Abstract
Objective. To compare the current state of health research on Aboriginal and non-Aboriginal youth in Canada.
Design. A search of published academic literature on Canadian Aboriginal youth health, including a comprehensive review of both non-Aboriginal and Aboriginal youth research, was conducted using MEDLINE and summarized.
Methodology. A MEDLINE search was conducted for articles published over a 10-year period (2000–2010). The search was limited to research articles pertaining to Canadian youth, using various synonyms for “Canada,” “youth,” and “Aboriginal.” Each article was coded according to 4 broad categories: Aboriginal identity, geographic location, research topic (health determinants, health status, health care), and the 12 key determinants of health proposed by the Public Health Agency of Canada (PHAC).
Results. Of the 117 articles reviewed, only 34 pertained to Aboriginal youth, while the remaining 83 pertained to non-Aboriginal youth. The results revealed major discrepancies within the current body of research with respect to the geographic representation of Aboriginal youth, with several provinces missing from the literature, including the northern territories. Furthermore, the current research is not reflective of the demographic composition of Aboriginal youth, with an under-representation of Métis and urban Aboriginal youth. Health status of Aboriginal youth has received the most attention, appearing in 79% of the studies reviewed compared with 57% of the non-Aboriginal studies. The number of studies that focus on health determinants and health care is comparable for both groups, with the former accounting for 62 and 64% and the latter comprising 26 and 19% of Aboriginal and non-Aboriginal studies, respectively. However, this review reveals several differences with respect to specific focus on health determinants between the two populations. In non-Aboriginal youth studies, all the 12 key determinants of health of PHAC are explored, whereas in Aboriginal youth studies the health profile remains incomplete and several key determinants and health indicators are neglected.
Conclusions. The current studies are not reflective of the demographic and geographic profiles of Aboriginal youth in Canada, and they have also failed to provide a comprehensive examination of their unique health needs and concerns compared with studies on non-Aboriginal youth.
In 2006, the Canadian Aboriginal population surpassed the 1 million mark, totalling 1,172,790, identifying themselves as First Nations, Métis and Inuit Citation1. The Aboriginal population is not only the fastest growing population in Canada but also the youngest, with nearly 50% of the total population under the age of 24 compared with 31% of the general Canadian population Citation1. The majority of Aboriginal youth reside off-reserve, with 52% living in urban centres, followed by 32% on-reserve and the remaining in rural areas Citation1.
Despite comprising 3.8% of the total Canadian population, Aboriginal people are disproportionately burdened by health and social issues Citation1. In comparison with the general Canadian population, Aboriginal people experience much higher levels of poverty, unemployment, abuse, addiction, obesity and suicide Citation2. Aboriginal youth experience a mortality rate 3 times greater than that of non-Aboriginal youth and are 4 times more likely to suffer an injury (Citation3). For example, suicide is the leading cause of death of First Nations and Inuit youth with rates 5–6 times higher than that for non-Aboriginal youth Citation3. Substance abuse, including marijuana, inhalants and stimulants, is much higher among Aboriginal youth, and the approximate age of inhalant initiation is between 10 and 13, and on average the first use occurs at 11.5 years of age Citation3. In addition to illicit drugs, tobacco use is of particular concern because smoking rate in Aboriginal youth is 2 times higher than that of the general Canadian youth Citation4. Compared with the general Canadian youth, Aboriginal youth experience significantly higher rates of sexually transmitted infections (STIs), evidenced by a 7 times higher diagnosis rate of both chlamydia and HIV infection in the youth between the ages of 15 and 19 Citation5. These health disparities are compounded by the grave social inequalities Aboriginal people experience, such as racism, substandard living conditions (including lack of potable water and proper sanitation), crowding and abuse, all of which are further exacerbated by poverty. For example, the unemployment rate is 41% amongst Aboriginal youth aged 15–24 years, whereas it is only 13% amongst non-Aboriginal youth Citation2, and nearly half (42.5%) of the Aboriginal youth have not completed high school in contrast with only 23.5% of non-Aboriginal youth Citation2. Furthermore, they are 4 times more likely to live in a crowded house and 3 times more likely to live in a house that requires major repairs than non-Aboriginal youth Citation1. Although the health and social inequalities presented here are not exhaustive, they do represent several key social determinants of health. It is evident that Aboriginal youth experience much greater health disparities and inequities Citation6 than non-Aboriginal youth. This, in combination with the overall high rates of growth in the population of Aboriginal youth, demonstrates a need to understand the extent to which the current research adequately examines the pressing health needs of Aboriginal youth. In doing so, this study examines the current state of health research on Aboriginal youth in comparison with that on non-Aboriginal youth in Canada.
