Abstract
Background
The MRC/Wits University Agincourt research centre, part of the INDEPTH Network, has documented mortality in a defined population in the rural northeast of South Africa for 20 years (1992–2011) using long-term health and socio-demographic surveillance. Detail on the unfolding, at times unpredicted, mortality pattern has been published. This experience is reviewed here and updated using more recent data.
Objective
To present a review and summary of mortality patterns across all age-sex groups in the Agincourt sub-district population for the period 1992–2011 as a comprehensive basis for public health action.
Design
Vital events in the Agincourt population have been updated in annual surveys undertaken since 1992. All deaths have been rigorously recorded and followed by verbal autopsy interviews. Responses to questions from these interviews have been processed retrospectively using the WHO 2012 verbal autopsy standard and the InterVA-4 model for assigning causes of death in a standardised manner.
Results
Between 1992 and 2011, a total of 12,209 deaths were registered over 1,436,195 person-years of follow-up, giving a crude mortality rate of 8.5 per 1,000 person-years. During the 20-year period, the population experienced a major HIV epidemic, which resulted in more than doubling of overall mortality for an extended period. Recent years show signs of declining mortality, but levels remain above the 1992 baseline recorded using the surveillance system.
Conclusions
The Agincourt population has experienced a major mortality shock over the past two decades from which it will take time to recover. The basic epidemic patterns are consistent with generalised mortality patterns observed in South Africa as a whole, but the detailed individual surveillance behind these analyses allows finer-grained analyses of specific causes, age-related risks, and trends over time. These demonstrate the complex, somewhat unpredicted course of mortality transition over the years since the dawn of South Africa's democratic era in 1994.
This paper is part of the Special Issue: INDEPTH Network Cause-Specific Mortality. More papers from this issue can be found at http://www.globalhealthaction.net
The Agincourt Health and Socio-Demographic Surveillance System (HDSS) of the MRC/Wits Rural Public Health and Health Transitions Research Unit is an INDEPTH member site situated in the northeast of South Africa. The HDSS has been documenting mortality in a rural population since 1992. As of 2011, the population comprised some 90,000 individuals residing in 16,000 households in 27 villages (Citation1). This paper both reviews the published outputs from Agincourt HDSS relating to mortality and presents detailed overall results based on the 20 year period 1992–2011, as contributed to the INDEPTH Network pooled cause of death analyses covering the Agincourt HDSS and 21 other INDEPTH HDSS sites (Citation2).
Over the two decades the Agincourt site has operated, more than 40 papers have reported on particular aspects of mortality patterns and transitions, and related issues. Several papers have taken an overview of mortality at different points in time. The first signs of a reversal of mortality declines were documented at an early stage of the local HIV/AIDS epidemic (Citation3). Subsequently, the complexities of HIV and TB co-infection were also documented (Citation4), alongside South Africa's new struggle with increasing mortality (Citation5). Throughout, mortality patterns have been seen to be shaped by competing forces of: 1) HIV/AIDS, 2) other communicable and nutritional diseases, 3) non-communicable diseases, and 4) violence and injuries (Citation6, Citation7). Given the high proportions of HIV and TB-related mortality in this population, this has been perceived as a major issue (Citation8–Citation11). Maternal health and fertility, including the effects of the HIV epidemic, have also been important issues (Citation12–Citation14). Child mortality has been explored in relation to various risk factors (Citation15) and adult mortality similarly (Citation16). The relationship between cause of death and beliefs in witchcraft has also been explored (Citation17), as well as mortality related to sleep disorders (Citation18). Connections between mortality and migration, as geographic patterns of residence and work have gradually evolved in the post-apartheid era, have been shown to continue to be important (Citation19–Citation21). Finally, there has been a substantial volume of work that has capitalised on the rich detail of the Agincourt HDSS data in terms of undertaking spatio-temporal analyses of mortality patterns (Citation22–Citation31).
