Abstract
Background
Antibiotics are considered among the most commonly prescribed drug classes in developing countries. Inappropriate prescription of antibiotics is a major public health concern and is related to the development of antimicrobial resistance.
Objective
This study aimed at assessing the appropriateness of antibiotic prescription by non-infectious disease physicians in a community setting in Lebanon.
Methods
A pilot cross-sectional study was undertaken on community pharmacy patients presenting with antibiotic prescription. It was performed over a period of 4 months in different regions of Lebanon. Participants answered a questionnaire inquiring about socio-demographic characteristics, medical conditions, symptoms that required medical attention, the doctor's diagnosis, the prescribed antibiotic, and whether laboratory tests were ordered to identify the causative organism or not. Data were analyzed using SPSS 17.
Results
We studied 270 patients (49.3% males and 50.7% females). This study showed that the most-prescribed antibiotics were the cephalosporins (82%) and that almost half of the illnesses for which antibiotics were prescribed were respiratory tract infections (41%). The study also showed that the choice of the prescribed antibiotic was appropriate in 61.5% of the studied cases, while the prescribed dose and the duration of the treatment were inaccurate in 52 and 64% of the cases, respectively. In addition, fever seemed to be a factor that influenced the physician's prescriptions, since the choice of drug conformity to guidelines increased from 53.7% (1 day of fever) to 88.9% (1 week of fever), and the dose prescription compliance to guidelines was higher (55.9%) for patients suffering from fever compared to those with no fever (38.1%).
Conclusion
This study showed a high prevalence of inappropriate antibiotic prescriptions in Lebanon. Therefore, actions should be taken to optimize antibiotic prescription.
Antibiotics are considered among the most commonly sold drug classes in developing countries (Citation1). The irrational use and overuse of antibiotics are a major public health concern nowadays; although this problem cannot be prevented, its prevalence can be decreased (Citation2). Irrational use may involve several practices such as prescribing injections where oral prescriptions are available, inadequate dosage or use of unnecessary number of medications, a shorter or longer than necessary duration of use, use of antimicrobials for non-bacterial infection, and the choice of higher cost over lower cost therapeutic options (Citation3).
The misuse of antibiotics results not only in the emergence of resistant bacterial strains but also in adverse reactions and economic burden on national health systems (Citation4). This irrational use arises from economic factors, health policies concerning medical insurance, lack of physicians’ concern about long-term resistance and effect while treating current symptoms, pharmaceutical marketing, and the sale of antibiotics without prescription in some countries (Citation5, Citation6).
To tackle inadequate antibiotic use and its subsequent bacterial resistance, the World Health Organization proposed, among numerous interventions, that prescribers adopt and use protocols or guidelines based on strong evidence for the use of antibiotics for community infections (Citation7). Adopting these guidelines would standardize treatments, minimize dosage mistakes, avoid individual decisions, and prioritize decisions based on clinical evidence (Citation8). Recent studies showed that not adopting guidelines has led to antibiotic prescription mistakes in terms of dose or duration (Citation9, Citation10).
In Lebanon, the healthcare system depends mainly on the private sector; although 42% of antibiotics sold in the pharmacy are delivered without prescription, 58% are, however, prescribed by physicians (Citation11). Detailed information on antibiotic drug prescribing in the community setting is scarce. Thus, the objective of the present study was to assess the prescribing practices of non-infectious disease practitioners in the community, checking the appropriateness of antibiotic prescription in terms of antibiotic choice, dose, and duration of treatment.
Materials and methods
Population and data collection
A pilot cross-sectional survey was conducted on community pharmacy patients. The study was carried out over a period of 4 months, between May and August 2014. The study was conducted in 18 pharmacies, located as follows: 9 in the South of Lebanon, 2 in Mount Lebanon, 2 in the North, and 5 in Beirut and its suburbs. The pharmacy locations were chosen by convenience, while the included patients were all patients fulfilling inclusion criteria. Thus, all patients of different ages and of both sexes who presented to community pharmacies with an antibiotic prescription were included in this study; patients who bought antibiotics with a prescription by infectious disease specialists, without prescription or with non-antibiotic prescriptions were excluded. A total of 270 patients were interviewed.
The Lebanese University, Faculty of Pharmacy Internal Review Board waived the need for a written informed consent since patients were only interviewed once, with no further traceability or follow-up.
Tools and procedures
The working pharmacist within the community pharmacy interviewed participants. They gave verbal informed consent to participate in the study and were assured about the anonymity of questionnaires. Data were recorded about the patient for whom the prescription belonged: proxy responding by parents was only permitted in case the patients were children. Individuals were informed about the objective of the study, that is, to study the trends of physician's antibiotic prescribing and to check if they were compliant to the guidelines; for this purpose, the Infectious Disease Society of America (IDSA) guidelines were used (Citation12). Because of the absence of Lebanese guidelines, the IDSA guidelines are generally taught during medical education in Lebanon and are deemed to be the most important guidelines on an international level.