Material and methods
To review the current studies examining the health of Aboriginal youth, a MEDLINE search was conducted. A search of article titles was done using terms, such as “Aboriginal,” “First Nation(s),” “Inuit,” “Indigenous,” “native” and “Métis,” in combination with “Canada” and “Canadian,” to identify articles that focus on Aboriginal and non-Aboriginal populations. In addition, a range of search terms were used to identify articles that focus on youth, including “youth,” “adolescent,” “young” and “teen(ager).” Also, the search was limited to English publications between 2000 and 2010, and search terms for various age groups (all children: 0–12 years; adolescents: 13–18 years; young adults: 19–24 years) were used to maximize search for articles that did not have youth-related terms in the titles. Articles were read in their entirety and only those that focus on Canadian youth (Aboriginal and non-Aboriginal) and health-related data were included. Articles that focus only on immigrant Canadian youth were not included, as the focus of this study was a comparison between Aboriginal youth and general Canadian youth populations. Furthermore, articles on infants and children that had a reference to youth populations, which for the purpose of this review were classified as those between the ages of 12 and 30, were included. Furthermore, book reviews and literature reviews were not included for analysis.
On the basis of the study by Young Citation7, the articles selected for analysis were coded according to 4 broad categories: Aboriginal identity, geographic location, research topic (health determinants, health status, health care) and the 12 key determinants of health proposed by the Public Health Agency of Canada (PHAC). With respect to research topics and the key determinants of health, articles received multiple codes when applicable. The articles were further divided into various subcategories under the 3 research topics. The 4 broad categories are described below:
Aboriginal identity: Articles were coded according to 3 broad identity groups: First Nations, Métis and Inuit. Those articles where no Aboriginal group was specified were classified as Aboriginal.
Geographic location: The geographic focus of each article was assessed and coded on the basis of the geographic location (i.e. province/territory). Articles that focus on the Aboriginal youth population were further examined to identify whether the research was conducted on-reserve or off-reserve locations (i.e. rural and/or urban).
Research topic: The articles were coded on the basis of research topic.
Health care: This category includes articles that focus on some aspect of health care, such as treatment, preventative measures or public health.
Health status: This category represents the articles that focus on the following health outcomes: injury, chronic conditions, infectious diseases and mental health.
Health determinants: This category includes articles that focus on health determinants, which were classified into the following subcategories: lifestyle, human biology, social environment and physical environment.
12 key health determinants: The articles were also coded on the basis of the 12 key health determinants of PHAC: income and social status; social support networks; education and literacy; employment and working conditions; social environments; physical environments; personal health practices and coping skills; healthy child development; biology and genetic endowment; health services; gender; and culture.
Results
The process for identifying and selecting articles for inclusion resulted in a database containing 34 article on Aboriginal youth and 83 articles on non-Aboriginal youth.Footnote1 Among the articles on Aboriginal youth, 62% [21] focused on First Nations, 18% on Inuit and only 9% on Métis Citation8 Citation9. Interestingly, the initial search generated an even larger number of articles relating to Inuit populations, but they were subsequently removed as they dealt with infants and children. The 3 articles examining Métis youth also included First Nations and Inuit populations. Unfortunately, 35% of articles [13] with the term “Aboriginal” did not specify or indicate the Aboriginal groups being examined.