At the same time as measuring mortality patterns, the MRC/Wits Agincourt Research Unit has also served as something of a methodological incubator for mortality surveillance, starting well before the INDEPTH Network was founded in 1998. From the initial descriptions of the Agincourt HDSS and its methods (Citation32, Citation33), a focus on determining cause of death became an important theme (Citation34–Citation37). Agincourt verbal autopsy (VA) data contributed to early work on automated cause of death assignment (Citation38, Citation39). It became clear that computer-coded VA methods were indeed able to track a mortality transition as dramatic as the evolving HIV epidemic in Agincourt (Citation40). Agincourt data again contributed substantially to the development and evaluation of the InterVA-4 VA interpretation model (Citation41) following the release of new WHO standards for VA in 2012 (Citation42). Pilot studies of handheld technology for undertaking VA interviews followed (Citation43).
Against this detailed and complex background of mortality levels and trends in the Agincourt HDSS, and methodological developments in automated cause of death assignment, we present here an overview of cause-specific mortality findings over the 20-year period 1992–2011 for all age groups.
Methods
The MRC/Wits Agincourt Research Unit has maintained individual health and socio-demographic surveillance among a rural population in the Agincourt sub-district, in northeast South Africa, starting in 1992. A detailed description of the site has been presented elsewhere (Citation1). Annual household surveillance update rounds have identified all deaths occurring in the population, and these have been followed up with VA interviews, undertaken by specifically trained interviewers 1–11 months after death. Local physicians have assigned causes of death to the VA material, which has also more recently been processed retrospectively using the InterVA-4 probabilistic model (version 4.02) (Citation41). As far as is possible, the VA instrument and InterVA-4 model aim to arrive at underlying causes of death, but this is not always possible with certainty using VA methods. Nevertheless, it has been established that causes of death based on results generated by the InterVA-4 model do not differ substantially from physician findings (Citation40). In addition, the InterVA-4 model assigns causes of death in a standardised automated manner that is much quicker and more consistent than physician coding. Rates of cause-specific HIV associated mortality using the InterVA-4 model have been explored in a multisite study (Citation44).
The outputs from the InterVA-4 model, up to three causes for each case plus a possible indeterminate residual fraction, for Agincourt contained in the INDEPTH Network Cause-Specific Mortality multisite dataset (Citation45) have been analysed with the same age-sex-time standardisation used for the INDEPTH cross-site comparisons (Citation46). The standardisation was necessary because the age-sex population structure in the Agincourt site changed appreciably over the 20-year period (Citation1). Consequently, in considering changing patterns of causes of death, it is important to standardise the age-sex structure to ensure that changes observed in particular causes are not due to age-sex changes in the population over time. Because the site covers an entire defined population, it is not meaningful to ascribe confidence intervals, although individual-level uncertainty in cause of death is captured through the indeterminate component of the InterVA-4 output.
The Agincourt HDSS was reviewed and approved by the Committee for Research on Human Subjects (Medical) of the University of the Witwatersrand (protocol M960720 and M081145). Community consent from civic and traditional leadership was secured at the start of surveillance and is reaffirmed from time to time, and informed verbal consent is obtained at individual and household level at each annual follow-up visit. A record is kept of the household respondent who consented to be interviewed as well as the responsible fieldworker.
Results
Over the period 1992–2011 a total of 12,209 deaths were registered over 1,436,195 person-years of follow-up, corresponding to a crude mortality rate of 8.5 per 1,000 person-years. After standardisation, these amounted to 13,153 deaths, of which 12,010 (91.3%) had VA interviews successfully completed. For 607 (5.1%) of these, the InterVA-4 model was unable to reach any conclusive cause of death.
