Abstract
Background. Among circumpolar populations, recent research has documented a significant increase in risk factors which are commonly associated with chronic disease, notably obesity.
Objective.The present study undertakes a scoping review of research on obesity in the circumpolar Inuit to determine the extent obesity research has been undertaken, how well all subpopulations and geographic areas are represented, the methodologies used and whether they are sufficient in describing risk factors, and the prevalence and health outcomes associated with obesity.
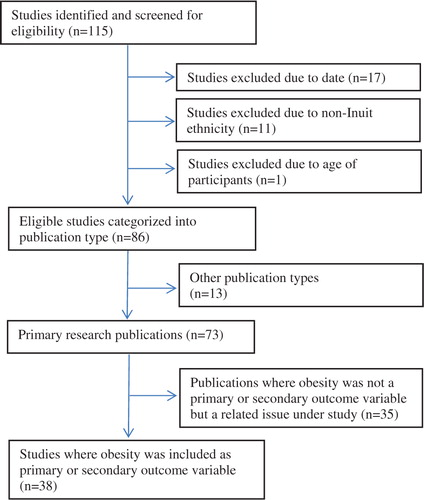
Design. Online databases were used to identify papers published 1992–2011, from which we selected 38 publications from Canada, the United States, and Greenland that used obesity as a primary or secondary outcome variable in 30 or more non-pregnant Inuit (“Eskimo”) participants aged 2 years or older.
Results. The majority of publications (92%) reported cross-sectional studies while 8% examined retrospective cohorts. All but one of the studies collected measured data. Overall 84% of the publications examined obesity in adults. Those examining obesity in children focused on early childhood or adolescence. While most (66%) reported 1 or more anthropometric indices, none incorporated direct measures of adiposity. Evaluated using a customized quality assessment instrument, 26% of studies achieved an “A” quality ranking, while 18 and 39% achieved quality rankings of “B” and “C”, respectively.
Conclusions. While the quality of studies is generally high, research on obesity among Inuit would benefit from careful selection of methods and reference standards, direct measures of adiposity in adults and children, studies of preadolescent children, and prospective cohort studies linking early childhood exposures with obesity outcomes throughout childhood and adolescence.
The human biology of Arctic populations has interested scientists since the 1800s. Narrative accounts exist from as early as the 18th and 19th centuries Citation1, Citation2 and the anthropometry of Inuit populations was the subject of early studies by noted anthropologists Boas Citation3 and Hrdlička Citation4, Citation5. Comprehensive nutritional surveys were conducted in the mid-20th century on subpopulations in the Arctic by United States and Canadian government agencies Citation6, Citation7 and by the International Biological Program (IBP) in 1968–1972 Citation8.
It is well documented that in recent decades, rapid social and economic changes have resulted in a health transition characterized by changes in diet and physical activity patterns and the emergence of health problems such as obesity, diabetes, hypertension, ischemic heart disease and stroke Citation9–Citation14.
Since 2000, a number of large-scale health and nutrition surveys have been undertaken in Alaska, Canada and Greenland. These have been supplemented by other more localized studies which examine various aspects of the health transition currently underway in circumpolar regions. The present study undertakes a comprehensive scoping review of this literature with the goal of examining the subject of obesity in the circumpolar Inuit.
Materials and methods
Target population
Our populations of interest are collectively referred to as Inuit, which extend from the Chukotka peninsula in Russia across Alaska and northern Canada to Greenland. They are known by a variety of self-designated names in different regions (including Yuit, Yupik, Inupiat, Inuvialuit, Inuit and Kalaallit). Our search revealed no English-language studies of obesity on Inuit living in Russia and they are excluded from our scoping review.
Research questions
In 2005 Arksey and O'Malley Citation15 published a methodological framework which presented 4 purposes for which a scoping review is appropriate:
To examine the extent, range and nature of research activity.
To determine the value of undertaking a full systematic review.
To summarize and disseminate research findings.
To identify research gaps in the existing literature.
The present study centres on the first purpose, namely to explore the extent, range and nature of research activity on obesity in the circumpolar Inuit: To what extent has obesity research been undertaken in the circumpolar context? Are all subpopulations and geographic areas represented? What methodologies are employed and are they sufficient to the task of describing risk factors, prevalence and health outcomes associated with obesity?
Our study also addresses the third and fourth purposes: What is the prevalence of obesity? What temporal trends, environmental risk factors and health outcomes are associated with obesity in this population?
Finally, we undertake comprehensive assessment of the field as a whole and identify gaps in the existing literature: What subgroups of this population are under-researched, what methodologies are underutilized, and what further research is needed?
Definitions and search strategies
We operationalized “obesity” as a condition defined by direct or indirect assessment of excess body fat or adiposity, including body mass index (BMI), various measures of abdominal obesity including waist circumference (WC) and waist-hip ratio (WHR), percent body fat and sum of skinfold thicknesses.