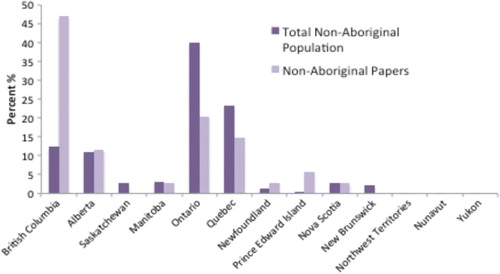
With respect to the geographic focus of the articles examined, 55% of the articles focused on-reserve populations, 45% on urban Aboriginal youth populations and 20% on rural populations (see ). Although the majority of reserve inhabitants are First Nations, 41% of First Nations youth reside in urban areas Citation10, yet only 10% of the articles on First Nations were urban-based Citation8 Citation11. In 11 of the 34 articles on Aboriginal youth, the geographic focus was not made explicit in terms of urban, rural or reserve.Footnote2 With respect to the scale of study, 53% [44] of the studies on non-Aboriginal youth were of national scale, whereas only 9% [3] of the studies on Aboriginal youth were of national scale. British Columbia was over-represented in the current body of research with respect to their youth populations, as a total of 47% [16] and 39% [10] of articles were focusing on non-Aboriginal and Aboriginal youth populations, respectively, of British Columbia. Manitoba was also over-represented in the Aboriginal youth research, accounting for 35% of the articles. Ontario was under-represented with only 7 (21%) articles, as it represents Canada's largest non-Aboriginal youth population, but was the third most studied with respect to Aboriginal youth research (31%). No studies existed for Alberta or Saskatchewan despite their significant Aboriginal youth populations. Although the Atlantic provinces make up more than 5% of the Aboriginal youth population, research on these youth is severely lacking. In addition, there has been no focus on Aboriginal youth populations located in the north (see and ). Only 3 comparative studies of Aboriginal and non-Aboriginal youth were retrieved Citation12.
Fig. 1. Regional geographic distribution of Aboriginal youth (aged 10–24) in comparison to research.4
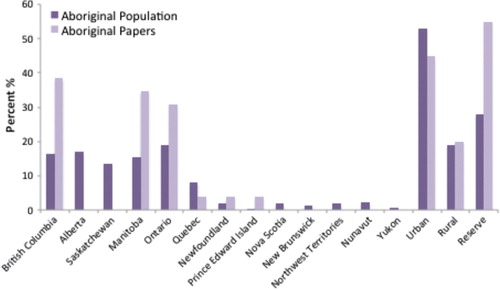
Fig. 2. Regional geographic distribution of non-Aboriginal youth (aged 10–24) population in comparison to research.
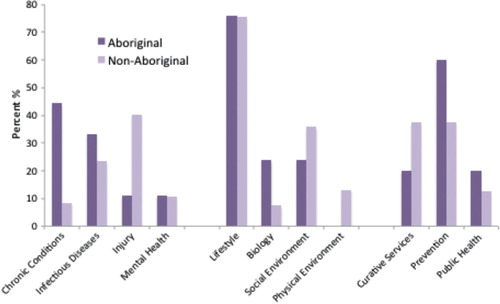
With respect to the health-related focus, health status was the focus of 79% [27] of the Aboriginal youth studies in comparison with 57% [47] of the non-Aboriginal youth studies. More than 60% of the studies for both youth populations examined health determinants, and 29% [10] of the Aboriginal youth studies and 19% [16] of the non-Aboriginal youth studies examined the aspects related to health care. With the exception of health status, when classified within these broad categories, the focus of health research on both groups appears quite similar (see ), but further analysis revealed interesting differences between the two populations (see ).
With respect to health status, chronic conditions were studied in nearly half [12] of the studies that focus on the health status of Aboriginal youth, and of these, 9 studies focused on diabetes and its related complications Citation10 Citation13. In contrast, only 9% of the non-Aboriginal youth studies examined chronic conditions [e.g. diabetes, cancer, asthma and fetal alcohol spectrum disorder (FASD)]. A total of 33% [9] of the Aboriginal youth studies related to health status dealt with infectious diseases in comparison with 23% of non-Aboriginal youth studies. The majority of Aboriginal studies focused on HIV infection (67%), with one-third pertaining to STIs and only one related to hepatitis. Articles on non-Aboriginal youth focused equally on hepatitis (27%) and HIV infection, with STIs accounting for the majority (55%). Studies on mental health were similar for both groups, representing 11% of the studies related to health status. Studies on injury comprised the largest percentage of non-Aboriginal youth studies at 40% [19], while it comprised only 11% [3] of Aboriginal youth studies. All Aboriginal youth studies regarding injury were related to suicide Citation14, whereas non-Aboriginal studies focused also on sports- and work-related injuries.
