU after 6 months, 1 year, 2 years, 3 years, 4 years, and 5 years of follow-up is presented in . The estimated cumulative incidence of attrition for any reason was 37.7% [95% confidence interval (CI) 35.5–40] at 5 years.
Table 2 Cumulative incidence and 95% confidence interval of attrition (mortality or loss to follow up), mortality, and loss to follow up at 0.5, 1, 2, 3, 4, and 5 years after antiretroviral therapy initiation
presents the cumulative incidence of attrition, mortality, and LTFU stratified by CD4 cell counts. The cumulative incidence curve of mortality was not statistically different from the cumulative incidence curve of LTFU (log–rank test P =0.65) (A). The mortality rate after ART initiation was 16.7 per 100 PY during the first semester, 7 per 100 PY during the second semester, 4.5 per 100 PY during the second year, 3 per 100 PY during the third year, 3.4 per 100 PY during the fourth year, and 1.7 per 100 PY during the fifth year. The LTFU rate after ART initiation was 18.1 per 100 PY during the first semester, 5.9 per 100 PY during the second semester, 4.6 per 100 PY during the second year, 4 per 100 PY during the third year, 2.4 per 100 PY during the fourth year, and 0.7 per 100 PY during the fifth year.
Fig. 2 Cumulative incidence of (A) mortality and loss to follow up, (B) attrition by CD4 lymphocyte count, (C) mortality by CD4 lymphocyte count, and (D) loss to follow up by CD4 lymphocyte count.
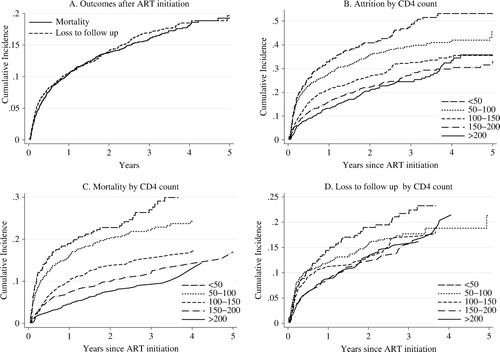
The cumulative incidence curves of attrition by CD4 cell counts showed three patterns of attrition: patients with CD4 counts <50 cells/µl, those with CD4 counts 50–100 cells/µl, and those with CD4 counts >100 cells/µl (B). Mortality was inversely proportional to the CD4 cell counts of the patients (C). Cumulative incidence curves of LTFU showed three patterns of attrition: patients with CD4 counts <50 cells/µl, those with CD4 counts 50–150 cells/µl, and those with CD4 counts >150 cells/µl (D). However, patients with CD4 counts >50 cells/µl had similar proportions of LTFU after 3 years of follow-up.
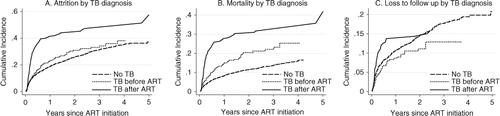
presents the cumulative incidence of attrition, mortality, and LTFU by the timing of tuberculosis diagnosis. Patients diagnosed with tuberculosis after ART initiation had higher incidence of attrition (47.4%) and mortality (31.6%) after 4 years of follow-up. This group also had a higher incidence of LTFU during the first 2 years of follow-up (C). Those patients diagnosed with tuberculosis before ART initiation had a similar incidence of attrition (36 vs. 35.2%, log–rank test P=0.19), higher incidence of mortality (23.2 vs. 16%, log–rank test P<0.001), and lower incidence of LTFU (12.9 vs. 19.3%, log–rank test P=0.045) than patients without tuberculosis after 4 years of follow-up.
Fig. 3 (A) Attrition, (B) mortality, and (C) loss to follow up by the timing of tuberculosis diagnosis. ART, antiretroviral therapy; TB, tuberculosis.