A standardized questionnaire, specifically designed for the study and written in Arabic, was used. It inquired about the following characteristics: socio-demographic characteristics, medical conditions, symptoms that required medical attention, the doctor's diagnosis, the medication prescription details (name, dose, duration, mode of administration, as written on the prescription), and whether laboratory tests were ordered to identify the causative organism. The details permitted to assess the choice of drug appropriateness (if it was considered so by guidelines), and the dose and duration of treatment adequacy. Physicians’ specialty was also recorded: non-specialists’ (general and family physicians) versus non-infectious disease specialists’ (pulmonologists, gastroenterologists, nephrologists, etc.) prescriptions were compared.
Statistical analysis
Data were entered and analyzed using the statistical software SPSS (Statistical Package for Social Sciences), version 17. A P<0.05 was considered significant. Descriptive statistics, mainly proportions, were used for discrete variables. The chi-square test was used to compare qualitative variables.
Results
Study population characteristics
Data from a total of 270 patients were recorded, 133 males (49.3%) and 137 females (50.7%). Individuals from all age groups were included, the majority being between 21 and 50 years of age (52.6%), while 19.6% were aged 1–11 years, 13.3% were 12–21 years, and 12.6% were ≥51 years of age. The majority of the participants was from the South (44.1%), followed by Mount Lebanon (26.3%), North (18.9%), Beirut (8.9%), and finally Bekaa (1.1%). A high percentage had a university degree (32.2%), while 24.1% had secondary education, 11.5% had intermediate education, and 13.7% had elementary education.
A total of 240 patients (88.4%) had no associated medical conditions, while 18 (6.6%) suffered from chronic diseases, among which 2.6% had hypertension, 1.3% had asthma, 0.7% had renal failure, and 0.4% for both diabetes and COPD. Twelve participants (4.4%) were pregnant and one (0.4%) had an allergy to penicillin.
In addition, the highest percentage (112; 41%) presented with a respiratory tract infection (RTI; mainly pharyngitis and acute bronchitis), followed by 37 (14%) who suffered from urinary tract infections (uncomplicated cystitis), 31 (11%) had gastrointestinal infections (diarrhea), 26 (10%) had oral infections, 11 (4%) had skin and soft tissue infections, 6 (2%) suffered from post-operation wound infections, and 5 (2%) had infections in the reproductive system. However, 42 (16%) were unable to identify the disease that they were suffering from and the physician did not mention the diagnosis on the prescription ().
Table 1 Characteristics of the study population
Antibiotic choice and diagnosis
The most-prescribed antibiotic families were the cephalosporins 87 (32%) (mainly cefixime, an oral third-generation cephalosporin), followed by penicillins [82 (30.6%), amoxicillin–clavulanic acid fixed-dose combination], and quinolones 55 (20%; equally divided into levofloxacin and ciprofloxacin). The least-prescribed antibiotics were lincosamides 5 (2%), tetracyclines 2 (0.7%), and rifaximin 2 (0.7%) ( and Table A.1).
Table 2 List of prescribed antibiotics
Conformity to guidelines
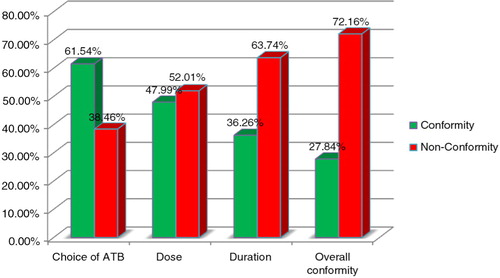
Our study has shown that 61.54% of doctors have prescribed the right antibiotic against 38.46% (95% CI 32.66; 44.26) of doctors who failed to do so. In the majority of the studied cases, the dose prescribed was inappropriate (52.01%) (95% CI 46.05; 57.97), and so was the duration of treatment, where 63.74% (95% CI 58.01; 69.47) of doctors did not prescribe the antibiotic for the right duration. When all of the aforementioned factors were summed together, it turned out that 72.16% of antibiotic prescriptions (95% CI 69.43; 74.89) did not adhere to guidelines ().
Fig. 1. Percentages of conformity and non-conformity of antibiotic choice, dose, duration of treatment, and global conformity to Infectious Diseases Society of America guidelines.
As shown in Table A.2, the following factors have not shown a difference that is statistically significant in terms of choice of drug conformity: doctor specialty, gender, residence, level of education, presence of fever, persistence of fever, and laboratory tests. Age category showed a statistically significant difference in conformity to guidelines (P=0.035): children aged 1–11 had the least adequate prescriptions (52.8% conformity) versus others. Fever persistence has also shown statistically a significant increase from 53.7% (1 day of fever) to 88.9% (1 week of fever; p=0.012).
