Abstract
Background
Prior to the scale-up of antiretroviral therapy (ART), demographic surveillance cohort studies showed higher mortality among migrants than residents in many rural areas.
Objectives
This study quantifies the overall and AIDS-specific mortality between migrants and residents prior to ART, during ART scale-up, and after widespread availability of ART in Rufiji district in Tanzania.
Design
In Health and Demographic Surveillance System (HDSS), the follow-up of individuals aged 15–59 years was categorized into three periods: before ART (1998–2003), during ART scale-up (2004–2007), and after widespread availability of ART (2008–2011). Residents were those who never migrated within and beyond HDSS, internal migrants were those who moved within the HDSS, and external migrants were those who moved into the HDSS from outside. Mortality rates were estimated from deaths and person-years of observations calculated in each time period. Hazard ratios were estimated to compare mortality between migrants and residents. AIDS deaths were identified from verbal autopsy, and the odds ratio of dying from AIDS between migrants and residents was estimated using the multivariate logistic regression model.
Results
Internal and external migrants experienced higher overall mortality than residents before the introduction of ART. After widespread availability of ART overall mortality were similar for internal and external migrants. These overall mortality experiences observed were similar for males and females. In the multivariate logistic regression model, adjusting for age, sex, education, and social economic status, internal migrants had similar likelihood of dying from AIDS as residents (adjusted odds ratio [AOR]=1.14, 95% confidence interval [CI]: 0.70–1.87) while external migrants were 70% more likely to die from AIDS compared to residents prior to the introduction of ART (AOR=1.70, 95% CI: 1.06–2.73). After widespread availability of ART with the same adjustment factors, the odds of dying from AIDS were similar for internal migrants and residents (AOR=1.56, 95% CI: 0.80–3.04) and external migrants and residents (AOR=1.42, 95% CI: 0.76–2.66).
Conclusions
Availability of ART has reduced the number of HIV-infected migrants who would otherwise return home to die. This has reduced the burden on rural communities who had cared for the return external migrants.
This paper is part of the Special Issue: Measuring HIVAssociated Mortality in Africa. More papers from this issue can be found at http://www.globalhealthaction.net
Rural-urban migration pattern is the dominant form of mobility in developing countries characterized by youth migrating to urban cities in search for work, better life, and advanced education (Citation1). The reverse pattern is commonly characterized by people returning home after retirement (Citation2–Citation4). A substantial proportion of research on migrations and health has focused much on the growing population of urban migrants, where emphasis has been on increased vulnerability to poor health and acquisition of diseases relative to urban residents. However, upon their return to rural areas, little is known about their health status and survival relative to rural residents. Public health research on migration patterns provides insights on factors that drive mobility and their influence on health-seeking behavior, disease transition, and mortality.
In the process of integrating with urban residents, rural-urban migrants are more likely to be exposed to HIV-related risky sexual behavior and HIV infection than their urban counterpart (Citation5–Citation7). In developing countries, there is a growing evidence of higher HIV prevalence for return rural migrants compared to rural residents (Citation8–Citation10). In South Africa, Welaga described the mortality differentials between migrants and nonmigrants in a rural community in South Africa (Citation11). After adjusting for age, sex, and social economic status, this study showed higher overall mortality and elevated odds of dying from AIDS for external migrants compared to residents. Another rural cohort study in a similar setting in South Africa reported higher mortality for external migrants than residents in communities with circular labor migrants (Citation12).
Before the introduction of free antiretroviral therapy (ART), the majority of infected migrants could not afford treatment cost in urban centers approximated at US$35/month, and often returned to their rural home villages to seek care from traditional healers, and to be looked after by their families in anticipation of death (Citation13–Citation17). In Thailand, Knodel reported consistent patterns of adults with AIDS migrating home to seek care from their parents at final stages of illness (Citation17).
Overall ART coverage in Tanzania was estimated at 42% among adults and 18% among children by 2010, following the introduction of free ART services (Citation18–Citation21). Several studies have investigated the differentials in treatment access and reported higher loss to follow-up in the continuum of care, less good adherence to care, and treatment by migrants than residents (Citation22–Citation25). We anticipate and hypothesize that the scaling-up of free ART program may possibly contribute to a reduction in return migrants seeking terminal care in rural areas (Citation26–Citation30). However, there are few reports on mortality among rural migrants in Africa, and how this has been affected by HIV and the availability of ART.