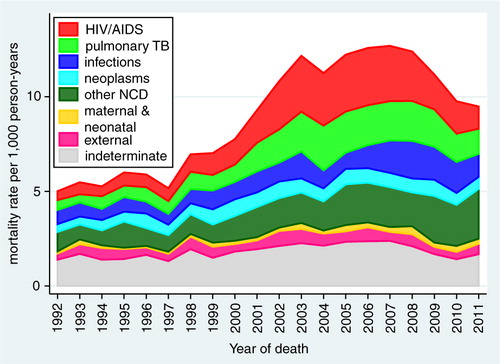
presents detailed standardised mortality rates by age group and causes of death according to the WHO 2012 VA standard categories (Citation47). shows the development of standardised mortality rates by cause categories over time, clearly showing the overall mortality epidemic peak associated with HIV in this population around 2007 and reduction in the most recent time period. shows the same data for the separate WHO 2012 age groups (with neonatal and 1–11 month age groups combined into a single infancy category). In this figure, the vertical scales for mortality rates are appreciably different between the different age groups, with highest rates for infants and over-65 year olds, and lowest rates for the 5–14 year age group. All age groups except the over-65 year olds experienced reduction in mortality rate from around 2007. Mortality increased steadily in the over-65 year olds over the 20-year period. shows trends in non-communicable disease (NCD) mortality in adult age groups. NCD mortality steadily increased in all adult age groups from the late 1990s and declined in the most recent time period only in the 15–49 year age group. The increase in NCD mortality in the 50–64 and 65+ year age groups are largely driven by increases in cardiovascular conditions (including stroke and acute cardiac disease) followed by respiratory conditions (including chronic obstructive pulmonary disease). In the 15–49 year age group, trends in NCD mortality mirror trends in HIV/AIDS mortality.
Fig. 2 Age-sex-time standardised mortality rates by broad cause categories and age group, Agincourt HDSS.
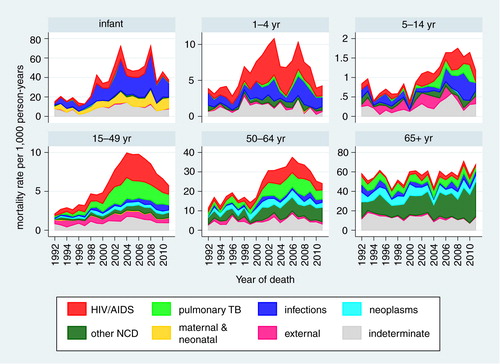
Fig. 3 Age-sex-time standardised non-communicable disease (NCD) mortality in adult age groups, Agincourt HDSS.
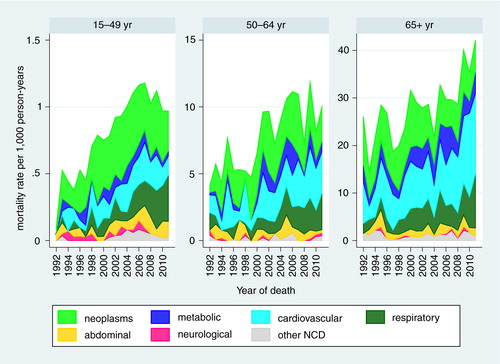
Table 1 Age-sex-time standardised cause-specific mortality rates per 1,000 person-years by WHO 2012 causes and age group, for a total of 12,209 deaths registered over 1,436,195 person-years at the Agincourt HDSS, 1992–2011
Discussion
Mortality findings at the Agincourt HDSS for the overall period 1992–2011 reflect, as expected, many facets from interim publications. This paper provides a 20-year retrospective picture of a community in which mortality patterns changed drastically over time as a consequence of the HIV epidemic, as is clearly visible in . Few epidemics in human history have caused a sudden doubling in all-cause mortality in a particular population, sustained over a decade. There is still some way to go until mortality rates return to near pre-epidemic levels, despite encouraging recent decreases.
Attributing individual deaths unambiguously to HIV, in the absence of biomedical information, is not simple. Another study showed that the InterVA-4 model achieved a high level of specificity for HIV/AIDS related mortality in relation to sero-status (Citation44). However, it was also clear that, given higher cause-specific mortality rates for other causes among HIV positives, substantial proportions of HIV-related mortality are likely not to be attributed as such. This is seen in the Agincourt population, with substantially higher rates of TB, other infections, and NCDs during the peak incidence of HIV/AIDS deaths. There may also be some concomitant increases in NCD mortality rates due to other risk factors such as smoking and obesity, but the INDEPTH multisite analysis of adult NCD mortality showed significant correlations between HIV and NCD mortality, over a wide range of rates (Citation48).