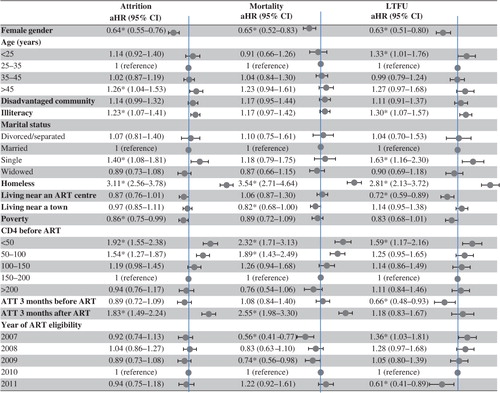
presents the Cox regression analysis of factors associated with attrition, mortality, and LTFU. Factors associated with attrition were being homeless [adjusted hazard ratio (aHR) 3.11, 95% CI 2.56–3.78); CD4 count <50 cells/µl (aHR 1.92, 95% CI 1.55–2.38); CD4 count 50–100 cells/µl (aHR 1.54, 95% CI 1.27–1.87); initiating anti-tuberculous treatment within 3 months after ART initiation (aHR 1.83, 95% CI 1.49–2.24); being single, age >45 years (aHR 1.26, 95% CI 1.04–1.53); and illiteracy (aHR 1.23, 95% CI 1.07–1.41). Female gender (aHR 0.64, 95% CI 0.55–0.76) and poverty (aHR 0.86, 95% CI 0.75–0.99) were factors associated with a lower risk of attrition. Factors associated with mortality were being homeless (aHR 3.54, 95% CI 2.71–4.64); CD4 count <50 cells/µl (aHR 2.32, 95% CI 1.71–3.13); CD4 count 50–100 cells/µl (aHR 1.89, 95% CI 1.43–2.49); and initiating anti-tuberculosis treatment within 3 months after ART initiation (aHR 2.55, 95% CI 1.98–3.3). Female gender (aHR 0.65, 95% CI 0.52–0.83) and living near a town (aHR 0.82, 95% CI 0.68–1) were factors associated with a lower risk of mortality. Factors associated with LTFU were being homeless (aHR 2.81, 95% CI 2.13–3.72); being single (aHR 1.63, 95% CI 1.16–2.3); CD4 count <50 cells/µl (aHR 1.59, 95% CI 1.17–2.16); age <25 years (aHR 1.33, 95% CI 1.01–1.76); and illiteracy (aHR 1.3, 95% CI 1.07–1.57). Female gender (aHR 0.63, 95% CI 0.51–0.8); initiating anti-tuberculous treatment within 3 months before ART initiation (aHR 0.66, 95% CI 0.48–0.93); and living near an ART centre (aHR 0.72, 95% CI 0.59–0.89) were factors associated with a lower risk of LTFU. Although an earlier calendar year of ART initiation was not associated with attrition after ART initiation, it was associated with an increased risk of LTFU and a reduced risk of death, suggesting that it was more difficult to document the mortality at earlier calendar years.
Fig. 4 Cox regression analysis of factors associated with attrition (mortality or loss to follow up), mortality, and loss to follow up.
*P value < 0.05. aHR, adjusted hazard ratio by Cox regression analysis; ART, antiretroviral therapy; ATT, anti-tuberculous treatment; CI, confidence interval; LTFU, loss to follow up.
Discussion
In this study, it was demonstrated that nearly 40% of patients who initiate ART die or are LTFU after 5 years of follow-up. This staggering figure is in line with other studies from sub-Saharan Africa (Citation9), and with a study performed in an urban setting in North India (Citation10), which found that 35 and 39% of patients had died or were LTFU after 3 years of follow-up, respectively. However, the attrition was higher than the ones reported in recent studies from China (24%), Thailand (19%), and South Africa (21–26%) (Citation22–Citation24). These findings highlight the urgent need to reduce the attrition after ART initiation of HIV infected patients in India.
Patients with CD4 counts <100 cells/µl were at higher risk of attrition. Starting ART at higher CD4 cell counts could have a major impact on reducing the mortality and LTFU after ART initiation. Current Indian guidelines have raised the CD4 cell count threshold for initiation of ART to 350 cells/µl (Citation25), and this threshold has been recently increased to 500 cells/µl by the World Health Organization (Citation26). However, in our setting, two thirds of patients are diagnosed with HIV when their CD4 counts are <350 cells/µl (Citation27). Increasing the CD4 cell count threshold for starting ART will not increase the CD4 cell count of patients at ART initiation unless this is accompanied by interventions to achieve earlier diagnosis of HIV and to improve the linkage between HIV-diagnosis and ART centres (Citation27, Citation28).