Evaluating differentials in mortality among migrants and residents in rural requires continuous follow-up and documentation of death events of both migrants and residence. In addition, evaluation of AIDS-related mortality requires further follow-up that documents cause of death for both migrants and residence. This study focuses on the longitudinal follow-up of residents and migrants from 1998 to 2011 in a rural setting in Rufiji district in Tanzania. The district is located 170 km from Dar-es-Salaam, the largest and closest city with approximately 4.36 million inhabitants. Majority of migrants from Rufiji relocate to Dar-es-salaam while maintaining links with their parents and families. This study quantifies differences in overall and AIDS-specific mortality between migrants and residents and investigates changes in the mortality risks and likelihood of dying from AIDS before ART was introduced, during ART scale-up, and after widespread availability of ART in the rural district of Rufiji in Tanzania.
Methods
Study area
This study used data collected from Rufiji Health and Demographic Surveillance System (HDSS) in Tanzania. The HDSS covers 38 villages, with approximately 95,000 individuals in about 19,000 households and it covers approximately 50% of district population. Rufiji HDSS is a member of the INDEPTH Network (Citation31) and of the Analysing Longitudinal Population-based HIV data in Africa (ALPHA) network (Citation32).
The surveillance is designed as an open cohort of individuals who enter through initial census enumeration, birth, and in-migration and exit through out-migration, lost to follow-up, and death. An initial census was conducted between October 1998 and January 1999 by enumerating all individuals in the selected study area. Basic demographic events of birth, deaths, in- and out-migration were regularly documented during household visits that are normally conducted once in every 4 months. Baseline socioeconomic (education and occupation) and environmental (source of drinking water and type of toilet facilities) factors were collected during the initial census and in follow-up rounds.
Residency status definition
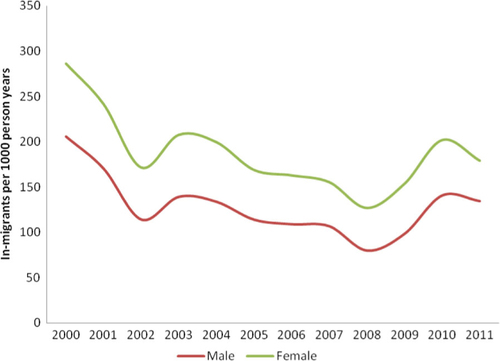
Individuals migrating into the surveillance area are registered if they have been in the surveillance for at least 4 months and are expecting to stay in the study area for a longer period of time, or if they are married to a resident. Information on reasons for migration and where the migrant came from is also collected. Annually about 6,000 individuals aged 15–59 years migrate within or into the study area. Patterns of migration for males and females between 2000 and 2011 are shown in .
Residents were defined as all individuals who were present during initial census, or were born into the cohort, or who had resided in the same household for 2.5 years. Individuals who migrated into the study area from outside the surveillance area were classified as external migrants from the date of migration until 2.5 years after migration. Those who changed location within the study area were considered as internal migrants from the date of migration until 2.5 years after migration. After 2.5 years, both external and internal migrants were considered residents.
ART period definition
All individuals aged 15 to 59 years in the study area from 2000 to 2011 were included in the analysis. The total person-years of observation (PYO) were calculated from 1 January 2000, or the date the individual entered the cohort, at the age of 15 years, or through migration until the date the person died, left the HDSS, was lost to follow-up, attained the age of 60 years, or at the end of analysis period (31 December 2011). The observation time was divided into three periods for this analysis: period prior to availability of ART (2000–2003), period when ART was scaled-up (2004–2007), and period of widespread availability of ART (2008–2011). Within each period, all deaths and person-years of follow-up were recorded, and the overall mortality rates were calculated for residents and migrants separately.
Cause of death
The cause of death information of all registered deaths was derived from verbal autopsy (Citation33). The process involves interviewing close relatives of the deceased through a structured questionnaire that details an account of the sequence of events and symptoms leading to death. Two sets of questionnaire were implemented between 1999 and 2011, but the basic questions necessary to detect AIDS deaths did not differ between the two questionnaires. Structured questionnaires were then reviewed by two independent physicians and the cause of death was assigned using International Classification of Diseases, tenth revision (ICD10) (Citation34). A third physician was involved in cases of disagreement between the two. Where we have all three discordant, the cause was registered as ‘undetermined’. Validated studies have shown that the verbal autopsy procedure is among reliable tools for identifying AIDS deaths in the absence of reliable medical death certificate (Citation35–Citation37).