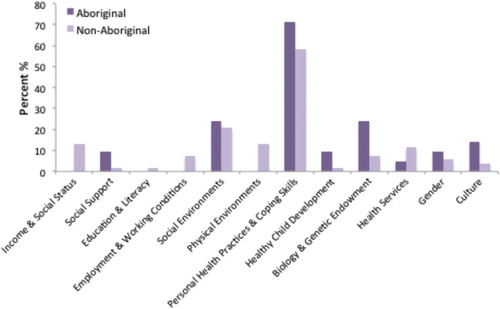
In terms of specific health determinants, more than 75% of studies for both youth populations were related to lifestyle. In particular, physical activity Citation11 Citation15, sexual behaviour Citation16 Citation17 and substance abuse Citation18 were all equally represented in the Aboriginal youth studies at 33% each, followed by diet [20%] Citation19 and tobacco use [13%] Citation4 Citation20. Substance abuse was the most prominent lifestyle factor for the non-Aboriginal youth population, totalling 43% followed by smoking (33%), physical activity (15%), diet (13%) and sexual behaviour (10%). Human biology, specifically genetics, was studied in 24% of the Aboriginal youth studies Citation21 compared with only 8% of the non-Aboriginal studies (see ).
Of the 29% [10] of Aboriginal youth studies examining health care, more than half (60%) dealt with prevention Citation15 Citation18 Citation22 and 20% focused on both public health and curative services Citation12. Traditional healing was not explored in any of the Aboriginal youth studies that focus on health care. In contrast, of the non-Aboriginal youth health care studies, curative services and prevention each represented a 38% share of the literature, while public health and access to services each accounted for 13%.
In Aboriginal youth studies related to health determinants, several of the 12 key health determinants identified by PHAC were not dealt with (see ). Personal health practices and coping skills was the most studied determinant, representing 71% of all Aboriginal studies, followed by social environment, and biology and genetic endowment (24%) and, lastly, culture [14%] Citation23. Gender, healthy child development, and social support networks were studied in 10% of the article, and health services were focused in 5% of the articles.
In contrast, it appears that non-Aboriginal youth studies better reflect the 12 key determinants of health. Personal health practices and coping skills was discussed in 58% of the articles that focus on the determinants of health—21% on social environment and 13% on physical environment. This was followed by health services (11%), employment and biology (8%), income and social status (13%) and gender (6%). Finally, culture and healthy child development represented 4% and social support networks, and education and literacy accrued to 2% of the total studies (see ).
Discussion
The aim of this study was to examine the current state of health research of Aboriginal youth in Canada in relation to the health research for the non-Aboriginal youth population. The MEDLINE search revealed that only 34 articles pertaining to Aboriginal youth were published between 2000 and 2010, whereas 83 articles pertaining to non-Aboriginal youth were published over the same time span. These low numbers are surprising given the general youthfulness of the Aboriginal population in addition to their troubling health status. It is, however, important to acknowledge that the low number of studies could be partially attributed to the selection methods used (i.e. searches were limited to key terms within titles only, and the search was limited to one database). However, since a large number of articles related to infants and children were retrieved from the initial search (but excluded from this analysis), it appears that these very young populations are the focus of the majority of research on younger cohorts of the Aboriginal population.
It is also acknowledged that the discrepancies found regarding Aboriginal identity could partially be affected by the ambiguity of the studies. Thirty-five per cent of those articles reviewed did not indicate the Aboriginal groups being examined. Overlooking the Aboriginal identities of participants in health research is a concern especially considering key differences between groups as they relate to status and health benefits. For example, status First NationsFootnote3 are eligible to receive a range of medical and health-related goods and services under the Non-Insured Health Benefits Program, such as dental care, drugs and medical transportation to access certain medical services Citation24, whereas Métis have no such privileges. It is clear that these differences with respect to access to health care and services amongst Aboriginal groups would have important health implications; thus, specifying the Aboriginal group when presenting research findings should be emphasized.