In this study, we describe socio-demographic factors associated with attrition in India, which can be used to design interventions aimed at giving extra support to groups of patients having a higher risk of attrition. Male gender, illiteracy, being homeless, and being >45 years old were factors associated with an increased risk of attrition. Patients who were <25 years old or single were more likely to be LTFU. Typically, HIV infected individuals who are found to be eligible for ART receive two or three sessions of ART preparedness counselling before initiating ART (Citation25). HIV programmes in India should take into consideration that these groups of patients at higher risk of attrition may need a more intensive counselling before initiating ART (Citation24).
In line with two South African studies (Citation22, Citation29), attrition was more common during the first year of follow-up. Studies from resource-limited settings have shown that the most common reasons given by patients to not come back to the clinics are financial and fear of harsh treatment by healthcare workers (Citation30, Citation31). Implementing strategies to provide social and economic support during the first year of ART could reduce the programme attrition because patients who were retained in care for 1 year were less likely to be LTFU (Citation32). Moreover, campaigns to educate healthcare providers about the benefits of using positive rather than negative reinforcement in patients who miss appointments to the clinics, and to reduce the stigma and discrimination in healthcare facilities could be beneficial (Citation31).
In accordance with a South African study (Citation22), factors associated with mortality were similar to factors associated with LTFU. However, differences between predictors of mortality and LTFU were also found. Being single or <25 years old was associated with an increased risk of LTFU, but not with an increased risk of mortality. People living far from a town had a higher risk of mortality, but did not have a higher risk of LTFU. The higher risk of death of people living in rural areas is probably related to poorer access to medical care in rural areas of India (Citation33). Patients living near an ART centre were less likely to be LTFU, which supports the current policy of decentralisation of ART centres of the Indian Government (Citation34).
Patients who initiated anti-tuberculous treatment after ART initiation had an increased risk of attrition. However, initiating anti-tuberculous treatment before ART was not associated with an increased risk of attrition and was associated with a reduced risk of LTFU in the multivariable analysis. The increased risk of death observed when initiating ART before anti-tuberculous treatment confirms previous findings from our cohort and other resource-limited settings (Citation35, Citation36). Although these results suggest that HIV patients living in areas with a high prevalence of tuberculosis should be thoroughly investigated for tuberculosis before ART initiation, current Indian guidelines do not have a protocol to rule out tuberculosis before starting ART (Citation25).
The study had some limitations. Patients LTFU may not be lost forever because they may reengage in the future or enrol in other ART centres. However, in a systematic review and meta-analysis of the mortality of patients LTFU in sub-Saharan Africa, it was estimated that the mortality of patients LTFU can be nearly 50% in programmes with a 20% rate of LTFU (Citation30). In a community tracking survey of patients LTFU in Ethiopia (Citation37), nearly half of patients LTFU died, most deaths occurred during the first 6 months of loss, and the mortality was particularly higher in those patients with lower CD4 cell counts or tuberculosis. The high mortality of patients LTFU may explain the similarities between the predictors of mortality and LTFU found in our study. Those variables related to LTFU, but not to mortality (i.e. younger age, being single, illiteracy, and not living near an ART centre), may be useful to identify patients with a lower risk of death among those LTFU.
Conclusions
The results of this cohort study indicate that the attrition after ART initiation is extremely high. Nearly 40% of patients die or are LTFU. Having low CD4 cell counts, being homeless, and male gender were found to be factors strongly associated with attrition. Although the mortality of patients diagnosed with tuberculosis after ART initiation was very high, patients who started anti-tuberculosis treatment before ART had similar attrition to patients without tuberculosis. The results of this study indicate that intervention aimed at increasing the CD4 cell count of patients at the time of ART initiation, improving the diagnosis of tuberculosis before starting ART, and giving extra support to the groups of patients at higher risk of attrition could potentially reduce the mortality and LTFU of HIV programmes in India.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
References
- UNAIDS. UNAIDS report on the global AIDS epidemic. 2012. Available from: http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2012/gr2012/20121120_UNAIDS_Global_Report_2012_en.pdf [cited 5 Dec 2012].