Statistical analysis
Descriptive analysis described all cause and AIDS-related mortality for migrants and residents stratified by sex and ART period. Predictive analysis used statistical models to compare residents and migrants adjusted for sex, age, level of education, and social economic status. Age categories were generated by splitting residency episodes at age 15, 25, 40, and 60 years. Education level was collected during regular updates of household and individual level variables. Social economic status variable was generated from principal component analysis of household ownership of selected items including bicycle, car, motor cycle, radio, fridge, TV, watch, land, sofa set, bed, video, mattress, water pump, animals such as cow, tailoring machine, satellite dish, iron, fan, concrete floor, water sources, and type of energy used for cooking (Citation38).
Multivariate survival model
Since Rufiji HDSS does not collect data on HIV status of participants, all cause mortality rates were estimated for residents and external and internal migrants with mortality rate ratios (RRs) and 95% confidence intervals (95% CI) comparing migrants to residents. In each ART period, we compared all cause mortality for residents and migrants using multivariate Poisson regression obtaining hazard rate ratios (HRR) and 95% CIs, adjusting for possible confounders.
Logistic regression for AIDS deaths
We evaluated AIDS mortality from the verbal autopsy cause of death, defining a binary response variable of AIDS death or not AIDS death. In each ART period, we used a multivariate logistic regression to assess the adjusted odds ratio (AOR) of dying from AIDS for external migrants and internal migrants compared to residents, adjusting for age, sex, education, and socioeconomic status. Stata software version 12 (StataCorp, College Station, TX) was used to perform all statistical analysis.
Results
Overall mortality in 4 years
shows results of longitudinal follow-up of adults aged 15–59 years with a total of 428,010 person-years, and 2,653 deaths recorded from 2000 through 2011. Crude mortality rates were stratified by gender and ART periods, and were higher for external migrants than residents before and during ART scale-up (RR=1.38, 95% CI: 1.16–1.63 and RR=1.40, 95% CI: 1.13–1.64, respectively). After widespread availability of ART, mortality was comparable for residents and external migrants (RR=1.14, 95% CI: 0.92–1.40). Similar patterns of overall mortality were observed for males and females.
Table 1 Adult (aged 15 to 59 years of age) deaths, person-years of observation (PYO), overall mortality and mortality RR over ART periods stratified by gender
Internal migrants were observed with higher mortality than residents before ART (RR=1.22, 95% CI: 1.04–1.43), while lower mortality rates comparable to residents were observed during scale-up and after widespread availability (RR=1.14, 95% CI: 0.96–1.35 and RR=0.91, 95% CI: 0.74–1.13), respectively. Sex-specific mortality rates for residents and internal migrants were comparable over all ART periods, except during ART scale-up when female internal migrants were observed with higher mortality than residents.
Estimates from the multivariate survival model in indicate that internal and external migrants had a higher mortality rate than residents after adjusting for sex, age, education, and economic status. Compared to residents, higher mortality rates were observed among external migrants [adjusted hazard ratio (AHR)=1.54, 95% CI: 1.30–1.84] and internal migrants (AHR=1.24, 95% CI: 1.05–1.46) before ART was available. During ART scale-up, external migrants continued to show persistently higher mortality rates than residents (AHR=1.43, 95% CI: 1.17–1.73), while internal migrant's mortality was higher compared residents but not statistically significant (AHR=1.13, 95% CI: 0.95–1.35). Internal and external migrants had comparable mortality rates to residents after widespread availability of ART.
Table 2 Adjusted relative risk for multivariate models for the 4 years survival experience by migration status and ART period
Logistic regression model for AIDS deaths
shows the number of deaths assessed using verbal autopsy and the proportion that was identified as AIDS deaths. In the crude analysis, there were no significant associations between AIDS death and residency status within males and females separately and over all ART periods. In a multivariate logistic regression of all deaths (), adjusting for sex, age, education, and social economic status, external migrants were 70% more likely to die from AIDS compared to residents before the introduction of ART (AOR=1.70, 95% CI: 1.06–2.73). During ART scale-up and after widespread availability of ART, there were no significant differences in the odds of AIDS mortality between residents, internal migrants, and external migrants.