We wanted to explore obesity in the widest possible age range. Both the Dietitians of Canada and the Canadian Pediatric Society recommend the use of BMI to screen for overweight and obesity in children 2 or more years of age Citation17, and a variety of guidelines exist for the identification of obesity in children 2 years and older Citation18–Citation21. Under the age of 2 years, rapid growth and variety in feeding practices make it difficult to identify children at risk of obesity Citation21. We have therefore excluded studies of infants and children under 2 years.
The online databases Cochrane Library, JSTOR, Medline, PubMed, Science Citation Index, Science Direct and Scopus were used to compile a list of English-language papers. Search terms included a combination of medical subject headings and keywords related to the inquiry: Greenlandic, Inuit, Eskimo, Inupiat, Alaska(n), Aboriginal, indigenous, health, overweight, obesity, adiposity, body fat, body mass index, waist circumference, waist-hip ratio, diabetes, metabolic disease. The websites of national and regional governments and health agencies were searched for relevant published and unpublished documents. The publication records of authors and the reference lists of identified papers were combed for additional related resources. Duplicate citations from the multiple databases were removed. The search identified 115 citations which were assembled in an online Refworks (Refworks-COS, Bethesda, MD) file available to members of the team throughout the review.
Study selection
Inclusion and exclusion criteria were developed based on the objectives of the research. Studies were included in the review on the following basis:
The study was published during the 20-year period spanning 1992–2011.
Participants were age 2 years or greater.
Participants were identified in the study as “Greenlandic”, “Inuit” or “Eskimo” or any of the regional self-designated terms.
The study included 30 or more participants.
“Obesity” or “abdominal obesity” was a primary or secondary outcome variable or associated factor.
The study was the result of primary research.
Study selection () was conducted independently by both the principal reviewer (TG) and a second reviewer (HB). Inter-rater reliability was assessed by the Kappa statistic (K). The review team included authors of several of the papers identified in the literature search. These authors were excluded from selection, data extraction or quality assessment (QA) of their own papers.
Data extraction
A customized data extraction instrument was developed to explore the scope of the available literature and to compare study design, methodology and results. The instrument summarizes study characteristics and findings, allows for expansion of sections relevant to each study under review, and permits comparisons across studies. Data collected were entered into a spreadsheet made available to the entire review team.
Quality assessment (QA)
We undertook QA of all selected studies using a modified version of the STROBE instrument Citation22, Citation23 (STrengthening the Reporting of OBservational studies in Epidemiology), a checklist of 22 items designed for cohort, case-control, and cross-sectional studies and intended as a tool to improve the consistency, quality and transparency of epidemiologic reporting. It is not designed to evaluate the quality of the research studies themselves Citation24, Citation25. A review of 86 published QA instruments yielded no clear candidate for a generic QA tool as the majority of reviewers develop subject-specific instruments Citation26.
We followed the recommendation of Sanderson et al. Citation26 and used the comprehensive STROBE statement as a starting point for our own QA instrument. However with its emphasis on reporting, STROBE may inflate the quality of studies which are methodologically weak due to small sample size or lack of geographic representativeness. We therefore incorporated elements from the Scottish Intercollegiate Guidelines Network (SIGN) Citation27 methodology checklist in the development of our QA instrument. The resulting instrument yields a numeric QA score with maximum values that range from 27 to 29 depending on study design. We calculated percentage scores based on the maximum score for each category of study design and classified results as follows: “A” studies (QA score >85%); “B” studies (QA score 76–85%); “C” studies (QA score 61–75%); and “D” studies (QA score≤60%). In accordance with recommendations Citation28, the QA was piloted prior to implementation. Two reviewers (TG and HB) performed QA on 4 randomly-selected studies (11% of those selected) and the results were compared using the K-statistic. Then QA was performed by one of the reviewers (either TG or HB) on each of the studies reviewed.
We use the term “study” in this paper to refer to journal articles and reports. These publications ultimately were based on a far smaller number of research studies or projects conducted in specific regions and are thus not independent. Several publications from one study thus share the same methodological features of the parent study and only the reporting may differ. These publications may report on different “cuts” of the master dataset in terms of age–sex categories or other criteria. Furthermore, some publications report on the result of merging of the datasets of one or more of these studies.
Results
Application of study selection criteria resulted in the inclusion of 38 studies in the review ( and ). The inter-rater reliability for the study selection was extremely strong (weighted K=0.90, p<0.001).
Table I. Studies of adult circumpolar Inuit included in the review by country of study, sample size, participants, study design and anthropometric measures/indices
Geographic coverage, participants and study design
Thirty-nine percent of studies examined obesity among Canadian Inuit; 24% were set in Alaska and 33% in Greenland. Two studies compared obesity prevalence among all 3 countries. No studies of Siberian Inuit were located.
The majority of studies (84%) examined obesity in adults. The age range of adult participants tended to be broad, however, the lower age limit varied considerably (). The exclusion of pregnant subjects was reported in 28% of studies. The study design was exclusively cross-sectional; however, 19% of studies made comparisons to earlier research in order to report temporal trends in obesity metrics.