The findings presented here are similar to those of other reviews Citation7 Citation23, and they show that the existing body of research is not representative of the demographic and geographic composition of Aboriginal youth. At first glance, Inuit youth appear to be slightly over-represented, but when considering the articles (6%) that focus only on Inuit, the numbers are low Citation7 Citation25. Often over-represented in research Citation26 Citation27, these lower numbers are somewhat surprising. This perhaps indicates that Inuit populations have a significant presence within the broader literature on Aboriginal health, but studies relating to their youth are lacking. Finally, it appears that Métis youth are neglected within the current body of research. This reveals a significant gap that needs to be addressed, as the Métis population comprises a very unique Aboriginal group without land or status rights recognized by the federal government.
Research on Aboriginal youth is also not reflective of the geographic distribution of Aboriginal youth across Canada because 3 provinces account for most of the studies and several provinces entirely are absent from research. The fact that no studies on Aboriginal youth in the northern territories (Yukon, Nunavut and Northwest Territories) were conducted is particularly worrisome given the relative size of Aboriginal populations and their unique health concerns in these remote areas. Overall, the regional discrepancies in Aboriginal studies do not appear to be attributed to broader regional trends within youth research, as non-Aboriginal youth research is generally more representative of the geographic distribution of the population with the exception of a few provinces.
Census data shows that of Aboriginal youth aged between 10 and 24 years, 28% live on-reserves while more than half (53%) reside in urban areas and 19% live in rural areas Citation1. The current research however does not adequately reflect this, with on-reserve Aboriginal youth greatly over-represented, while under-emphasizing urban Aboriginal youth Citation1. These findings reflect those of Wilson and Young Citation38 and reveal the greater availability of data on on-reserve Aboriginal youth populations as compared with data on those living off-reserve whom are not as easily identified or located. It is often argued that researchers fail to recognize the urban presence of Aboriginal people because of on-going and prevalent misconceptions regarding where Aboriginal populations live and belong Citation28. In a review of Canadian Aboriginal health research conducted by Young Citation7, only 2% of the studies examined included urban Aboriginal populations. Although still under-represented, the higher percentage of urban Aboriginal youth populations found here may reveal a greater awareness of the presence of Aboriginal youth within cities (albeit the numbers are still low).
With respect to health status, health care and determinants of health, the results of this review revealed that health determinants and, to a slightly lesser extent, health care have received equal attention across both groups. However, in Aboriginal youth studies, health status has received a 20% greater focus. The emphasis on health status in Aboriginal youth research perhaps reflects their worse state of health compared with non-Aboriginal youth. That said, most of the studies focused on diabetes and its related complications while other important health issues were mainly overlooked. Although Canadian statistics for Fetal Alcohol Spectrum Disorder (FASD) are lacking, it can be agreed upon that for those communities with higher rates of alcohol use FASD would also be more common, such as in Aboriginal communities Citation29 where binge drinking is a reported issue Citation30. It is well-known that injury is the leading cause of death amongst Aboriginal youth Citation3, so it is concerning that injury was studied in only 3 of the Aboriginal articles, and all the 3 articles focused on suicide. In contrast, in the non-Aboriginal youth studies on injury, sports- and work-related injuries were also focused. This difference may be explained by the low participation rate of Aboriginal youth in recreational activities Citation31 Citation32 and the employment sector Citation2, which itself represents another important health issue. Although suicide accounts for a large portion of injuries among Aboriginal youth, injuries related to motor vehicle collisions, violence, abuse, falls and exposure (frostbite/hypothermia) also constitute major health concerns for Aboriginal youth Citation33, yet remain overlooked in the current studies.
Health care accounted for the lowest percentage of all studies on both groups. Given issues regarding access to health care services, cultural sensitivity in care and the need for public health and prevention within Aboriginal communities, more studies of health care are clearly needed. Although it is clear that research dedicated to prevention is a priority for both groups, research regarding curative services for Aboriginal youth is lacking in comparison with the literature available for non-Aboriginal youth. This finding is surprising given that Aboriginal youth are burdened with a wide range of health issues and the obvious relationship between poor health and the need for and/or use of health care services. In addition, cultural appropriateness of care, such as traditional healing, did not appear within any of the studies examining curative services. Furthermore, given the remoteness of a large percentage of Aboriginal youth in terms of residence with 16% living in rural areas and 28% living on-reserve Citation1, access to such services presents a major concern, yet this issue was examined in only one article Citation20.