Table 3 Characteristics of participants included in the AIDS mortality model
Table 4 Adjusted odds ratio for multivariate logistic regression model for factors associated with AIDS deaths by migration status and ART period
Reasons for migration
The dominant reason for migration among deceased individuals varied depending on the ART period as shown in . Prior to the introduction of ART, about 50% of diseased external migrants were reported to follow their parents as their main reason for migration into the study area. Among external migrants, 8% moved to the study area to seek for treatment compared to 2.4% of internal migrants. After widespread availability of ART, patterns of reasons for migration changed for external migrants, where the proportion of external migrants reported following parents decreased from 50 to 34%. The proportion of external migrants returning to seek for treatment decreased from 8% prior ART to 5% during ART scale-up and 1.8% after widespread availability of ART.
Table 5 Reasons for migration for deceased adults’ Pre-ART, ART scale up and Post ART
Discussion
This study shows higher overall mortality among external migrants compared to residents before ART became widely available in the district. Internal migrants also had higher mortality than residents before the introduction of ART. Decreasing trends in mortality rates were noted for both migrants and residents between 2000 and 2011. Sex-specific crude mortality rate for external migrants was higher for males than females. Although the overall mortality rates for females were slightly higher than those of males, there was no statistical difference in the adjusted analysis comparing male and female mortality rates in any of ART periods. Prior to ART introduction, the odds of an AIDS death was significantly higher among deaths in external migrants than in residents (AOR=1.70, 95% CI: 1.06–2.73). After widespread availability of ART, there remained higher odds of AIDS deaths among deaths in external migrants than in residents, but this was no longer significant (AOR=1.42, 95% CI: 0.76–2.66). Females were more likely to die from AIDS than males during all ART periods.
Both the crude mortality analysis and subanalysis of those who died affirm our hypothesis that scaling-up of free ART programs may possibly have contributed to the reduction of return migrants seeking care in rural areas as a result of improved health status and survival among those on ART treatment. Elevated odds of dying from AIDS for external migrants compared to residents observed in this study were comparable with findings from other cohort studies in Rural South Africa before the introduction of ART (Citation11, Citation12).
The introduction of free ARV in 2004, in Tanzania, may have influenced HIV-infected migrants to stay in urban areas, who would otherwise return home for palliative care while waiting to die in the absence of treatment. This is reflected in the reduced risk of death and odds of AIDS deaths for migrants after widespread availability of ART. Treatment and care for HIV patients were made available and accessible for free to majority of health centers and hospital hence reduced migration of AIDS-infected individual to rural areas previously induced by AIDS-related illness and morbidity. High AIDS mortality rate for males external migrants compared to females could be attributed by lower ARV coverage among males as reported in routine health system in Tanzania (Citation10, Citation22) and other parts of the world (Citation24). This is due to the fact that more females than males are accessing ART services through provider-initiated programs, where all females attending antenatal clinic are counseled, tested for HIV, and those with the disease are enrolled on care or treatment (Citation19).
Analysis of reasons for migration could be used to factor out the ‘coming home to die’ concept from other possible factors pulling individuals to rural areas. Before ART was available, more than half of the deceased external migrants reported to follow parents as their main reason for migration. However, following parents could possibly feature ‘follow parent for care or possibly die’ because the majority who reported this reason were in the age of independence (25–59 years) from their parents. This means that they may possibly return home not to stay with their parents but seek for care or treatment from their parents or relative. In many developing countries affected by the HIV epidemic, mothers are highly involved in the care of their infected sons and daughters to the point of death as well as the care of orphans left behind by their children. Majority of infected return migrants did not report return home for care or treatment as their main reason for migration in an attempt to hide their HIV. This was mainly contributed by high stigma behaviour in the study area toward HIV positive individuals and ARV users (Citation39, Citation40). Men's superiority behavior observed elsewhere may also influence some of the male respondents not to report return home for care or treatment in an effort to maintain their status quo (Citation39–Citation41). Following widespread availability of ART, diseased individuals reporting ‘follow parents’ decreased from 50 to 34%. External migrants group was also reported to have the highest percentage of those reported returning home to seek treatment compared to internal migrants. Other reasons for migration, such as retirement, contribute little to reasons of return migrants because majority (approximately 80%) of internal and external migrants were in the age range between 25 and 59 years, while retirement age in Tanzania is 60 years and above. Since the quality of health care in urban areas is often superior to rural, then seeking care in rural could mean consulting traditional healers or waiting to die from incurable diseases such as AIDS.