details the effects of the HIV epidemic on each age group. Although in infancy HIV/AIDS as a specific cause was not the major cause of death, it is clear that other infections were mainly responsible for the increase in infant deaths due to the peak of the overall epidemic. It must be presumed therefore that these additional infant deaths due to other infections were associated with HIV. In the 1–4 year age group, the major increases appear to be more clearly associated with clinically typical HIV/AIDS, and hence a large part of the additional mortality was assigned as such. The mortality peaks both for the infant and 1–4 year age groups appear to slightly precede the peaks in older age groups. On the assumption that most of the childhood HIV/AIDS deaths would follow perinatally acquired infections, this may reflect young children developing disease fairly rapidly and dying from HIV-related causes before their mothers also went on to die, particularly at the stage before prevention of mother to child transmission (PMTCT) and adult anti-retroviral treatment (ART) programmes were well established in South Africa. It is not clear what would have caused the two peaks in the infant and child mortality patterns, but because they occurred during the time of peak HIV/AIDS mortality, they could have resulted from inconsistencies in the provision of PMTCT. For the 5–14 year age group, the peak of HIV-related mortality was later than in other age groups. HIV still accounted for a substantial increase in the relatively low overall mortality rates in this age group, presumably largely reflecting perinatal infections some years earlier in a sub-group of children who survived for several years. A study of mortality in young people found that HIV and TB combined was the third ranking cause of death globally in the 10–14 age group (Citation49), and HIV/AIDS was the leading cause of adolescent hospitalisation in Zimbabwe (Citation50).
Among adults, the 15–49 year age group had the largest proportion of HIV/AIDS deaths, though the cause-specific rate was lower than in the 50–64 year age group. In both of those age groups, rates of TB and NCDs increased substantially with the increase in HIV/AIDS, but there was no sign of NCDs decreasing in later years as HIV/AIDS and TB decreased. The 65+ year age group was the least affected by HIV/AIDS, as might be expected, although the relatively small proportion of HIV/AIDS deaths in this age group even during the epidemic peak amounted to an appreciable mortality rate, given the high overall mortality in this age group. As would be expected, NCDs accounted for the single largest category in this age group, and also increased over time.
Despite improvement since 2007, and contrary to global trends, infant and under-5 mortality rates () remained substantially higher in 2011 than they were 20 years earlier. There is still some way to go to achieving reductions in these key parameters, not only in relation to HIV/AIDS, but also in terms of further improvements in the provision of maternal and perinatal health care. Inevitably the major political changes in South Africa over the same period are likely to have also affected mortality rates. However, from an analytical perspective, given the overwhelming impact of the HIV epidemic, it is hard to distinguish the effects of socio-political developments on mortality.
From a methodological perspective, despite some shortcomings associated with the use of proxy respondents (common to all VA methods), and that vital events are updated annually in Agincourt resulting in longer recall periods and potentially underestimating perinatal and infant mortality (Citation1), the evidence is very clear that the surveillance operations mounted in the Agincourt HDSS have succeeded to a large extent in identifying and registering deaths, and subsequently determining cause of death. The use of the WHO 2012 VA standard and the InterVA-4 model, even as applied here retrospectively to VA material that was not originally envisaged to be computer coded, has resulted in a plausible picture of a major epidemic. This was possible even though the methods had no means of ‘knowing’ about the development of the epidemic. This clearly demonstrates that it is feasible to use a general model for cause of death assignment, which does not need to be fed with local knowledge of mortality patterns and changes.
The analyses in this paper were restricted by the available data, and conformed to WHO-defined age groups and cause categories. We anticipate forthcoming papers utilizing advanced statistical analysis techniques and an extended time period to capture more fully the effects of the public sector rollout of ART and also assess the impacts of the seismic political and social changes following the abolition of racial segregation (apartheid), including the changing exposures associated with evolving patterns of migration and livelihoods, and the first universal elections in South Africa in 1994.