With respect to health determinants, several key factors affecting the health of Aboriginal youth were neglected in the studies reviewed. Given the extremely high rates of smoking among Aboriginal populations Citation4 and the demonstrated poor health outcomes associated with tobacco use, it is puzzling as to why research on smoking has not been carried out at the same level as it has been in non-Aboriginal research. Furthermore, although the importance of the physical environment as a health determinant for Aboriginal youth is apparent given issues related to environmental contaminants, housing conditions and geographic location, researchers have neglected this topic in their studies on youth. Although Canada ranks 6th on the UN Human Development Index Citation34, many Canadian reserves can be best described as deplorable as substandard housing, lack of potable water and proper sanitation continue to shape the lives and health of reserve residents and those living in the North. Such conditions are linked to various infectious diseases such as tuberculosis Citation35 and gastrointestinal viruses Citation36. In addition, a link has been drawn between crowding and health outcomes related to violence, stress and injury Citation37, thus only exacerbating the poor health conditions of many Aboriginal youth.Footnote
When reviewing those articles focused on health determinants, several of the 12 key health determinants of PHAC were entirely absent form Aboriginal youth research, such as income and social status, education and literacy, employment and working conditions, and physical environments. As discussed previously, Aboriginal youth often experience challenges with respect to many of these key determinants, and as such, their importance as health priorities should be demonstrated by health research. In contrast, non-Aboriginal research examined all the 12 key determinants to some extent.
In summary, this review highlights several weaknesses in the research being conducted on the health of Aboriginal youth in Canada. In comparison with the non-Aboriginal youth research, there are major discrepancies in research that focus on the health of Aboriginal youth. Similar to the findings of Young Citation7 and Wilson and Young Citation38, health research on Aboriginal youth is not representative of their demographic or geographic composition. Furthermore, research on the non-Aboriginal youth population appears to capture a diverse and broad range of health-related issues, whereas research on Aboriginal youth has failed to produce a similar comprehensive picture. Although a substantial focus in research related to the health status of Aboriginal youth, suicide remains a neglected health outcome despite its overwhelming prevalence. In addition, several health determinants such as socio-economic status and physical environment have not received sufficient attention from researchers. It is alarming that health care ranked significantly lower on the research agenda compared with the aforementioned 2 categories given the fact that geographic access to health services and their cultural relevance remains a huge challenge to Aboriginal people. It is clear that Aboriginal youth are severely disadvantaged in terms of their health status and, thus, are likely the most in need of such services and care. It is clear that future research needs to approach the study of Aboriginal youth health from a broader perspective to adequately encompass the aspects of health determinants and health care appropriately in relation to the health status of this population. This is necessary to ensure that research addresses the unique health needs and concerns of Aboriginal youth and also provides a more comprehensive profile on the health of Aboriginal population.Footnote
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
Appendix
Notes
1Three comparative studies including both Aboriginal and non-Aboriginal youth populations have been added individually to the totals for both groups.
2It should be noted that select articles indicated more than one geographic focus and, thus, could be counted for up to 3 locations in the total percentages.
3Status First Nations (referred to as Status Indians within legislation) are those Aboriginal people registered with Indian and Northern Affairs Canada as according to the Indian Act of Canada.
4To arrive at this figure, we summed the total number of articles per province and divided it by the total number of articles indicating a provincial focus [26]. The same procedure was completed for calculating the total number of articles [20] for urban, rural and reserve. It should be noted that the numbers will not add up to 100% as some articles included more than one of these locations and, thus, could be counted more than once.
5 To arrive at this figure, we summed the total number of articles related to the given subcategory and divided it by the total number of articles within the broader category of interest.
References
- Statistics Canada. 2006. Aboriginal peoples in Canada 2006: Inuit, Metis and First Nations, 2006 Census. Ottawa: Statistics Canada. January 2008. Catalogue No. 97-558-X IE. Available from: http://www12.statcan.ca/census-recensement/2006/as-sa/97-558/p6-eng.cfm.