This study has several limitations that need to be considered when interpreting the findings and make general conclusions to other settings. The analysis of this HDSS data mainly depended on mortality events rather than HIV prevalent cases. If HIV sero-surveys were available in the study area, we could provide more concrete analysis on return migrants and residents by HIV status. The subset analysis of those who died in the study area could be more precise in settings where the HIV status of migrants and residents was available. This analysis is restricted to individuals aged 15–59 years; therefore, care should be taken in extrapolating results to individual aged below 15 years and above 60 years. Comparability of cause of deaths over time and misclassification HIV/AIDS-related deaths should be taken into consideration. Although verbal autopsy has been successful in detecting HIV/AIDS deaths (Citation35–Citation37), comparability of results generated by physicians may not be consistent due to their changes in general perception of local AIDS epidemic. While some physician may perceive AIDS mortality decreasing in the population and tend to assign less frequent AIDS deaths during cause of death assignment, others may regard AIDS mortality a growing public health concern and assign AIDS death more frequent. Over the last 10 years there have been changes in physicians who assign cause of death. This could possibly result in changes in number of deaths assigned as HIV/AIDS death due to differences in implementing ICD10 procedures among physicians. TB and HIV misclassification is another limitation in this study. Co-infection of the diseases and existence of similarity in signs and symptoms may lead to misclassification (Citation42, Citation43). In this study, we have taken the definition of AIDS death alone, though some other studies have grouped together the two diseases (Citation44).
The findings in this study support the widespread evidence of benefits of ART on premature mortality and population mobility among HIV-positive migrants.
Conclusions
This work has provided evidence that ART's universal access policy in Tanzania has averted a substantial number of deaths connected with AIDS in rural areas among internal and external migrants. Prior to ART scale-up, critically ill AIDS patients preferred to migrate to rural for care and possibly die because of the absence of affordable treatment and care. The return rural-urban migrants who are critically ill contributed in burdening the already unstable rural health-care system and families. Widespread availability of ART has reduced the burden of care to families and health-care system in rural areas. Reduction of AIDS patients seeking care in rural may have resulted in savings for families, increased time for economic activities, especially in agriculture and improving other sectors of health such maternal and newborn health.
Projection studies show 50% of African inhabitants will be living in urban area by 2,025 implying increased rural-urban migrants in the future (Citation3). The fact that rural-urban migrants are more likely to engaging in risky sexual behaviors, health-care planners need long-term plans and investments in strengthening HIV/AIDS education both to rural and urban inhabitants. Reducing the gap in access to ARV among the poor should be the key factor in designing intervention programs aimed at optimizing the effect of ARV's to both migrants and residents. This is due to the fact that majority of rural-urban migrants are poor and their access to ARV may be compromised compared to those who are economically well in urban.
Ethical review
The study received ethical clearance from the institutional review board of the Ifakara Health Research and Development Centre (Now Ifakara Health Institute) and the Tanzanian Medical Research Coordinating Committee.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
Acknowledgements
We thank Ifakara Health Institute's staff at RHDSS at field and data section for collecting and storing the data in usable format. Special thanks to the ALPHA network for building capacity to HDSS staff's on longitudinal data analysis. The analysis for this paper was funded through the ALPHA network grant from the Wellcome Trust to LSHTM, grant ref number 090959/Z/09/Z.
Notes
This paper is part of the Special Issue: Measuring HIVAssociated Mortality in Africa. More papers from this issue can be found at http://www.globalhealthaction.net
References
- Kulabako RN. Environmental health practices, constraints and possible interventions in peri-urban settlements in developing countries – a review of Kampala, Uganda. Int J Environ Health Res. 2010; 20: 231–57.
- Kulu H, Milewski N. Family change and migration in the life course. Demogr Res. 2007; 17: 567–90.
- Zulu E, Dodoo F, Ezeh A. HIV and AIDS in Africa: beyond epidemiology. 2004; Malden, MA: Blackwell.
- Braun van J. Towards a renewed focus on rural development. Agric Rural Dev J. 2004; 2: 4–6.
- Lindstrom DP, Hernández CH. Internal migration and contraceptive knowledge and use in Guatemala. Int Fam Plan Perspect. 2006; 32: 146–53.
- Coast E. Local understandings of, and responses to, HIV: rural–urban migrants in Tanzania. Soc Sci Med. 2006; 63: 1000–10.