There were 6 studies on children from Canada and Greenland, and none from Alaska. Three of these were retrospective cohorts constructed from Greenland health surveillance data based on growth measures taken in doctors’ offices at age 2 years, at school entry and at various points during childhood and adolescence, which permitted the authors to examine the pattern of obesity onset in Greenland Inuit children and youth ages 2–17 years.
Table II. Studies of circumpolar Inuit children included in the review by country of study, participants, study design and anthropometric indices
Measurement, metrics and reference standards
All but one of the studies collected measured, rather than reported data. Age-standardized prevalence of obesity was reported in 47% of studies; the remainder reported only crude prevalence.
BMI was used as an index of body size in all studies reviewed and was the only metric employed in studies in children. Overall, the majority of studies (66%) employed a combination of anthropometric markers; the most common combinations were BMI+WC (17%) and BMI+WC+WHR (25%). No direct measures of adiposity, such as dual-energy X-ray absorptiometry or computerized tomography, were used.
Studies at the oldest end of the date range, prior to the publication of universal reference values for BMI, WC and WHR, used a variety of reference standards, such as the 1987 US National Center for Health Statistics standards for men and women Citation51, Citation52, Citation64 and Bray's BMI cutoff of 26 kg/m2 Citation28, Citation65 The majority of studies of adults (63%) employed BMI, WC and WHR cutoffs defined by the World Health Organization (WHO) Citation66–Citation68.
All studies of children undertaken in Greenland used the International Obesity Task Force (IOTF) reference values to define childhood obesity Citation18. Both the IOTF and the 2000 Centers for Disease Control (CDC) reference Citation20 were used in the 3 Canadian publications derived from the Nunavut Inuit Child Health Survey Citation58–Citation60.
Quality assessment
During the QA pilot, there was moderate inter-rater reliability (K=0.43, p=0.046). Raters subsequently reviewed the QA protocol together step-by-step to improve the consistency of rating prior to undertaking QA during the review.
The QA rated 26% of studies “A”, 18% “B”, 39% “C” and 16% “D”. Failure to achieve optimal quality scores resulted from a lack of clear definition of variables and data sources, in particular the failure to define obesity as a study variable. In 61% of studies, the authors did not provide adequate rationale for the obesity metric or the reference criteria used. A second major factor in study quality ranking was a lack of discussion of biases and limitations of the selected methodology; this occurred in 76% of studies.
Prevalence of obesity, associated risk factors and health outcomes
We compared the obesity prevalence reported in studies of Inuit adults (). In general, higher abdominal obesity prevalence was observed in women than in men. This gender difference was particularly marked in studies reporting abdominal obesity, the sole exception being a Greenland study of adults aged 35–86 years Citation46 which employed lower WC cutoff values for abdominal obesity.
Table III. Prevalence (%) of obesity and abdominal obesity among Inuit adults by sex and country of study
Eighty-two percent of studies analyzed risk factors associated with obesity, most commonly metabolic risk factors: lipid profile (44%); serum glucose values (56%); and either serum insulin or insulin resistance or both (13%). Prevalence of hypertension was reported in 34% of adult studies. The tendency for obesity to be significantly associated with insulin resistance, impaired glucose metabolism, and unfavourable lipid profile was widely reported among adults. The metabolic syndrome (MetS) has received increasing interest. Four studies examined the impact of variation in existing diagnostic criteria for MetS Citation31, Citation37, Citation45, Citation47. Among these studies, reported prevalence of MetS was consistently near 20%. There was considerable discussion about whether abdominal obesity (indicated by high WC) had as deleterious an effect on metabolic risk relative to non-Inuit populations. Two papers called for improved diagnostic criteria for MetS Citation31, Citation45 and 2 others documented moderate agreement between WHO and National Cholesterol Education Program diagnostic criteria for MetS Citation37, Citation47.
Relatively few studies looked at diet and physical activity as risk factors for obesity among Inuit. Twenty-three percent of studies documented increased obesity prevalence in individuals with high energy intake, low physical activity measures, or some combination of both. The Nunavut Inuit Child Health Survey was unable to establish a relationship between obesity risk and the consumption of market foods Citation59, Citation60. In Greenland a study showed that overweight at school entry (age 7 years) predicted overweight in late childhood and adolescence Citation60.
The association between obesity and SES, specifically education, employment, job type and childhood socioeconomic conditions, was examined in 7 studies. Two studies one in adults Citation58 and one in children Citation58 failed to find any association between household food insecurity and obesity outcomes. In Greenland, Westernization influenced the development of obesity and metabolic risk, although the processes differed among men and women. For men, risk of obesity and metabolic disease arose through a decrease in traditional hunting and fishing activities; for women, the negative health consequences of Westernization seem to be mediated through differences in SES, mainly educational attainment Citation47.