- Disant M, Hebert C, Bergeron O, Bruneau S. Aboriginal youth and social inequalities in health. [internet]. Quebec: Quebec Population Health Research Network. 2008Nov. Available from: http://www.santepop.qc.ca/bulletin.php?l=en&id=68..
- Coleman H, Charles G, Collins J. Inhalant use by Canadian Aboriginal youth. J Child Adoles Subst. 2001; 10: 1–20. 10.3402/ijch.v71i0.18497.
- Retnakaran R, Hanley A, Connelly P, Harris S, Zinman B. Cigarette smoking and cardiovascular risk factors among Aboriginal Canadian youths. CMAJ. 2005; 173: 885–9. 10.3402/ijch.v71i0.18497.
- Devries K, Free C, Morison L, Saewyc E. Factors associated with the sexual behavior of Canadian Aboriginal young people and their implications for health promotion. Am J Public Health. 2009; 99: 855–62. 10.3402/ijch.v71i0.18497.
- Adelson N. The embodiment of inequity. Can J Public Health. 2005; 96: 45–61.
- Young K. Review of the research on Aboriginal populations in Canada: relevance to their health needs. BMJ. 2003; 327: 419–22. 10.3402/ijch.v71i0.18497.
- Worthington C, Jackson R, Mill J, Prentice T, Myers T, Sommerfeldt S. HIV testing experiences of Aboriginal youth in Canada: service implications. AIDS Care. 2010; 22: 1269–76. 10.3402/ijch.v71i0.18497.
- Mill J, Jackson R, Worthington C, Archibald C, Wong T, Myers T, et al.. HIV testing and care in Canadian Aboriginal youth: a community based mixed methods study. BMC Infect Dis. 2008; 8: 132. 10.3402/ijch.v71i0.18497.
- Fact sheet- urban Aboriginal population in Canada. Aboriginal Affairs and Northern Development Canada. Last modified September, 15, 2010. Available from: http://www.aadnc-aandc.gc.ca/eng/1100100014298.
- Chuback J, Embil J, Sellers E, Trepman E, Cheang M, Dean H. Foot abnormalities in Canadian Aboriginal adolescents with Type 2 diabetes. Diabet Med. 2007; 24: 747–52. 10.3402/ijch.v71i0.18497.
- Ng C, Young K, Corey P. Associations of television viewing, physical activity and dietary behaviours with obesity in Aboriginal and non-Aboriginal Canadian youth. Public Health Nutr. 2010; 13: 1430–7. 10.3402/ijch.v71i0.18497.
- Allan C, Flett B, Dean H. Quality of life in First Nation youth with type 2 diabetes. Matern Child Health J. 2008; 12: 103–9. 10.3402/ijch.v71i0.18497.
- Mignone J, O'Neil J. Social capital and youth suicide risk factors in First Nations communities. Can J Public Health. 2005; 96: 51–4.
- Skinner K, Hanning R, Tsuji L. Barriers and supports for healthy eating and physical activity for First Nation youths in northern Canada. Int J Circumpolar Health. 2006; 65: 148–61.
- Steenbeek A. Empowering health promotion: a holistic approach in preventing sexually transmitted infections among First Nations and Inuit adolescents in Canada. J Holit Nurs. 2004; 22: 254–66. 10.3402/ijch.v71i0.18497.
- Devries K, Free C. “I told him not to use condoms”: masculinities, femininities and sexual health of Aboriginal Canadian young people. Sociol Health Illn. 2010; 32: 827–42. 10.3402/ijch.v71i0.18497.
- Mehrabadi A, Paterson K, Pearce M, Patel S, Craib KJ, Moniruzzaman A, et al.. Gender differences in HIV and hepatitis C related vulnerabilities among Aboriginal young people who use street drugs in two Canadian cities. Women Health. 2008; 48: 235–60. 10.3402/ijch.v71i0.18497.
- Skinner K, Hanning R, Tsuji L. Barriers and supports for healthy eating and physical activity for First Nations youth in northern Canada. Int J Circumpolar Health. 2006; 65: 148–61.