- Marston M, Michael D, Wringe A, Isingo R, Clark BD, Jonas A, etal. The impact of antiretroviral therapy on adult mortality in rural Tanzania. Trop Med Int Health. 2012; 17: e58–65.
- Voeten HA, Vissers DC, Gregson S, Zaba B, White RG, de Vlas SJ, etal. Strong association between in-migration and HIV prevalence in urban sub-Saharan Africa. Sex Transm Dis. 2010; 37: 240–3.
- Zhang L, Chow EP, Jahn HJ. High HIV prevalence and risk of infection among rural-to-urban migrants in various migration stages in China: a systematic review and meta-analysis. Sex Transm Dis. 2013; 40: 136–47.
- Lurie MN, Williams BG, Zuma K, Mkaya-Mwamburi D, Garnett G, Sturm AW, etal. The impact of migration on HIV-1 transmission in South Africa: a study of migrant and nonmigrant men and their partners. Sex Transm Dis. 2003; 30: 149–56.
- Welaga P, Hosegood V, Weiner R, Hill C, Herbst K, Newell M-L. Coming home to die? The association between migration and mortality in rural South Africa. BMC Public Health. 2009; 9: 193.
- Clark SJ, Collinson MA, Kahn K, Drullinger K, Tollman SM. Returning home to die?: circular labour migration and mortality in South Africa. Scand J Public Health. 2007; 69: 35–44.
- Neves D. The impact of illness and death on migration back to the Eastern Cape. 2008; Cape Town: Centre for Social Science Research, University of Cape Town.
- MacPherson D, Gushulak B. Human mobility and population health: new approaches in a globalizing world. Perspect Biol Med. 2001; 44: 390–441.
- Urassa M, Boerma J, Isingo R. The impact of HIV/AIDS on mortality and household mobility in rural Tanzania. AIDS. 2001; 15: 2017–23.
- Ntozi JP, Nakayiwa Y. The continuing HIV/AIDS epidemic in Africa: responses and coping strategies. 1999; Canberra, Australia: Australia National University.
- Knodel J, VanLandingham M. Return migration in the context of parental assistance in the AIDS epidemic: the Thai experience. Soc Sci Med. 2003; 57: 327–42.
- World Health Organization, Joint Program on HIV/AIDS (UNAIDS), United Nations Children's Fund (UNICEF). Global HIV/AIDS response: epidemic update and health sector progress towards Universal Access. 2011; Geneva, Switzerland: WHO Press.
- United Republic of Tanzania. Report of the 3 by 5 mission to Tanzaniaon scaling up antiretroviral treatment as part of the global emergency response to HIV/AIDS. 2003; Dar es Salaam, Tanzania: United Republic of Tanzania. 4–12.
- Somi G, Matee M, Makene CL, Van Den Hombergh J, Kilama B. Three years of HIV/AIDS care and treatment services in Tanzania. Tanzan J Health Res. 2009; 11: 136–43.
- WJCF. William J. Clinton Foundation HIV/AIDS care and treatment plan 2003–2008. 2003; Dar es Salaam, Tanzania: WJCF.
- Kageea A, Remienb R, Berkmanc A, Hoffmanc S, Campos L, Swartza L. Structural barriers to ART adherence in Southern Africa: challenges and potential ways forward. Glob Public Health. 2012; 6: 1–12.
- Camlin CS, Hosegood V, Newell M-L, McGrath N, Bärnighausen T, Snow RC. Gender, migration and HIV in rural KwaZulu-Natal, South Africa. PLoS One. 2010; 5: e11539.
- Remien RH, Chowdhury J, Mokhbat JE, Soliman C, Adawy ME, El-sadr W. Gender and care: access to HIV testing, care, and treatment. J Acquir Immune Defic Syndr. 2009; 51: 106–10.
- The Antiretroviral Therapy Collaboration (ART-CC). Higher rates of AIDS during the first year of antiretroviral therapy among migrants: the importance of tuberculosis. AIDS. 2013; 27: 1321–9.
- Gershengorn HB, Blower SM. Could widespread use of combination antiretroviral therapy eradicate HIV epidemics?. Lancet Infect Dis. 2002; 2: 487–93.
- Blower SM, Aschenbach AN, Gershengorn H, Kahn J. Predicting the unpredictable: transmission of drug-resistant HIV. Nat Med. 2001; 7: 1016–20.
