Abstract
Background : Population health data are vital for the identification of public health problems and the development of public health strategies. Challenges arise when attempts are made to disseminate or access anonymised data that are deemed to be potentially identifiable. In these situations, there is debate about whether the protection of an individual's privacy outweighs potentially beneficial public health initiatives developed using potentially identifiable information. While these issues have an impact at planning and policy levels, they pose a particular dilemma when attempting to examine and address community concerns about a specific health problem.
Methods : Research currently underway in northern Canadian communities on the frequency of Helicobacter pylori infection and associated diseases, such as stomach cancer, is used in this article to illustrate the challenges that data controls create on the ability of researchers and health officials to address community concerns.
Results : Barriers are faced by public health professionals and researchers when endeavouring to address community concerns; specifically, provincial cancer surveillance departments and community-driven participatory research groups face challenges related to data release or access that inhibit their ability to effectively address community enquiries. The resulting consequences include a limited ability to address misinformation or to alleviate concerns when dealing with health problems in small communities.
Conclusions : The development of communication tools and building of trusting relationships are essential components of a successful investigation into community health concerns. It may also be important to consider that public wellbeing may outweigh the value of individual privacy in these situations. As such, a re-evaluation of data disclosure policies that are applicable in these circumstances should be considered.
Community members regularly express concerns about perceived health threats, such as apparent higher rates of cancer in their community. In the United States alone, over 1,000 cancer cluster investigation requests are made annually to health authorities Citation1. Concerns about specific local health problems may also be reported to health practitioners, community champions, researchers, or the media. Once reported, health officials or researchers often undertake an investigative process to answer questions and address concerns Citation2 Citation3. Through these examinations, investigators aim to determine whether there is evidence of an excessive rate of the perceived health problem and to establish if further investigation is required and feasible. These investigations involve both analytical and communication components: both are essential to effectively address community concerns.
Analyses are conducted that compare the frequency of disease in the concerned community to that of a reference population in another geographic area. These calculations may involve a comparison of community disease rates to those observed elsewhere, or a comparison of the number of disease outcomes observed in the community to the number of outcomes expected based on rates in a reference population. While analytical assessment provides evidence about whether there is a higher-than-expected number of outcomes, other aspects of the investigation are also vital to the success of the investigation. These include the building of relationships and the maintenance of open and bi-directional communication Citation4–Citation6. It has been noted that successful investigations require an on-going collaborative relationship with the local community at the beginning stages of the investigation, and that the process and results must be transparent Citation7 Citation8.
Many challenges arise when attempting to undergo such investigations. This article describes one of the challenges faced by investigators when attempting to address community concerns about a particular health problem; specifically, the obstacles created by data disclosure and data access restrictions. To illustrate these issues, we present a case study highlighting work done in northern Canada to address community concerns related to the frequency of Helicobacter pylori infection and stomach cancer. Also discussed are the consequences of data controls in such investigations and potential solutions that may reduce future challenges when addressing community concerns.
Obstacles
There are a variety of challenges that arise when undergoing investigations to address community concerns about a specific health problem. These include methodological issues, as well as problems resulting from miscommunication between investigators and concerned community members Citation4 Citation9. Conducting the analyses required in these investigations can be difficult, particularly when investigations occur in small communities such as those located in the northern regions of Canada. These methodological issues may include an inability to capture cases of disease observed in people who have moved away from the community and were diagnosed elsewhere, or incomplete historical data for analytic purposes Citation10. Additionally, drawing conclusions from analytic results can be difficult. In many cases, a small number of outcomes within the community yields results with low statistical power, making results difficult to interpret and inhibiting the assessment of trends over time Citation11.
Other barriers to a successful investigation include fundamental differences between the questions posed by the concerned community and those answered by investigators: community members may know there is a problem and want to understand its cause, while investigators first attempt to determine if there is a problem. These misaligned perceptions can be exacerbated by other challenges with communication of the investigation results. Community members may differ on how they interpret scientific facts Citation12 and cross-cultural differences in research interpretation Citation13 may prevent a common conclusion about the meaning of the synthesized results. Furthermore, community members may differ in their perceptions of what constitutes a higher than expected number of disease outcomes and may be more likely to perceive a need for an in-depth investigation Citation12.