- Eaton JW , Johnson LF , Salomon JA , Bärnighausen T , Bendavid E , Bershteyn A , etal. HIV treatment as prevention: systematic comparison of mathematical models of the potential impact of antiretroviral therapy on HIV incidence in South Africa. PLoS Med. 2012; 9: e1001245.
- National AIDS Control Organisation, India. HIV estimates 2012. Technical Report. 2013. Available from: www.nacoonline.org/upload/Surveillance/Reports%20&%20Publication/Technical%20Report%20-%20India%20HIV%20Estimates%202012.pdf [cited 22 Jul 2013].
- Dandona L , Lakshmi V , Sudha T , Kumar GA , Dandona R . A population-based study of human immunodeficiency virus in south India reveals major differences from sentinel surveillance-based estimates. BMC Med. 2006; 4: 31.
- Perkins JM , Khan KT , Subramanian SV . Patterns and distribution of HIV among adult men and women in India. PLoS One. 2009; 4: e5648.
- Alvarez-Uria G , Midde M , Pakam R , Naik PK . Gender differences, routes of transmission, socio-demographic characteristics and prevalence of HIV related infections of adults and children in an HIV cohort from a rural district of India. Infect Dis Rep. 2012; 4: e19.
- Alvarez-Uria G , Midde M , Naik PK . Trends and risk factors for HIV infection among young pregnant women in rural India. Int J Infect Dis. 2012; 16: e121–3.
- National AIDS Control Organisation. Annual Report 2012–13. 2013. Available from: http://www.nacoonline.org/upload/Publication/Annual%20Report/Annual%20report%202012-13_English.pdf [cited 22 Jul 2013].
- Fox MP , Rosen S . Patient retention in antiretroviral therapy programs up to three years on treatment in sub-Saharan Africa, 2007–2009: systematic review. Trop Med Int Health. 2010; 15(Suppl 1): 1–15.
- Sharma SK , Dhooria S , Prasad K , George N , Ranjan S , Gupta D , etal. Outcomes of antiretroviral therapy in a northern Indian urban clinic. Bull World Health Organ. 2010; 88: 222–6.
- Census of India. 2011; India: Office of the Registrar General & Census Commissioner.
- National AIDS Control Organisation. HIV sentinel surveillance 2010–11. A Technical Brief. 2012. Available from: http://naco.gov.in/upload/Surveillance/Reports%20&%20Publication/HSS%202010-11_Technical%20Brief_30%20Nov%2012.pdf [cited 21 Jan 2013].
- National AIDS Control Organisation. Ministry of Health & Family Welfare Government of India. Antiretroviral therapy guidelines for HIV infected adults and adolescents including post-exposure. 2007. Available from: http://www.nacoonline.org/About_NACO/Policy__Guidelines/Policies__Guidelines_Table_for_download/ [cited 1 Sep 2011].
- Panos. Antiretroviral drugs for all? Obstacles in accessing treatment lessons from India. 2007. Available from: http://www.panossouthasia.org/pdf/Antiretrovirals.pdf [cited 27 May 2012].
- WHO. Antiretroviral therapy for HIV infection in adults and adolescents. 2006. Available from: http://www.who.int/hiv/pub/guidelines/artadultguidelines.pdf [cited 27 May 2012].
- Gang IN , Sen K , Yun MS . Caste, ethnicity, and poverty in rural India. IZA Bonn, Germany. 2002
- Alvarez-Uria G , Midde M , Naik PK . Socio-demographic risk factors associated with HIV infection in patients seeking medical advice in a rural hospital of India. J Public health Res. 2012; 1: e14.
- Chi BH , Yiannoutsos CT , Westfall AO , Newman JE , Zhou J , Cesar C , etal. Universal definition of loss to follow-up in HIV treatment programs: a statistical analysis of 111 facilities in Africa, Asia, and Latin America. PLoS Med. 2011; 8: e1001111.
- Kleinbaum DG , Klein M . Survival analysis, a self-learning text. Second. 2005; USA: New York.
- Royston P . Multiple imputation of missing values: further update of ice, with an emphasis on categorical variables. Stata J. 2009; 9: 466–77.