While studying the dose prescribed and its conformity to the IDSA guidelines, the gender of patients and the presence of fever showed a difference that was statistically significant (p=0.002). The dose was compliant to the guidelines in 57.9% of the males, while it was 39.4% in females. The dose compliance to the guidelines was higher (55.9%) for patients suffering from fever compared to those with no fever (38.1%) (Table A.3). None of the studied factors have shown a difference that was statistically significant with respect to antibiotic duration (P>0.05 for all; Table A.4). Our study did not show any statistically significant difference with respect to overall conformity (p>0.05 for all; Table A.5).
Discussion
In this pilot study, we found that antibiotic prescription was not conforming to the IDSA guidelines in the majority of cases. High rates of non-conformity to guidelines in the prescribed antibiotics concerning dosage (52%) and duration of therapy (62%) were also found. This could be explained by several factors, such as the lack of simple and clear recommendations for the dose and treatment duration, the lack of clinical trials to assess the optimal treatment duration, variability in medical knowledge, and psychosocial factors involved in medical decision making (Citation13, Citation14).
In addition, the results of our study showed that almost half of the prescribed antibiotics (49%) were used to treat RTI. These findings are consistent with the results from other studies conducted in Turkey, Sweden, and India showing that antibiotics were mostly prescribed for RTI (Citation15–Citation17). Interestingly, the diseases treated most frequently among the RTIs were pharyngitis and acute bronchitis. These infections are usually caused by viruses and in most of the cases are self-limited. Data from numerous studies showed that antibacterial agents do not significantly shorten the duration of illness in acute bronchitis (Citation18).
As for pharyngitis, approximately 30–40% of cases in children are bacterial (Citation19) and thus necessitate antibiotic treatment. When trying to establish the causative agent as viral or bacterial, age appears to be the most helpful factor: viral pharyngitis is more common in children younger than 3 years, while group A beta-hemolytic streptococcus (GABHS) pharyngitis is more common in children aged 6 years or older (Citation20). In our study, among patients diagnosed with pharyngitis (34 cases), the majority [65% (22 cases)] were either adults [41% (14 cases)] or lower than 3 years of age [24% (8 cases)]. A bacterial infection with GABHS in these age groups is thus uncommon. Despite this fact, antibiotic therapy was prescribed for these patients without ruling out the possibility of a viral infection which is more common in their case. These are important findings, because inappropriate antibiotic use for upper respiratory infections has contributed to the rising incidence of antimicrobial resistance (Citation21).
We also found that the choice of prescribed drug was more compliant to the guidelines when fever has persisted for more than 1 week (88.9%), which may be explained by the presence of a severe case that necessitates a thorough follow-up. Also, the dose that was prescribed by the physician seemed to adhere more to guidelines in patients suffering from fever (55.9%), a fact that can be explained by doctors considering the fever as an indicator of a serious infection and therefore taking time to treat such patients. These results are consistent with a study done in nine countries in Europe, where clinicians reported that fever had an influence on their decision to prescribe antibiotics (Citation22).
This study has several limitations that merit discussion. This was a pilot study performed on a limited number of participants, due to the small time frame (4 months) used to conduct it; thus, it may not represent the Lebanese population. The low number of patients could also explain non-significant results. The study was also done in the summer period in which there is a normal decline in antibiotic prescription. Further studies with bigger sample size and time frame should be done to thoroughly assess the trends of antibiotic prescription in the outpatient setting in Lebanon. Although the pharmacy locations were chosen by convenience, the included patients were all patients fulfilling inclusion criteria, which may decrease the selection bias. In addition, the diagnoses mentioned in this study were written on the prescription or given by patients; in the latter case, inaccurate diagnosis is possible although infection symptoms are generally clearly identified; in case of missing diagnosis, this problem would be greater. Finally, the study was done in community pharmacies. We suggest conducting similar studies at the doctors’ offices in which information such as the age and gender of doctors, the medical academic institutions from which they graduated, and their practicing location can be determined.
Despite these limitations, the key results of this study would form the basis for future interventional directions to improve antibiotic prescription in Lebanon. Optimizing antibiotic use is a challenge that deserves to be undertaken, thus efforts should be made to rationalize and change antibiotic prescription in Lebanon. To achieve this, we suggest a number of steps, including the following: implementing local guidelines for selecting optimal drug concerning spectrum of activity and side effects, using optimal dose and optimal treatment duration, determining patients requiring antibiotic prescription, implementing stewardship programs to reduce inappropriate antibiotic prescribing among practicing physicians, and implementing undergraduate courses that directly address bacterial resistance causes and consequences. Adopting consensual marketing policies to control antibiotic promotion to prescribers is also of utmost importance.