Another obstacle to the effective dissemination of investigation results is the inability of investigators to share some of the findings with community members due to data release controls Citation14 Citation15. Concerns over confidentiality infringements prevent the release of identifiable data such as name, date of birth, and health care number by health officials and other custodians of health-related data. The importance of privacy has been widely acknowledged; Myers et al. stated that, “As a society, we place great value on individual rights and uphold the importance of protecting personal information…” Citation16. Nass et al. stated that privacy is, “an essential component of human well-being,” and highlighted that privacy is valuable because it promotes ideals such as “personal autonomy, individuality, respect, and dignity and worth as human beings” Citation17. The importance of privacy has also been emphasized by the fact that release of individual health information may result in embarrassment, stigma, or discrimination Citation16 Citation18.
Data release restrictions designed to maintain confidentiality are not limited to overtly identifiable data; anonymised data may also be considered potentially identifiable and, therefore, withheld to uphold the privacy of an individual. This can occur when there are a small number of outcomes in a small population. In such situations, if cases are characterized by a small number of factors such as age and year of diagnosis, it may be possible for the identity of the individual to be inferred. The exact rules and regulations around what constitutes “small” varies by agency, political region, disease, and investigative situation. Typically, fewer than 5 outcomes are suppressed to prevent the release of information on potentially identifiable cases Citation14. For example, 2 cases of stomach cancer in a community of 1,000 people would be reported as fewer than 5 cases. These restrictions limit the amount of information that custodians of the data, such as cancer registries, are permitted to share with community members. Data controls also prevent the release of useful information to researchers who are conducting community-driven work in attempt to address concerns.
Case study: Aklavik H. pylori project
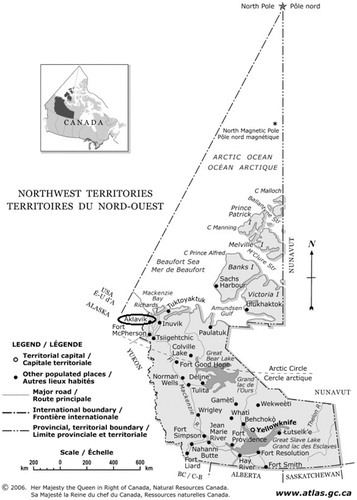
The hamlet of Aklavik is a remote community located on the Peel Channel of the Mackenzie River Delta in the Northwest Territories (NWT), Canada (). The community has a population of approximately 600 and is made up of primarily Gwich'in First Nations and Inuvialuit peoples; in the 2006 Canadian Census, 92% of Aklavik residents self-identified as Aboriginal Citation19. Throughout several years preceding 2006, Aklavik residents voiced concerns to local health professionals about a perceived increase in the number of stomach cancer cases diagnosed in the community. Many residents believed that this occurred due to a high frequency of H. pylori, a bacterium known to be a risk factor for stomach cancer. While the prevalence of H. pylori has decreased in developed countries, research suggests that northern Aboriginal populations have a disproportionately high prevalence of H. pylori infection and an increased frequency of H. pylori-associated diseases Citation20.
Fig. 1. Map of the Northwest Territories, Canada. Aklavik circled by authors (modified from The Atlas of Canada: Northwest Territories, Natural Resources Canada) Citation21
In response to community concerns, the Canadian North Helicobacter pylori (CANHelp) Working Group was formed in 2006. The CANHelp Working Group is a collaborative research initiative that links community representatives, faculty from various disciplines at the University of Alberta in Canada, as well as Northwest Territories and Yukon health care practitioners and health authorities. The overall aims of the research program are to describe the burden of disease and risk factors associated with H. pylori infection, and to identify effective public health strategies for infection control Citation22. Although originating in Aklavik, other communities in the NWT and Yukon Territory have since expressed interest in participating in this research; projects have been initiated in Old Crow, Yukon and Tuktoyaktuk, NWT. In each community, a planning committee comprising community representatives, researchers, and health professionals helps guide the research so that the work done is aligned with community priorities and interests.