Discussion
In terms of overall scope, the literature on obesity in Inuit populations is presently skewed toward studies of adults. This is likely due to the fact that obesity is a strong risk factor of diabetes and cardiovascular disease, which are primarily diseases of adults. There is strong evidence that obesity is increasing, that abdominal obesity is widely prevalent among Inuit women, and that (above a certain threshold not yet well-defined) obesity has a deleterious effect on metabolic and cardiovascular health. In 1996 Young observed that, in past studies, the low prevalence of obesity among Inuit set them apart from other North American Aboriginal populations Citation28. Studies published since 2000 document a consistent rise in obesity prevalence with increasing prevalence in the WHO class II (BMI 35–39.9) and III (BMI≥40) categories of obesity Citation38, Citation50, Citation53, Citation54, Citation69. Many studies report disproportionately high prevalence of obesity (measured by BMI) and centripetal fat patterning (measured by WC and WHR) among Inuit women Citation11, Citation30, Citation32, Citation37, Citation38, Citation52, Citation55.
There is substantial evidence that obesity prevalence is increasing in children, which is particularly well documented in Greenland Citation62, Citation63. The most recent data come from the Nunavut Inuit Child Health Survey, where the prevalence of overweight and obesity (using IOTF cutoffs) in this preschool age sample were 39 and 28%, respectively Citation58. Such high prevalence raises significant concern over future health and metabolic disease risk in children.
There is also strong evidence from Greenland and Nunavut that the age of obesity onset is decreasing, such that obesity has emerged as a significant health concern in Inuit preschoolers Citation59, Citation62. The decreasing age of onset of overweight is part of a constellation of biological processes (including earlier skeletal maturity, earlier adolescent growth spurt, and decreasing age at menarche) accompanying rapid acculturation to a Western lifestyle Citation70, Citation71.
There are pronounced gaps in our knowledge of obesity among Inuit children, especially adolescents (our review located only 2 studies) Citation61, Citation63 and no recent data on obesity prevalence among children aged 10–12 years. There are no studies of obesity among children and youth living in Alaska. It is increasingly recognized that many adult health problems have their origin in childhood, and socioeconomic factors operating during childhood has been shown to be associated with adult obesity among Greenlanders Citation41. Prospective cohort studies offer the opportunity to examine associations between early childhood environment and obesity as well as the relative contribution of obesity and other risk factors to metabolic and cardiovascular health outcomes in Inuit adults.
In terms of international comparison, this review located only 2 studies that compared obesity prevalence in adult populations Citation56, Citation57. While it is likely that obesity and its concomitant health effects are influenced by processes particular to each country, there is nevertheless marked consistency in patterns of risk factors, prevalence and health-related outcomes among Inuit. Examples are changes in diet and physical activity patterns Citation9, Citation50, Citation58, Citation72 and the role of a marine diet in mitigating some of the negative health effects of acculturation to a Western lifestyle Citation32, Citation73–Citation76.
We make several observations regarding the methodologies currently in use to assess obesity in the circumpolar Inuit. First, while the link between obesity and metabolic/cardiovascular disease risk in this population is well established, there is evidence that current diagnostic thresholds may not reflect the levels of risk experienced by Inuit. Studies demonstrate that for given levels of obesity, Inuit have lower blood pressure, lower levels of glucose, insulin, triglyceride and higher levels of HDL cholesterol than non-Inuit subjects Citation31, Citation44, prompting some researchers to call for Inuit-specific cutoffs for central obesity measures associated with diabetes and cardiovascular disease outcomes Citation31, Citation44, Citation57. However, we find consistency in the relationship between rising adiposity and health risks. There is ample evidence that Inuit mortality from cardiovascular disease is at least as high as in non-Inuit populations and that Inuit mortality from cerebrovascular disease is significantly higher Citation56. Rather than developing ethnic-specific cutoff values, we propose that researchers first undertake validation studies to determine the accuracy of indirect measures of adiposity in Inuit adults and children.
There is a dearth of body composition studies among the Inuit. The accumulation of intra-abdominal or visceral fat is a marker of considerable metabolic risk. However without imaging studies (e.g. dual X-ray absorptiometry, computerized tomography, ultrasonography and magnetic resonance imaging) it is not known whether central obesity is predominantly intra-abdominal or subcutaneous. While attempts have been made to more accurately describe fat- and lean-mass distribution in Inuit Citation77, Citation78 we still know relatively little about fat distribution at various levels of BMI or waist circumference in this population.
Finally, we observe a general failure to define obesity as a variable. The quality of studies would be significantly improved by careful selection of metrics and reference standards and consistent reporting of limitations. Our review found multiple metrics employed in 66% of studies however BMI was the sole indirect measure of adiposity employed in studies of children. There is evidence that methodologies such as WC, triceps skinfolds and mid-upper arm circumference (MUAC) may be effective tools for obesity screening in children Citation79, Citation80. Inclusion of these methodologies may assist in the improvement of health surveillance programs for Inuit children. Standardized protocols incorporating hold-out samples and repeat measures would permit reporting of inter- and intra-observer error and technical error of measurement Citation81, features which would improve both the rigour and comparability of anthropometric studies.
Given the logistical challenges of conducting obesity research in the north, it is likely that the majority of future studies will continue to employ indirect measures of adiposity. In order to improve consistency in the use of cutoffs for classifying body weight in Inuit populations, we recommend the following: (a) The use and reporting of WHO cutoffs for adults Citation67, Citation68 and (b) Until international consensus is reached on the appropriate reference for children, the use and reporting of prevalence determined by both the IOTF Citation18 and WHO growth standard and reference for children Citation19, Citation21.