Conclusions
The Agincourt population has experienced a major mortality shock over the past two decades, from which it will take time to recover. The basic mortality pattern is consistent with the generalised pattern of mortality from an unfinished burden of communicable and nutritional diseases, HIV/AIDS, NCD, and violence and injuries observed elsewhere in South Africa (Citation51–Citation54), but the detailed individual surveillance behind these analyses allows finer-grained analyses of specific causes, age-related risks, and trends over time. The mortality trends presented here contribute to the understanding of South Africa's progress towards the achievement of some of the health-related millennium development goals. Most important, the trends highlight the importance of monitoring the evolution of NCD conditions and their risk factors and the need for South Africa to focus on their prevention, control, and treatment while continuing to strengthen HIV/AIDS prevention and treatment programmes in order to achieve further reductions in mortality rates.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
Acknowledgements
Thanks are due to key funding partners of the MRC/Wits Rural Public Health and Health Transitions Research Unit who have enabled the ongoing Agincourt Health and Socio-demographic Surveillance System: the Wellcome Trust, UK (grants 058893/Z/99/A, 069683/Z/02/Z, and 085477/Z/08/Z); the Medical Research Council, University of the Witwatersrand, and Anglo-American Chairman's Fund, South Africa; the William and Flora Hewlett Foundation (grant 2008-1840), the Andrew W. Mellon Foundation, and the National Institute on Aging (NIA) of the National Institutes of Health (NIH), USA (grants 1R24AG032112-01 and 5R24AG032112-03). This paper contributes to the Programme on Economic Evaluation of Child and Maternal Health Interventions (PEECHi), funded by the South African Department of Health and Medical Research Council. We are grateful to the INDEPTH Secretariat for organising and funding a series of data analysis and scientific writing workshops in Ghana, Thailand, Belgium and UK through core support grants from Sida (Research Cooperation), the Wellcome Trust and the William & Flora Hewlett Foundation.
Notes
This paper is part of the Special Issue: INDEPTH Network Cause-Specific Mortality. More papers from this issue can be found at http://www.globalhealthaction.net
References
- Kahn K, Collinson MA, Gómez-Olivé FX, Mokoena O, Twine R, Mee P, etal. Profile: Agincourt health and socio-demographic surveillance system. Int J Epidemiol. 2012; 41: 988–1001. [PubMed Abstract] [PubMed CentralFull Text].
- INDEPTH Network Cause-Specific Mortality Writing Group. Cause-specific mortality in Africa and Asia: evidence from INDEPTH Health and Demographic Surveillance System sites. Glob Health Action. 2014; 7: 25362. http://dx.doi.org/10.3402/gha.v7.25362 .
- Tollman SM, Kahna K, Garenne M, Gear JS. Reversal in mortality trends: evidence from the Agincourt field site, South Africa, 1992–1995. AIDS. 1999; 13: 1091–7. [PubMed Abstract].
- Zwang J, Garenne M, Kahn K, Collinson M, Tollman SM. Trends in mortality from pulmonary tuberculosis and HIV/AIDS co-infection in rural South Africa (Agincourt). Trans Roy Soc Trop Med Hyg. 2007; 101: 893–8. [PubMed Abstract].
- Kahn K, Garenne ML, Collinson MA, Tollman SM. Mortality trends in a new South Africa: hard to make a fresh start. Scand J Publ Health. 2007; 35(Suppl 69): 26–34.
- Tollman SM, Kahn K, Sartorius B, Collinson MA, Clark SJ, Garenne ML. Implications of mortality transition for primary health care in rural South Africa: a population-based surveillance study. Lancet. 2008; 372: 893–901. [PubMed Abstract] [PubMed CentralFull Text].
- Houle B, Clark SJ, Gómez-Olivé FX, Kahn K, Tollman SM. The unfolding counter-transition in rural South Africa: mortality and cause of death, 1994–2009. PLoS One. 2014; 9: e100420. [PubMed Abstract] [PubMed CentralFull Text].
- Pronyk P, Kahn K, Hargreaves J, Tollman S, Collinson M, Hausler H, etal. Undiagnosed pulmonary tuberculosis deaths in rural South Africa. Int J Tubercul Lung Dis. 2004; 8: 796–9.
- Pronyk PM, Kahn K, Tollman SM. Using health and demographic surveillance to understand the burden of disease in populations: The case of tuberculosis in rural South Africa. Scand J Publ Health. 2007; 35(Suppl 69): 45–51.