- Coviello V , Boggess M . Cumulative incidence estimation in the presence of competing risks. Stata J. 2004; 4: 103–12.
- Fatti G , Meintjes G , Shea J , Eley B , Grimwood A . Improved survival and antiretroviral treatment outcomes in adults receiving community-based adherence support: 5-year results from a multicentre cohort study in South Africa. J Acquir Immune Defic Syndr. 2012; 61: e50–8.
- Fregonese F , Collins IJ , Jourdain G , Lecoeur S , Cressey TR , Ngo-Giang-Houng N , etal. Predictors of 5-year mortality in HIV-infected adults starting highly active antiretroviral therapy in Thailand. J Acquir Immune Defic Syndr. 2012; 60: 91–8.
- Zhu H , Napravnik S , Eron J , Cole S , Ma Y , Wohl D , etal. Attrition among human immunodeficiency virus (HIV) – infected patients initiating antiretroviral therapy in China, 2003–2010. PLoS One. 2012; 7: e39414.
- National AIDS Control Organisation. Operational guidelines for ART services. 2012. Available from: http://www.nacoonline.org/upload/Publication/Treatment%20Care%20and%20support/Operational%20guidelines%20for%20ART%20services.pdf [cited 22 Jul 2013].
- World Health Organization. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. 2013. Available from: http://www.who.int/hiv/pub/guidelines/arv2013/en/index.html [cited 20 Jul 2013].
- Alvarez-Uria G , Midde M , Pakam R , Kannan S , Bachu L , Naik PK . Factors associated with late presentation of HIV and estimation of antiretroviral treatment need according to CD4 lymphocyte count in a resource-limited setting: data from an HIV cohort study in India. Interdiscip Perspect Infect Dis. 2012; 2012: 293795.
- Alvarez-Uria G . Factors associated with delayed entry into HIV medical care after HIV diagnosis in a resource-limited setting: data from a cohort study in India. Peer J. 2013; 1: e90.
- Boyles TH , Wilkinson LS , Leisegang R , Maartens G . Factors influencing retention in care after starting antiretroviral therapy in a rural South African programme. PLoS One. 2011; 6: e19201.
- Brinkhof MWG , Pujades-Rodriguez M , Egger M . Mortality of patients lost to follow-up in antiretroviral treatment programmes in resource-limited settings: systematic review and meta-analysis. PLoS One. 2009; 4: e5790.
- Ware NC , Wyatt MA , Geng EH , Kaaya SF , Agbaji OO , Muyindike WR , etal. Toward an understanding of disengagement from HIV treatment and care in sub-Saharan Africa: a qualitative study. PLoS Med. 2013; 10: e1001369.
- Franke MF , Kaigamba F , Socci AR , Hakizamungu M , Patel A , Bagiruwigize E , etal. Improved retention associated with community-based accompaniment for antiretroviral therapy delivery in rural Rwanda. Clin Infect Dis. 2013; 56: 1319–26.
- Bagchi S . Telemedicine in rural India. PLoS Med. 2006; 3: e82.
- Srikantiah P , Ghidinelli M , Bachani D , Chasombat S , Daoni E , Mustikawati DE , etal. Scale-up of national antiretroviral therapy programs: progress and challenges in the Asia Pacific region. AIDS. 2010; 24(Suppl 3): S62–71.
- Alvarez-Uria G , Naik PK , Pakam R , Bachu L , Midde M . Natural history and factors associated with early and delayed mortality in HIV infected patients treated of tuberculosis under directly observed treatment short course (DOTS) strategy: a prospective cohort study in India. Interdiscip Perspect Infect Dis. 2012; 2012: 502012.
- Koenig SP , Riviere C , Leger P , Joseph P , Severe P , Parker K , etal. High mortality among patients with AIDS who received a diagnosis of tuberculosis in the first 3 months of antiretroviral therapy. Clin Infect Dis. 2009; 48: 829–31.
- Wubshet M , Berhane Y , Worku A , Kebede Y . Death and seeking alternative therapy largely accounted for lost to follow-up of patients on ART in northwest Ethiopia: a community tracking survey. PLoS One. 2013; 8: e59197.