Conclusion
The results of this review indicate that concerted research effort has yielded substantial knowledge about the prevalence and factors associated with obesity in the circumpolar Inuit. With the exception of Inuit in Chukotka, Russia, there is broad geographic coverage of the regions where Inuit reside. Obesity prevalence is high among adults and has risen significantly in selected populations of preschool- and school-aged children. Inuit women are at greater risk of abdominal obesity than Inuit men however in both sexes obesity is associated with elevated metabolic risk factors such as insulin resistance, impaired glucose metabolism and negative trends in lipid profile.
While the quality of studies is generally high and relies on measured, rather than reported, data, research on obesity among Inuit would benefit from emphasis on several areas: careful selection of metrics and reference standards; direct measures of adiposity in adults and children which can be used to determine accurate anthropometric markers of disease risk; studies of preadolescent children; and prospective cohort studies linking early childhood exposures with obesity outcomes throughout childhood and adolescence.
Conflict of interest and funding
The authors have no conflict of interest to declare.
Acknowledgements
This research was made possible through the generous support of the CIHR Team in Circumpolar Health.
References
- Michael HN. Lieutenant Zagoskin's travels in Russian America, 1842–1844, translation from Russian sources, No 7. Toronto: University of Toronto Press. 1967. 358. p.
- Oswalt WH. Eskimos and explorers. Novato CA: Chandler and Sharp. 1979. 349. p.
- Boas F. Bureau of American Ethnology, 6th Annual Report. Smithsonian. Washington DC, 1888; 675.
- Hrdlička A. Anthropological survey in Alaska. 46th Annual Report of the Bureau of American Ethnology, 1928–1929. Washington DC: Bureau of American Ethnology. 1930. 654. p.
- Hrdlička A. Height and weight in Eskimo children. Am J Phys Anthropol. 1941; 28: 331–41. 10.3402/ijch.v71i0.18698.
- Mann GV, Scott EM, Hursh LM, Heller CA, Youmans JB, Consolazio CF, et al.. The health and nutritional status of Alaskan Eskimos: a survey of the interdepartmental committee on nutrition for national defense 1958. Am J Clin Nutr. 1962; 11: 31–76.
- Demirjian A. Anthropometry report: height, weight and body dimensions. Ottawa: Minister of National Health and Welfare, Health and Promotion Directorate, Health Services and Promotion Branch. 1980. 133. p.
- Auger F, Jamison PL, Balslev-Jorgensen J, Lewin T, de Penã JF, Skrobak-Kaczynski J. Anthropometry of circumpolar populations. The human biology of circumpolar populations. Milan FCambridge University Press. Cambridge, 1980; 213–55.
- Bjerregaard P, Jeppessen C. Inuit dietary patterns in modern Greenland. Int J Circumpolar Health. 2010; 69: 13–24.
- Castor ML, Smyser MS, Taualii MM, Park AN, Lawson SA, Forquera RA. A nationwide population-based study identifying health disparities between American Indians/Alaska Natives and the general populations living in select urban counties. Am J Public Health. 2006; 96: 1478–84. 10.3402/ijch.v71i0.18698.
- Dewailly E, Chateau-Degat ML, Ékoé JM, Ladouceur R. Nunavik Inuit Health Survey 2004/Qanuippitaa? How are we? Status of cardiovascular disease and diabetes in Nunavik. Quebec: Institut National de Santé Publique de Québec and Nunavik Regional Board of Health and Social Services. 2007. 20. p.
- Ebbesson SO, Adler AI, Risica PM, Ebbesson LO, Yeh JL, Go OT, et al.. Cardiovascular disease and risk factors in three Alaskan Eskimo populations: the Alaska Siberia project. Int J Circumpolar Health. 2005; 64: 365–86.
- Ng C, Corey PN, Young TK. Socio-economic patterns of obesity among aboriginal and non-Aboriginal Canadians. Can J Public Health. 2011; 102: 264–8.
- Sarkar J, Lix LM, Bruce S, Young TK. Ethnic and regional differences in prevalence and correlates of chronic diseases and risk factors in northern Canada. Prev Chronic Dis. 2010; 7: A13.
- Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005; 8: 19–32. 10.3402/ijch.v71i0.18698.
- Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010; 5: 69. 10.3402/ijch.v71i0.18698.
- Dietitians of Canada, Canadian Paediatric Society, The College of Family Physicians of Canada, Community Health Nurses of Canada. Promoting optimal monitoring of child growth in Canada: using the new World Health Organization growth charts – executive summary. Paediatr Child Health. 2010;15:77–83.
- Cole TJ, Bellizi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000; 320: 1–6. 10.3402/ijch.v71i0.18698.
- de Onis M, Onyango A, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007; 85: 660–7. 10.3402/ijch.v71i0.18698.
- Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al.. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat 11. 2002; 246: 1–190.
- WHO Multicentre Growth Reference Study Group. WHO child growth standards based on length/height, weight and age. Acta Paediatr. 2006;(Suppl 450): 76–85.