Challenges have arisen when attempting to specifically address concerns over the perceived excess of stomach cancer cases. Unsubstantiated numbers of stomach cancer cases have been reported to and disseminated by the media, along with assertions of increased stomach cancer incidence. For example, the Edmonton Journal has reported that, “Between 1992 and 2000, the Northwest Territories government recorded 27 cases of stomach cancer, of which 8 were centred in Aklavik” Citation23, thus making the highly improbable attribution of 30% of the territory's stomach cancer cases to less than 1.5% of its population. Reader's Digest has stated that, “[Aklavik] has had exceptionally high stomach-cancer rates for years – men here develop it at about 3 times the national average” Citation24, applying a statistic reported for the territory's regional centres to one community for which no such statistics are estimated Citation25. Another popular news source has also reported that, “Residents have long suspected that a high number of H. pylori infections may explain why so many of their family members and other residents have died from stomach cancer. Exact numbers are not known, but 1 local family is said to have lost 5 relatives to the disease” Citation26.
Due to data disclosure restrictions, the territorial cancer registry has been unable to release information on the actual number of stomach cancer cases diagnosed in the community over recent time periods to clarify unsubstantiated information. This inhibits the research team from giving the community needed region-specific information to put their risk of stomach cancer in perspective. Furthermore, comparisons between the incidence of stomach cancer within northern communities expressing concern and incidence observed in other parts of Canada have not been possible. Attempts to address questions and concerns about cancer in the community, therefore, have had to be done indirectly; researchers have provided community members with broad educational information on H. pylori and what is known about the risk of developing stomach cancer. Unfortunately, without being able to directly address community-specific stomach cancer risk, anxiety over a perceived excess of cancer cases in the community persists.
Consequences
Data disclosure and data release restrictions inhibit the ability of investigators to effectively address community concerns. Data custodians, such as cancer registries or health surveillance departments, are unable to release to community members, or to researchers, data that are considered to be potentially identifiable. These data release restrictions hinder the ability of researchers to compare disease rates within a concerned community to disease rates in other reference populations, thereby preventing the assessment of disease risk associated with living in the area. Consequently, researchers are not able to gain perspective on the community health issue relative to other areas of Canada and are limited in their ability to undertake public health research Citation27, such as etiologic studies that would be warranted if an elevated disease frequency were documented.
In situations where analyses are feasible, data release controls prevent investigators from adequately communicating investigation results to community members, a vital component of the investigative process. Data controls prevent the release of certain investigation findings, which creates problems when investigators attempt to describe the results to community members and explain how the findings may be interpreted. For example, investigators may be able to explain that there is no evidence of higher rates of disease in the community compared to rates observed in other populations, but are unable to share how many cases have actually been observed. Community members may feel that they have been left out of the investigative process by not being allowed to evaluate the results for themselves. Because a sense of inclusion in the investigative process by the community is necessary for acceptance of the investigation results Citation28, these restrictions therefore also create issues when discussing next steps. These communication challenges are exacerbated by the potential perception that the investigation lacks transparency. Because a transparent process is essential to the success of these investigations Citation7, the perceived absence of this transparency limits trust in the investigative process, the acquired results, and the conclusions drawn. Furthermore, withholding information makes it difficult to maintain trusting relationships that are essential to the success of investigations into health problems in communities Citation29.
Because of data disclosure restrictions, opportunities to decrease anxiety in the community are missed; misinformation or unsubstantiated information cannot be corrected, thereby perpetuating anxiety over the perceived health threat. In addition, without directly addressing concerns over the specific health problem, resources may be wasted or misaligned. Money, time, and energy may be spent on addressing specific concerns at the expense of other community health and social issues. Without the ability of data custodians to share data that are considered to be potentially identifiable, and without data access for researchers, investigative teams are unable to adequately address community concerns.