- Sharrow DJ, Clark SJ, Collinson MA, Kahn K, Tollman SM. The age pattern of increases in mortality affected by HIV: Bayesian fit of the Heligman-Pollard model to data from the Agincourt HDSS field site in rural northeast South Africa. Demographic Res. 2013; 29: 1039.
- Sharrow DJ, Clark SJ, Raftery AE. Modeling age-specific mortality for countries with generalized HIV epidemics. PLoS One. 2014; 9: e96447. [PubMed Abstract] [PubMed CentralFull Text].
- Garenne M, Kahn K, Collinson M, Gómez-Olivé X, Tollman S. Protective effect of pregnancy in rural South Africa: questioning the concept of indirect cause of maternal death. PLoS One. 2013; 8: e64414. [PubMed Abstract] [PubMed CentralFull Text].
- Garenne M, Kahn K, Collinson MA, Gómez-Olivé FX, Tollman S. Maternal mortality in rural South Africa: the impact of case definition on levels and trends. Int J Wom Health. 2013; 5: 457.
- Garenne ML, Tollman SM, Collinson MA, Kahn K. Fertility trends and net reproduction in Agincourt, rural South Africa, 1992–2004. Scand J Publ Health. 2007; 35(Suppl 69): 68–76.
- Houle B, Stein A, Kahn K, Madhavan S, Collinson M, Tollman SM, etal. Household context and child mortality in rural South Africa: the effects of birth spacing, shared mortality, household composition and socio-economic status. Int J Epidemiol. 2013; 42: 1444–54. [PubMed Abstract] [PubMed CentralFull Text].
- Gómez-Olivé FX, Thorogood M, Bocquier P, Mee P, Kahn K, Berkman L. Social conditions and disability related to the mortality of older people in rural South Africa. Int J Epidemiol. 2014. dyu093.
- Fottrell E, Tollman S, Byass P, Golooba-Mutebi F, Kahn K. The epidemiology of ‘bewitchment as a lay-reported cause of death in rural South Africa. J Epidemiol Community. 2012; 66: 704–709.
- Gómez-Olivé FX, Thorogood M, Kandala N-B, Tigbe W, Kahn K, Tollman S, etal. Sleep problems and mortality in rural South Africa: novel evidence from a low-resource setting. Sleep Med. 2014; 15: 56–63.
- Clark SJ, Collinson MA, Kahn K, Drullinger K, Tollman SM. Returning home to die: circular labour migration and mortality in South Africa. Scand J Publ Health. 2007; 35(Suppl 69): 35–44.
- Collinson MA, White MJ, Bocquier P, McGarvey ST, Afolabi SA, Clark SJ. Migration and the epidemiological transition: insights from the Agincourt sub-district of northeast South Africa. Glob Health Action. 2014; 7: 23524. http://dx.doi.org/10.3402/gha.v7.23524 .
- Hargreaves JR, Collinson MA, Kahn K, Clark SJ, Tollman SM. Childhood mortality among former Mozambican refugees and their hosts in rural South Africa. Int J Epidemiol. 2004; 33: 1271–8. [PubMed Abstract].
- Mee P, Collinson MA, Madhavan S, Root ED, Tollman SM, Byass P, etal. Evidence for localised HIV related micro-epidemics associated with the decentralised provision of antiretroviral treatment in rural South Africa: a spatio-temporal analysis of changing mortality patterns (2007–2010). J Global Health. 2014; 4: 010403.
- Musenge E, Chirwa TF, Kahn K, Vounatsou P. Bayesian analysis of zero inflated spatiotemporal HIV/TB child mortality data through the INLA and SPDE approaches: applied to data observed between 1992 and 2010 in rural North East South Africa. Int J Applied Earth Observation Geoinformation. 2003; 22: 86–98.
- Musenge E, Vounatsou P, Collinson M, Tollman S, Kahn K. The contribution of spatial analysis to understanding HIV/TB mortality in children: a structural equation modelling approach. Glob Health Action. 2013; 6: 19266. http://dx.doi.org/10.3402/gha.v6i0.19266 [PubMed Abstract].