- Ritchie A, Reading J. Tobacco smoking status among Aboriginal youth. Int J Circumpolar Health. 2004; 63: 405–9.
- Sellers E, Triggs-Raine B, Rockman-Greenberg C. The prevalence of the HNF-1alpha G319S mutation in Canadian Aboriginal youth with type 2 diabetes. Diabetes Care. 2002; 25: 2202–6. 10.3402/ijch.v71i0.18497.
- Panagiotopoulos C, Rozmus J, Gagnon R, Macnab A. Diabetes screening of children in a remote First Nations community on the west coast of Canada: challenges and solutions. Rural Remote Health. 2007; 7: 771.
- Schinke R, Yunablut H, Blodgett A, Eys M, Peltier D, Ritchie S, et al.. The role of families in youth sport programming in a Canadian aboriginal reserve. J Phys Act Health. 2010; 7: 156–66.
- Health Canada. First Nations, Inuit and Aboriginal health. Ottawa: Health Canada. November 2011. Available from: http://www.hc-sc.gc.ca/fniah-spnia/nihb-ssna/c3-qa-qr-eng.phponFebruary.
- Steenbeek A, Tyndall M, Rothenberg R, Sheps S. Determinants of sexually transmitted infections among Canadian Inuit adolescent populations. Public Health Nurs. 2006; 23: 531–4. 10.3402/ijch.v71i0.18497.
- Kovesi T, Gilbert N, Stocco C, Fugler D, Dales R, Guay M, et al.. Indoor air quality and the risk of lower respiratory tract infections in young Canadian Inuit children. CMAJ. 2007; 177: 155. 10.3402/ijch.v71i0.18497.
- Dallaire F, Dewailly É Muckle G, Ayotte P. Time trends of persistent organic pollutants and heavy metals in umbilical cord blood of Inuit infants born in Nunavik (Québec, Canada) between 1994 and 2001. Environ Health Perspect. 2003; 111: 1660–64. 10.3402/ijch.v71i0.18497.
- Peters E. “Our city Indians”: negotiating the meaning of First Nations urbanization in Canada, 1945–1975. Hist Geogr. 2002; 30: 75–92.
- Square D. Fetal alcohol syndrome epidemic on a Manitoba reserve. CMAJ. 1997; 157: 59–60.
- MacMillan H, Walsh C, Jamieson E, Wong MY, Faries EJ, McCue H, et al.. The health of Ontario First Nations people: Results from the Ontario First Nations Regional Health Survey. Can J Public Health. 2003; 94: 168–172.
- Blodgett A, Schinke R, Fisher L, Yungblut H, Recollet-Saikkonen D, Peltier D, et al.. Praxis and community-level sport programming strategies in a Canadian aboriginal reserve. IJSEP. 2010; 8: 262–83.
- Skinner K, Hanning R, Tsuji L. Barriers and supports for healthy eating and physical activity for First Nation youths in northern Canada. Int J Circumpolar Health. 2006; 65: 148–61.
- Health Canada. Unintentional and intentional injury profile for Aboriginal people in Canada: 1990–1999. Ottawa: Minister of Public Works and Government Services Canada. 2001. Catalogue No. H35-4/8-1999. p. 1–18.
- Human Development Report. Sustainability and equity: a better future for all. New York: United Nations Development Programme. 2011.
- Clark M, Riben P, Nowgesic E. The association of housing density, isolation and tuberculosis in Canadian First Nations communities. Int J Epidemiol. 2002; 31: 940–5. 10.3402/ijch.v71i0.18497.
- Rosenberg T, Kendall O, Blanchard J, Martel S, Wakelin C, Fast M. Shigellosis on Indian reserves in Manitoba, Canada: its relationship to crowded housing, lack of running water, and inadequate sewage disposal. Am J Public Health. 1997; 87: 1547–51. 10.3402/ijch.v71i0.18497.
- Lauster N, Tester F. Culture as a problem linking material inequality to health: on residential crowding in the Arctic. Health and Place. 2010; 16: 523–30. 10.3402/ijch.v71i0.18497.
- Wilson K, Young K. An overview of Aboriginal health research in the social sciences. Int J Circumpolar Health. 2008; 67: 179–89.