Solutions
Investigations that attempt to address community concerns about a specific health problem are filled with a variety of challenges. These challenges include data disclosure and data access restrictions that inhibit the ability of investigators to disseminate information to community members. This may be overcome through the development of risk communication and knowledge translation tools, acknowledgement of the importance of relationship-building, and a re-evaluation of data disclosure policies.
The development of risk communication strategies and knowledge translation tools that are specific to health investigations initiated through community concern will support communication between investigators and community members throughout the investigative process. Enhancing effective communication will foster a mutual understanding of one another's perceptions and ultimately help to build strong relationships that are vital to the success of these investigations. This may involve an assessment of the prevalence and degree of concern amongst community members Citation30, and whether a common language is used when discussing investigation components Citation4 Citation9. The identification and development of effective communication tools can also support increased knowledge amongst all investigation participants about the research methods, results, and interpretation, thereby enhancing understanding of the investigative process and the limitations imposed by data restrictions Citation8. For example, an evaluation of which communication medium, such as community presentations or newsletters, would best facilitate discussions amongst investigation participants could help to foster participation and enhance successful communication Citation7 Citation28. Furthermore, knowledge translation tools may provide insights into how the results of these investigations can be effectively communicated in a way that is meaningful to community members and decision-makers.
Another way that these investigations can be supported is through investment in trust and bi-directional relationship-building. Relationship- and trust-development between investigators and community members will increase the likelihood that these investigations will be considered successful Citation6 Citation28 Citation29 Citation31. Because of large distances between remote communities and research centres, particularly in the northern regions of Canada, communication is often accomplished over email or by telephone. It should be noted, however, that successful relationship-building takes time, and that the development and maintenance of trust in community-based work is typically more successful and fulfilling when done in person Citation6 Citation31 Citation32. As such, researchers conducting work to address community concerns should allow for multiple in-person discussions when planning and budgeting for these research initiatives. Funding agencies that support these researchers should also recognize the necessity of strong relationships to the success of community-driven work, as well as the resources required to support these initiatives. Likewise, resource support from government agencies that employ health professionals who take part in these investigations is necessary to promote the development of meaningful relationships.
While the development of communication tools and trusting relationships are essential components to the success of investigations into community health concerns, they do not deal directly with the challenges posed by data disclosure controls. These data restrictions are in place to protect the right of individuals to privacy and apply to both directly identifiable data and anonymised data that are considered to be potentially identifiable. In situations where there is extreme community alarm over a perceived health threat, it may be important to consider that these data are only potentially identifiable, and that public wellbeing may outweigh the value of individual privacy. In these circumstances, exceptions to data release restrictions should be considered; that is, data custodians should consider releasing potentially identifiable and anonymised data to promote effective and direct communication with concerned community members, and to facilitate the ability of researchers to directly evaluate community risk in these circumstances. If applicable, data custodians might also consider contacting individuals who may be impacted by the public release of these anonymised data. As Bayer and Fairchild stated, “…there are occasions when those whose privacy will be compromised view [data sharing] not as a burden but as serving their interests” Citation33. If these individuals are members of a concerned community, they may encourage the public release of anonymised data to support community goals, despite the potential breach of their privacy.
In summary, challenges created by data disclosure and data access restrictions inhibit the ability of investigators to disseminate information to community members when attempting to address community concerns about a health problem. The development of communication tools, acknowledgement of the importance of relationship-building, and the re-evaluation of data disclosure policies that are applicable in these circumstances will help support the effective and successful investigation of community health threats, and foster the ability of investigators to adequately answer community questions and address concerns.
Conflict of interest and funding
The authors do not have any financial conflicts of interest to disclose. The research described in the case study was approved by the University of Alberta ethics board and all participants gave their informed consent.