- Musenge E, Vounatsou P, Kahn K. Space-time confounding adjusted determinants of child HIV/TB mortality for large zero-inflated data in rural South Africa. Spat Spatiotemporal Epidemiol. 2011; 2: 205–17. [PubMed Abstract].
- Sartorius B. Modelling determinants, impact, and space-time risk of age-specific mortality in rural South Africa: integrating methods to enhance policy relevance. Glob Health Action. 2013; 6: 19239. http://dx.doi.org/10.3402/gha.v6i0.19239 [PubMed Abstract].
- Sartorius B, Kahn K, Collinson MA, Sartorius K, Tollman SM. Dying in their prime: determinants and space-time risk of adult mortality in rural South Africa. Geospatial Health. 2013; 7: 237. [PubMed Abstract] [PubMed CentralFull Text].
- Sartorius B, Kahn K, Collinson MA, Vounatsou P, Tollman SM. Survived infancy but still vulnerable: spatial-temporal trends and risk factors for child mortality in rural South Africa (Agincourt), 1992–2007. Geospatial Health. 2011; 5: 285. [PubMed Abstract] [PubMed CentralFull Text].
- Sartorius B, Kahn K, Vounatsou P, Collinson MA, Tollman SM. Space and time clustering of mortality in rural South Africa (Agincourt HDSS), 1992–2007. Glob Health Action. 2010; 3 http://dx.doi.org/10.3402/gha.v3i0.522 .
- Sartorius BK, Kahn K, Vounatsou P, Collinson MA, Tollman SM. Young and vulnerable: Spatial-temporal trends and risk factors for infant mortality in rural South Africa (Agincourt), 1992–2007. BMC Public Health. 2010; 10: 645. [PubMed Abstract] [PubMed CentralFull Text].
- Sartorius K, Sartorius B, Tollman S, Schatz E, Kirsten J, Collinson M. Rural poverty dynamics and refugee communities in South Africa: a spatial-temporal model. Popul Space Place. 2013; 19: 103–23. [PubMed Abstract] [PubMed CentralFull Text].
- Tollman SM. The Agincourt field site: evolution and current status. S Afr Med J. 1999; 89: 853–8. [PubMed Abstract].
- Tollman SM, Herbst K, Garenne M, Gear J, Kahn K. The Agincourt demographic and health study-site description, baseline findings and implications. S Afr Med J. 1999; 89: 858–64. [PubMed Abstract].
- Kahn K, Tollman SM, Garenne M, Gear JS. Who dies from what? Determining cause of death in South Africa's rural north-east. Trop Med Int Health. 1999; 4: 433–41. [PubMed Abstract].
- Garenne M, Kahn K, Tollman S, Gear J. News from the regions. Causes of death in a rural area of South Africa: an international perspective. J Trop Pediatr. 2000; 46: 183–90. [PubMed Abstract].
- Kahn K, Tollman SM, Garenne M, Gear JS. Validation and application of verbal autopsies in a rural area of South Africa. Trop Med Int Health. 2000; 5: 824–31. [PubMed Abstract].
- Kahn K, Tollman SM, Collinson MA, Clark SJ, Twine R, Clark BD, etal. Research into health, population and social transitions in rural South Africa: data and methods of the Agincourt Health and Demographic Surveillance System. Scand J Publ Health. 2007; 35(Suppl 69): 8–20.
- Byass P, Kahn K, Fottrell E, Collinson MA, Tollman SM. Moving from data on deaths to public health policy in Agincourt, South Africa: approaches to analysing and understanding verbal autopsy findings. PLoS Med. 2010; 7: e1000325. [PubMed Abstract] [PubMed CentralFull Text].
- Fottrell E, Kahn K, Ng N, Sartorius B, Huong DL, Van Minh H, etal. Mortality measurement in transition: proof of principle for standardised multi-country comparisons. Trop Med Int Health. 2010; 15: 1256–65. [PubMed Abstract] [PubMed CentralFull Text].
- Byass P, Kahn K, Fottrell E, Mee P, Collinson MA, Tollman SM. Using verbal autopsy to track epidemic dynamics: the case of HIV-related mortality in South Africa. Popul Health Metr. 2011; 9: 46. [PubMed Abstract] [PubMed CentralFull Text].