Conclusion
In conclusion, non-conformity to guidelines is common among prescriptions in Lebanon, regardless of doctors’ specialty. Additional studies are needed to have a more precise idea about the extent of the problem.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
Acknowledgements
We thank the Lebanese University and the community pharmacists where the study took place.
References
- Cagri Buke A, Ermertcan S, Hosgor-Limoncu M, Ciceklioglu M, Eren S. Rational antibiotic use and academic staff. Int J Antimicrob Agents. 2003; 21: 63–6.
- Gould IM. Antibiotic resistance: the perfect storm. Int J Antimicrob Agents. 2009; 34: 52–5.
- World Health Organization. The world medicines situation. 2011. Available from: http://www.who.int/medicines/areas/policy/world_medicines_situation/en/ [cited April 2015]..
- Gyssens IC. Quality measures of antimicrobial drug use. Int J Antimicrob Agents. 2001; 17: 9.
- McManus P, Hammond ML, Whicker SD, Primrose JG, Mant A, Fairall SR. Antibiotic use in the Australian community, 1990–1995. Med J Aust. 1997; 167: 124–7.
- Metlay JP, Stafford RS, Singer DE. National trends in the use of antibiotics by primary care physicians for adult patients with cough. Arch Intern Med. 1998; 158: 1813–18.
- World Health Organization. Global strategy for containment of antimicrobial resistance. 2012. Available from: http://www.who.int/csr/resources/publications/drugresist/en/EGlobal_Strat.pdf [cited April 2015]..
- McCaig LF, Hughes JM. Trends in antimicrobial drug prescribing among office-based physicians in the United States. JAMA. 1995; 273: 214–19.
- Del Fiol Fde S, Lopes LC, Toledo MI, Barberato-Filho S. Prescription patterns and antibiotic use in community-based infections. Rev Soc Bras Med Trop. 2010; 43: 68–72.
- Porta A, Esposito S, Menson E, Spyridis N, Tsolia M, Sharland M, etal. Off-label antibiotic use in children in three European countries. Eur J Clin Pharmacol. 2010; 66: 919–27.
- Cheaito L, Azizi S, Saleh N, Salameh P. Assessment of self-medication in population buying antibiotics in pharmacies: a pilot study from Beirut and its suburbs. Int J Public Health. 2014; 59: 319–27.
- Infectious Disease Society of America. Infections by organ system. Available from: http://www.idsociety.org/Organ_System/ [cited April 2015]..
- Howie J, Bigg A. Family trends in psychotropic and antibiotic prescribing in general practice. Br Med J. 1980; 280: 836–38.
- Howie JG. Clinical judgment and antibiotic use in general practice. Br Med J. 1976; 2: 1061–4.
- Aydin S, Yaris F, Ozcakir A, Agalar C. Most common infections and antibiotic prescribing habits of residents: experience of three university hospitals. Turk J Med Sci. 2005; 35: 169–73.
- Lundborg CS, Olsson E, Mölstad S, Swedish Study Group on Antibiotic Use . Antibiotic prescribing in outpatients: a 1-week diagnosis-prescribing study in 5 counties in Sweden. Scand J Infect Dis. 2002; 34: 442–8.
- Pathak A, Mahadik K, Dhaneria SP, Sharma A, Eriksson B, Lundborg CS. Antibiotic prescribing in outpatients: hospital and seasonal variations in Ujjain, India. Scand J Infect Dis. 2011; 43: 479–88.
- Fahey T, Stocks N, Thomas T. Quantitative systematic review of randomised controlled trials comparing antibiotic with placebo for acute cough in adults. BMJ. 1998; 316: 906–10.
- Pichichero ME. Group A streptococcal tonsillopharyngitis: cost-effective diagnosis and treatment. Ann Emerg Med. 1995; 25: 390–403.
- Putto A. Febrile exudative pharyngitis: viral or streptococcal?. Pediatrics. 1987; 80: 6–12.
- McCaig LF, Besser RE, Hughes JM. Trends in antimicrobial prescribing rates for children and adolescents. JAMA. 2002; 286: 3096–102.
- Brookes-Howell L, Hood K, Cooper L, Coenen S, Little P, Verheij T, etal. Clinical influences on antibiotic prescribing decisions for lower respiratory tract infection: a nine country qualitative study of variation in care. BMJ Open. 2012; 2: 000795–e000795. doi: 10.1136/bmjopen-2011-000795.
Appendix
Table A.1. Antibiotics prescribed and their corresponding diagnostics
Table A.2. Choice of drug conformity to guidelines
Table A.3. Dose conformity to guidelines
Table A.4. Conformity of the duration of the antibiotic course to guidelines
Table A.5. Global conformity to guidelines