Acknowledgements
The authors would like to thank the community of Aklavik, Northwest Territories, Canada and other members of the CANHelp Working Group.
References
- Trumbo CW. Public requests for cancer cluster investigations: a survey of state health departments. Am J Public Health. 2000; 90: 1300–2. 10.3402/ijch.v71i0.18414.
- Centers for Disease Control. Guidelines for investigating clusters of health events. MMWR Recomm Rep. 1990;39:1–23.
- Kingsley BS, Schmeichel KL, Rubin CH. An update on cancer cluster activities at the Centers for Disease Control and Prevention. Environ Health Perspect. 2007; 115: 165–71. 10.3402/ijch.v71i0.18414.
- Edwards A, Elwyn G, Mulley A. Explaining risks: turning numerical data into meaningful pictures. BMJ. 2002; 324: 827–30. 10.3402/ijch.v71i0.18414.
- Frewer L. The public and effective risk communication. Toxicol Lett. 2004; 149: 391–7. 10.3402/ijch.v71i0.18414.
- Plowfield L, Wheeler EC, Raymond JE. Time, tact, talent, and trust: essential ingredients of effective academic-community partnerships. Nurs Educ Perspect. 2005; 26: 217–20.
- Greenberg M, Wartenberg D. Communicating to an alarmed community about cancer clusters: a fifty state survey. J Community Health. 1991; 16: 71–82. 10.3402/ijch.v71i0.18414.
- Thun MJ, Sinks T. Understanding cancer clusters. CA Cancer J Clin. 2004; 54: 273–80. 10.3402/ijch.v71i0.18414.
- Jardine CG, Hrudey SE. Mixed messages in risk communication. Risk Anal. 1997; 17: 489–98. 10.3402/ijch.v71i0.18414.
- Chen Y. Cancer incidence in Fort Chipewyan, Alberta, 1995–2006. Edmonton: Alberta Cancer Board. 2009. [cited 2010 Mar 5]. Available from: http://www.ualberta.ca/~avnish/rls-2009-02-06-fort-chipewyan-study.pdf.
- Wartenberg D, Greenberg M. Methodological problems in investigating disease clusters. Sci Total Environ. 1992; 127: 173–85. 10.3402/ijch.v71i0.18414.
- Levy AG, Weinstein N, Kidney E, Scheld S, Guarnaccia P. Lay and expert interpretations of cancer cluster evidence. Risk Anal. 2008; 28: 1531–8. 10.3402/ijch.v71i0.18414.
- Estey E, Kmetic A, Reading J. Knowledge translation in the context of Aboriginal health. Can J Nurs Res. 2008; 40: 24–39.
- Statistics Canada. Disclosure control. Ottawa: Statistics Canada. 2009. [cited 2011 Jun 5]. Available from: http://www.statcan.gc.ca/pub/12-539-x/2009001/control-controle-eng.htm.
- Statistics Canada. Data sources and methodology: Disclosure control. Ottawa: Canadian Cancer Registry, Statistics Canada. 2010. [cited 2011 Jun 5]. Available from: http://www.statcan.gc.ca/cgi-bin/imdb/p2SV.pl?Function=getSurvey&SDDS=3207&lang=en&db=imdb&adm=8&dis=2#b7.
- Myers J, Frieden TR, Bherwani KM, Henning KJ. Privacy and public health at risk: public health confidentiality in the digital age. Am J Public Health. 2008; 98: 793–801. 10.3402/ijch.v71i0.18414.
- Nass SJ, Levit LA, Gostin LOInstitute of Medicine (US) Committee on Health Research and the Privacy of Health Information: The HIPAA Privacy Rule. Beyond the HIPAA privacy rule: enhancing privacy, improving health through research. Washington: The National Academies Press. 2009. 334. p.
- Gostin L. Health care information and the protection of personal privacy: ethical and legal considerations. Ann Inter Med. 1997; 127: 683–90.