- Institute for Social and Preventive Medicine. STROBE statement: strengthening the reporting of observational studies in epidemiology. Bern: Institute for Social and Preventive Medicine. 2007. [cited 2011 Dec 1]. Available from: http://www.strobe-statement.org/index.php?id=strobe-home.
- Vandenbroucke JP, von Elm E, Altman DG, Gøtzche PC, Mulrow CD, Pocock SJ, et al.. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLoS Med. 2007; 4: e297. 10.3402/ijch.v71i0.18698.
- von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008; 61: 344–9. 10.3402/ijch.v71i0.18698.
- Da Costa BR, Cevallos M, Altman DG, Rutjes AWS, Egger M. Uses and misuses of the STROBE statement: bibliographic study. BMJ Open. 2012. [Epub ahead of print] [cited 2012 June 6]. Available from: http://bmjopen.bmj.com/content/1/1/e000048.draft-revisions.pdf.
- Sanderson S, Tatt ID, Higgins JPT. Tools for assessing quality and susceptibility to bias in observational studies in epidemiology: a systematic review and annotated bibliography. Int J Epidemiol. 2007; 36: 666–76. 10.3402/ijch.v71i0.18698.
- Scottish Intercollegiate Guidelines Network. Critical appraisal: notes and checklists. Edinburgh: Scottish Intercollegiate Guidelines Network. 2011. [cited 2011 Dec 8]. Available from: http://www.sign.ac.uk/methodology/checklists.html.
- Young TK. Obesity, central fat patterning, and their metabolic correlates among the Inuit of the Central Canadian Arctic. Hum Biol. 1996; 68: 245–63.
- Carter EA, MacCluer JW, Dyke B, Howard BV, Devereux RB, Ebbesson SO, et al.. Diabetes mellitus and impaired fasting glucose in Alaska Eskimos: the Genetics of Coronary Artery Disease in Alaska Natives (GOCADAN) study. Diabetologia. 2006; 49: 29–35. 10.3402/ijch.v71i0.18698.
- Charbonneau-Roberts G, Young TK, Egeland GM. Inuit anthropometry and insulin resistance. Int J Circumpolar Health. 2007; 66: 129–34.
- Chateau-Degat ML, Dewailly E, Poirer P, Gingras S, Egeland GM. Comparison of diagnostic criteria of the metabolic syndrome in 3 ethnic groups of Canada. Metab Clin Exp. 2008; 57: 1526–32. 10.3402/ijch.v71i0.18698.
- Chateau-Degat ML, Dewailly E, Louchini R, Counil E, Noël M, Ferland A, et al.. Cardiovascular burden and related risk factors among Nunavik (Quebec) Inuit: insights from baseline findings in the circumpolar Inuit health in transition cohort study. Can J Cardiol. 2010; 26: 190–6. 10.3402/ijch.v71i0.18698.
- Chateau-Degat ML, Dewailly E, Noël M, Valera B, Ferland A, Counil E, et al.. Hypertension among the Inuit from Nunavik: should we expect an increase because of obesity?. Int J Circumpolar Health. 2010; 69: 361–72.
- Counil E, Julien P, Lamarche B, Château-Degat ML, Ferland A, Dewailly E. Association between trans-fatty acids in erythrocytes and pro-atherogenic lipid profiles among Canadian Inuit of Nunavik: possible influences of sex and age. Br J Nutr. 2009; 102: 766–76. 10.3402/ijch.v71i0.18698.
- Hopping BN, Erber E, Mead E, Roache C, Sharma S. High levels of physical activity and obesity co-exist amongst Inuit adults in Arctic Canada. J Hum Nutr Diet. 2010; 23(Suppl 1): 110–4. 10.3402/ijch.v71i0.18698.
- Lawn J, Harvey D. Change in nutrition and food security in two Inuit communities, 1992 to 1997. Ottawa: Indian and Northern Affairs Canada. 2001. 140. p.
- Liu J, Hanley AJG, Young TK, Zinman B. Characteristics and prevalence of the metabolic syndrome among 3 ethnic groups in Canada. Int J Obes. 2006; 30: 669–76. 10.3402/ijch.v71i0.18698.
- Nolin B, Lamontagne P, Tremblay A. Nunavik Inuit Health Survey 2004/Qanuippitaa? How are we? Physical activity, anthropometry and perception of body weight. Quebec: Institut National de Santé Publique du Québec and Nunavik Regional Board of Health and Social Services. 2007. 20. p.
- Bjerregaard P, Jørgensen ME, Andersen S, Mulvad G, Borch-Johnsen K. the Greenland Population Study. Decreasing overweight and central fat patterning with westernization among the Inuit in Greenland and Inuit migrants. Int J Obes. 2002; 26: 1503–10. 10.3402/ijch.v71i0.18698.
- Bjerregaard P, Jorgensen ME, Borch-Johnsen K. Cardiovascular risk amongst migrant and non-migrant Greenland Inuit in a gender perspective. Scand J Public Health. 2007; 35: 380–6. 10.3402/ijch.v71i0.18698.