- Byass P, Chandramohan D, Clark SJ, D'Ambruoso L, Fottrell E, Graham WJ. Strengthening standardised interpretation of verbal autopsy data: the new InterVA-4 tool. Glob Health Action. 2012; 5: 19281. http://dx.doi.org/10.3402/gha.v5i0.19281 .
- Leitao J, Chandramohan D, Byass P, Jakob R, Bundhamcharoen K, etal. Revising the WHO verbal autopsy instrument to facilitate routine cause-of-death monitoring. Glob Health Action. 2013; 6: 21518. http://dx.doi.org/10.3402/gha.v6i0.21518 .
- Bird J, Byass P, Kahn K, Mee P, Fottrell E. A matter of life and death: practical and ethical constraints in the development of a mobile verbal autopsy tool. 2013; New York: ACM. 1489–98,Proceedings of the SIGCHI Conference on Human Factors in Computing Systems.
- Byass P, Calvert C, Miiro-Nakiyingi J, Lutalo T, Michael D, Crampin A. InterVA-4 as a public health tool for measuring HIV/AIDS mortality: a validation study from five African countries. Glob Health Action. 2013; 6: 22448. http://dx.doi.org/10.3402/gha.v6i0.22448 [PubMed Abstract].
- INDEPTH Network. INDEPTH Network Cause-Specific Mortality – Release 2014. Oct 2014. Provided by the INDEPTH Network Data Repository. www.indepth-network.org. doi: 10.7796/INDEPTH.GH003.COD2014.v1.
- Sankoh O, Sharrow D, Herbst K, Kabudula CW, Alam N, Kant S. The INDEPTH standard population for low-and middle-income countries, 2013. Glob Health Action. 2014; 7: 23286. http://dx.doi.org/10.3402/gha.v7.23286 [PubMed Abstract].
- World Health Organization. Verbal autopsy standards: the 2012 WHO verbal autopsy instrument. 2012; Geneva: WHO. Available from: http://www.who.int/healthinfo/statistics/WHO_VA_2012_RC1_Instrument.pdf [cited 26 September 2014]..
- INDEPTH Network Cause-Specific Mortality Writing Group. Adult non-communicable disease mortality in Africa and Asia: evidence from INDEPTH Health and Demographic Surveillance System sites. Glob Health Action. 2014; 7: 25365. http://dx.doi.org/10.3402/gha.v7.25365 .
- Patton GC, Coffey C, Sawyer SM, Viner RM, Haller DM, Bose K, etal. Global patterns of mortality in young people: a systematic analysis of population health data. Lancet. 2009; 374: 881–92. [PubMed Abstract].
- Ferrand RA, Bandason T, Musvaire P, Larke N, Nathoo K, Mujuru H, etal. Causes of acute hospitalization in adolescence: burden and spectrum of HIV-related morbidity in a country with an early-onset and severe HIV epidemic: a prospective survey. PLoS Med. 2010; 7: e1000178. [PubMed Abstract] [PubMed CentralFull Text].
- Bradshaw D, Groenewald P, Laubscher R, Nannan N, Nojilana B, Norman R, etal. Initial burden of disease estimates for South Africa, 2000. S Afr Med J. 2003; 93: 682–8. [PubMed Abstract].
- Groenewald P, Bradshaw D, Daniels J, Zinyakatira N, Matzopoulos R, Bourne D, etal. Local-level mortality surveillance in resource-limited settings: a case study of Cape Town highlights disparities in health. Bull World Health Organ. 2010; 88: 444–51. [PubMed Abstract] [PubMed CentralFull Text].
- Herbst AJ, Mafojane T, Newell ML, others. Verbal autopsy-based cause-specific mortality trends in rural KwaZulu-Natal, South Africa, 2000–2009. Popul Health Metr. 2011; 9: 47. [PubMed Abstract] [PubMed CentralFull Text].
- Hosegood V, Vanneste AM, Timæus IM. Levels and causes of adult mortality in rural South Africa: the impact of AIDS. AIDS. 2004; 18: 663. [PubMed Abstract].