- Statistics Canada. 2006Community Profiles. Aklavik, Northwest Territories (Code6107025) (table). 2006 Community Profiles. 2006 Census. Statistics Canada Catalogue no. 92-594-XWE. Ottawa: Statistics Canada. 2008 [cited 2011 Jun 27]. Available from: http://www12.statcan.gc.ca/census-recensement/2006/dp-pd/prof/92-591/details/Page.cfm?Lang=E&Geo1=CSD&Code1=6107025&Geo2=PR&Code2=61&Data=Count&SearchText=Aklavik&SearchType=Begins&SearchPR=01&B1=All&Custom=.
- Goodman KJ, Jacobson K, Veldhuyzen van Zanten S. Helicobacter pylori infection in Canadian and related Arctic Aboriginal populations. Can J Gastroenterol. 2008; 22: 289–95.
- Natural Resources Canada. The Atlas of Canada: Northwest Territories. Ottawa: Natural Resources Canada. 2006. [cited 2011 Jun 30]. Available from: http://atlas.nrcan.gc.ca/auth/english/maps/reference/provincesterritories/northwest_territories/referencemap_image_view.
- Cheung J, Goodman K, Munday R, Heavner K, Huntington J, Morse J, et al.. Helicobacter pylori infection in Canada's arctic: Searching for the solutions. Can J Gastroenterol. 2008; 22: 912–6.
- Sinnema J. Call for help. Edmonton Journal;2008. Feb 09 [cited 2012 Apr 19]. Available from: http://www2.canada.com/edmontonjournal/news/cityplus/story.html?id=ca78b5c6-7214-4896-9946-450b06beec11&p=1.
- Cornwall C. Can you catch cancer?. Canada: Reader's Digest Canada. (Canadian); 2010. [cited 2011 Jun 30]. Available from: http://www.readersdigest.ca/health/sickness-prevention/can-you-catch-cancer?id=2.
- Cancer in the Northwest Territories, 1990–2000. A descriptive report. Yellowknife: Department of Health and Social Services, Government of the Northwest Territories. 2003. [cited 2011 Nov 29]. Available from: http://www.hlthss.gov.nt.ca/pdf/reports/diseases_and_conditions/2003/english/cancer_in_the_nwt.pdf.
- CBC News. High rates of stomach bacteria in Arctic hamlet: study. Yellowknife: CBC News. 2008. [cited 2011 Jun 30]. Available from: http://www.cbc.ca/news/canada/north/story/2008/02/29/nwt-pylori.html.
- Wartenberg D, Thompson WD. Privacy versus public health: the impact of current confidentiality rules. Am J Public Health. 2010; 100: 407–12. 10.3402/ijch.v71i0.18414.
- McComas KA, Trumbo CW, Besley JC. Public meetings about suspected cancer clusters: the impact of voice, interactional justice, and risk perception on attendees’ attitudes in six communities. J Health Commun. 2007; 12: 527–49. 10.3402/ijch.v71i0.18414.
- Siegrist M, Cvetkovich GT, Gutscher H. Shared values, social trust, and the perception of geographic cancer clusters. Risk Anal. 2001; 21: 1047–53. 10.3402/ijch.v71i0.18414.
- Morgan MG, Fischoff B, Bostrom A, Lave L, Atman CJ. Communicating risk to the public. Environ Sci Technol. 1992; 26: 2048–56. 10.3402/ijch.v71i0.18414.
- Christopher S, Watts V, McCormick AK, Young S. Building and maintaining trust in a community-based participatory research partnership. Am J Public Health. 2008; 98: 1398–406. 10.3402/ijch.v71i0.18414.
- Bowen S, Martens P. Demystifying knowledge translation: learning from the community. J Health Serv Res Policy. 2005; 10: 203–11. 10.3402/ijch.v71i0.18414.
- Bayer R, Fairchild A. The limits of privacy: surveillance and the control of disease. Health Care Anal. 2002; 10: 19–35. 10.3402/ijch.v71i0.18414.