- Bjerregaard P,the Greenland Population Study Group. Childhood conditions and education as determinants of adult height and obesity among Greenland Inuit. Am J Hum Biol. 2010; 22: 360–6.
- Jørgensen ME. Obesity and metabolic correlates among the Inuit and a general Danish population. Int J Circumpolar Health. 2004; 63(Suppl 2): 77–9.
- Jørgensen ME, Bjerregaard P, Borch-Johnsen K. Diabetes and impaired glucose tolerance among the Inuit population of Greenland. Diabetes Care. 2002; 25: 1766–71. 10.3402/ijch.v71i0.18698.
- Jørgensen ME, Glümer C, Bjerregaard P, Gyntelberg F, Jørgensen T, Borch-Johnsen K,the Greenland Population Study. Obesity and central fat pattern among Greenland Inuit and a general population of Denmark (Inter99): relationship to metabolic risk factors. Int J Obes Relat Metab Disord. 2003; 27: 1507–15. 10.3402/ijch.v71i0.18698.
- Jørgensen ME, Bjerregaard P, Gyntelberg F, Borch-Johnsen K;the Greenland Population Study. Prevalence of the metabolic syndrome among the Inuit in Greenland. A comparison between two proposed definitions. Diabet Med. 2004; 21: 1237–42. 10.3402/ijch.v71i0.18698.
- Jørgensen ME, Borch-Johnsen K, Bjerregaard P. Lifestyle modifies obesity-associated risk of cardiovascular disease in a genetically homogeneous population. Am J Clin Nutr. 2006; 84: 29–36.
- Jørgensen ME, Moustgaard H, Bjerregaard P, Borch-Johnsen K. Gender differences in the association between westernization and metabolic risk among Greenland Inuit. Eur J Epidemiol. 2006; 21: 741–8. 10.3402/ijch.v71i0.18698.
- Ebbesson SO, Schraer CD, Risica PM, Adler AI, Ebbesson L, Mayer AM, et al.. Diabetes and impaired glucose tolerance in three Alaskan Eskimo populations: the Alaska-Siberia Project. Diabetes Care. 1998; 21: 563–9. 10.3402/ijch.v71i0.18698.
- Ebbesson SO, Tejero ME, López-Alvarenga JC, Harris WS, Ebbesson LO, Devereux RB, et al.. Individual saturated fatty acids are associated with different components of insulin resistance and glucose metabolism: the GOCADAN study. Int J Circumpolar Health. 2010; 69: 344–51.
- Mohatt GV, Plaetke R, Klejka J, Luick B, Lardon C, Bersamin A, et al.. CANHR Research Team. The Center for Alaska Native Health Research Study: a community-based participatory research study of obesity and chronic disease-related protective and risk factors. Int J Circumpolar Health. 2007; 66: 8–18.
- Murphy NJ, Schraer CD, Bulkow LR, Boyko EJ, Lanier AP. Diabetes mellitus in Alaskan Yup'ik Eskimos and Athabascan Indians after 25 yrs. Diabetes Care. 1992; 15: 1390–2. 10.3402/ijch.v71i0.18698.
- Murphy NJ, Schraer CD, Thiele MC, Boyko EJ, Bulkow LR, Doty BJ, et al.. Dietary change and obesity associated with glucose intolerance in Alaska Natives. J Am Diet Assoc. 1995; 95: 676–82. 10.3402/ijch.v71i0.18698.
- Risica PM, Ebbesson SO, Schraer CD, Nobmann ED, Caballero BH. Body fat distribution in Alaskan Eskimos of the Bering Straits region: the Alaskan Siberia Project. Int J Obes Relat Metab Disord. 2000; 24: 171–9. 10.3402/ijch.v71i0.18698.
- Risica PM, Schraer C, Ebbesson SO, Nobmann ED, Caballero B. Overweight and obesity among Alaskan Eskimos of the Bering Straits Region: the Alaska Siberia project. Int J Obes Relat Metab Disord. 2000; 24: 939–44. 10.3402/ijch.v71i0.18698.
- Tejero ME, Voruganti VS, Cai G, Cole SA, Laston S, Wenger CR, et al.. Pleiotropic effects on subclasses of HDL, adiposity and glucose metabolism in adult Alaskan Eskimos. Am J Hum Biol. 2010; 22: 444–8. 10.3402/ijch.v71i0.18698.
- Bjerregaard P, Dewailly E, Young TK, Blanchet C, Hegele RA, Ebbesson SE, et al.. Blood pressure among the Inuit (Eskimo) populations in the Arctic. Scand J Public Health. 2003; 31: 92–9. 10.3402/ijch.v71i0.18698.
- Young TK, Bjerregaard P, Dewailly E, Risica PM, Jørgensen ME, Ebbesson SEO. Prevalence of obesity and its metabolic correlates among the circumpolar Inuit in 3 countries. Am J Public Health. 2007; 97: 691–5. 10.3402/ijch.v71i0.18698.