- Bor J, Herbst AJ, Newell M-L, Bärnighausen T. Increases in adult life expectancy in rural South Africa: valuing the scale-up of HIV treatment. Science. 2013; 339: 961–5.
- Blower S, Farmer P. Predicting the public health impact of antiretrovirals: preventing HIV in developing countries. AIDScience. 2003; 11. Available from: http://aidscience.org/Articles/AIDScience033.asp [cited 15 October 2013].
- Iloeje U, Kastango K, Malan N, David N, Krantz E, Su J, etal. Health related quality of life (HRQoL) changes in antiretroviral (ARV) naïve HIV-infected patients on atazanavir based regimens, with (ATV/r) and without (ATV) ritonavir: week 48 results from AI424-089 XVI International AIDS. Conference: August 13–18 2006. XVI International AIDS Conference, 13–18 August 2006; Toronto, Canada: Abstract TUPE0065, 2006.
- INDEPTH Network. Population and health in developing countries volume I: population, health, and survival at INDEPTH sites. 2002; Ottawa, Canada: IDRC.
- Maher D, Biraro S, Hosegood V, Isingo R, Lutalo T, Mushati P, etal. Translating global health research aims into action: the example of the ALPHA network. Trop Med Int Health. 2010; 15: 321–8.
- Snow R, Schellenberg J, Forster D, Winstanley M, Marsh V, Newton C, etal. Childhood deaths in Africa: uses and limitations of verbal autopsies. Lancet. 1992; 340: 351–5.
- Leitao J, Chandramohan D, Byass P, Jakob R, Bundhamcharoen K, Choprapawon C, etal. Revising the WHO verbal autopsy instrument to facilitate routine cause-of-death monitoring. Glob Health Action. 2013; 6: 21518.
- Lopman B, Cook A, Smith J, Chawira G, Urassa M, Kumogola Y, etal. Verbal autopsy can consistently measure AIDS mortality: a validation study in Tanzania and Zimbabwe. J Epidemiol Community Health. 2010; 64: 330–4.
- Byass P, Kahn K, Fottrell E, Mee P, Collinson MA, Tollman SM. Using verbal autopsy to track epidemic dynamics: the case of HIV-related mortality in South Africa. Popul Health Metr. 2011; 9: 46.
- Lopman BA, Barnabas RV, Boerma JT, Chawira G, Gaitskell K, Harrop T, etal. Creating and validating an algorithm to measure AIDS mortality in the adult population using verbal autopsy. PLoS Med. 2006; 3: e312.
- Rabe-Hesketh S, Everitt B. A handbook of statistical analyses using Stata. 2004; New York. Available from: http://www.loc.gov/catdir/enhancements/fy0668/2006049170-d.html [cited 22 April 2014].
- Agnarson AM, Levira F, Masanja H, Ekström AM, Thorson A. Antiretroviral treatment knowledge and stigma – implications for programs and HIV treatment interventions in rural Tanzanian populations. PLoS One. 2013; 8: e53993.
- Agnarson AM, Masanja H, Ekström AM, Eriksen J, Tomson G, Thorson A. Challenges to ART scale-up in a rural district in Tanzania: stigma and distrust among Tanzanian health care workers, people living with HIV and community members. Trop Med Int Health. 2010; 15: 1000–7.
- Nyamhanga TM, Muhondwa EPY, Shayo R. Masculine attitudes of superiority deter men from accessing antiretroviral therapy in Dar es Salaam, Tanzania. Glob Health Action. 2013; 6: 21812.
- van't Hoog AH, Laserson KF, Githui WA, Meme HK, Agaya JA, Odeny LO. High prevalence of pulmonary tuberculosis and inadequate case finding in rural western Kenya. Am J Respir Crit Care Med. 2011; 183: 1245–53.
- Van Eijk AM, Ayisi JG, ter Kuile FO, Misore AO, Otieno JA, Rosen DH, etal. HIV increases the risk of malaria in women of all gravidities in Kisumu, Kenya. AIDS. 2003; 17: 595–603.
- Phillips-Howard PA, Odhiambo FO, Hamel M, Adazu K, Ackers M, van Eijk AM, etal. Mortality trends from 2003 to 2009 among adolescents and young adults in rural Western Kenya using a health and demographic surveillance system. PLoS One. 2012; 7: 47017.