- Egeland GM, Pacey A, Cao Z, Sobol I. Food insecurity among Inuit preschoolers: Nunavut Inuit Child Health Survey, 2007–2008. CMAJ. 2010; 182: 243–8. 10.3402/ijch.v71i0.18698.
- Galloway T, Young TK, Egeland GM. Emerging obesity among preschool-aged Canadian Inuit children: results from the Nunavut Inuit Child Health Survey. Int J Circumpolar Health. 2010; 69: 151–7.
- Johnson-Down L, Egeland GM. Adequate nutrient intakes are associated with traditional food consumption in Nunavut Inuit children aged 3–5 years. J Nutr. 2010; 140: 1311–6. 10.3402/ijch.v71i0.18698.
- Niclasen BV, Petzold MG, Schnohr C. Overweight and obesity at school entry as predictor of overweight in adolescence in an Arctic child population. Eur J Public Health. 2007; 17: 17–20. 10.3402/ijch.v71i0.18698.
- Schnohr CW, Petersen J, Niclasen BVL. Onset of overweight in Nuuk, Greenland: a retrospective cohort study of children from 1973 to 1992. Obesity. 2008; 16: 2734–8. 10.3402/ijch.v71i0.18698.
- Schnohr CW, Sørensen TIA, Niclasen BVL. Changes since 1980 in body mass index and the prevalence of overweight among inschooling children in Nuuk, Greenland. Int J Circumpolar Health. 2005; 64: 157–62.
- National Centers for Health Statistics., Najjar MF, Rowland M. Anthropometric reference data and prevalence of overweight, Unites States, 1976–80. Vital Health Stat 11. 1987;238.
- Bray GA. Classification and evaluation of the obesities. Med Clin North Am. 1989; 73: 161–84.
- WHO. Physical Status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. WHO Technical Report Series 854. Geneva: WHO. 1995.
- WHO. Obesity: preventing and managing the global epidemic. Report of a WHO Expert Committee. WHO Technical Report Series 894. Geneva: WHO. 2000.
- WHO. Waist circumference and waist-hip ratio. Report of a WHO expert consultation. Geneva: WHO., 2008.
- Hiratsuka VY, Loo R, Will JC, Oberrecht R, Poindexter P. Cardiovascular disease risk factor screening among Alaska Native women: the traditions of the heart project. Int J Circumpolar Health. 2007; 66(Suppl 1): 39–44.
- Zammit MP, Kalra V, Nelson S, Broadbent BH, Hans MG. Growth patterns of Labrador Inuit youth: II. Skeletal age. Arctic Med Res. 1994; 53: 176–8.
- Becker-Christensen FG. Growth in Greenland: development of body proportions and menarcheal age in Greenlandic children. Int J Circumpolar Health. 2003; 62: 284–95.
- Sheikh N, Egeland GM, Johnson-Down L, Kuhnlein HV. Changing dietary patterns and body mass index over time in Canadian Inuit communities. Int J Circumpolar Health. 2011; 70: 511–9.
- Counil E, Dewailly E, Bjerregaard P, Julien P. Trans-polar-fat: all Inuit are not equal. Br J Nutr. 2008; 100: 703–6. 10.3402/ijch.v71i0.18698.
- Bjerregaard P, Pedersen HS, Mulvad G. The associations of a marine diet with plasma lipids, blood glucose, blood pressure and obesity among the Inuit in Greenland. Eur J Clin Nutr. 2000; 54: 732–7. 10.3402/ijch.v71i0.18698.
- Chateau-Degat ML, Dannenbaum DA, Egeland GM, Nieboer E, Laouan Sidi EA, Abdous B, et al.. A comparison of the metabolic response to abdominal obesity in two Canadian Inuit and First Nations populations. Obesity (Silver Spring). 2011; 19: 2254–60. 10.3402/ijch.v71i0.18698.
- Chateau-Degat ML, Dewailly E, Charbonneau G, Laouan-Sidi EA, Tremblay A, Egeland GM. Obesity risks: towards an emerging Inuit pattern. Int J Circumpolar Health. 2011; 70: 166–77.
- Shephard RJ, Hatcher J, Rode A. On the body composition of the Eskimo. Eur J Appl Physiol. 1973; 32: 3–15. 10.3402/ijch.v71i0.18698.
- Rode A, Shephard RJ. Prediction of body fat content in an Inuit community. Am J Hum Biol. 1994; 6: 249–54. 10.3402/ijch.v71i0.18698.
- Laurson KR, Eisenmann JC, Welk GJ. Body fat percentile curves for US children and adolescents. Am J Prev Med. 2011; 41(4 Suppl 2): S87–92. 10.3402/ijch.v71i0.18698.
- MazIcIoğlu MM, Hatipoğlu N, Oztürk A, Ciçek B, Ustünbaş HB, Kurtoğlu S. Waist circumference and mid-upper arm circumference in evaluation of obesity in children aged between 6 and 17 years. J Clin Res Pediatr Endocrinol. 2010; 2: 144–50. 10.3402/ijch.v71i0.18698.
- Lohman TG, Roche AF, Martorell RAnthropometric standardization reference manual. Champaign IL: Human Kinetics. 1988. 184. p.