Abstract
Background
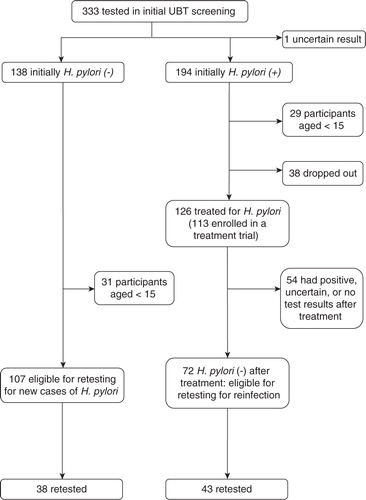
The Aklavik H. pylori Project (AHPP) (www.canhelpworkinggroup.ca) is a community-driven project examining Helicobacter pylori infection and its influence on health in a diverse Aboriginal community in the Northwest Territories. Initial research revealed that 58% of 333 participants who underwent a urea breath test (UBT) between 2007 and 2010 were H. pylori-positive. From 2008 to 2010, we offered treatment to H. pylori-positive participants and 113 consented to this treatment.
Objective
We estimated H. pylori incidence in AHPP participants who initially tested negative and the re-infection frequency in initially positive participants who were successfully treated to clear the infection.
Methods
Participants who were initially H. pylori-negative or negative after treatment during 2008–2010 were eligible for inclusion. From November 2011 to June 2012, participants were offered a UBT and the samples were analyzed using infrared spectroscopy (IRIS). Participants with a positive test result were classified as new cases for estimating incidence among participants testing negative at baseline and re-infection among those successfully treated for H. pylori infection.
Results
Among 38 initially negative participants, follow-up UBT showed that 33 remained negative, 3 were positive, and 2 had uncertain status. The estimated incidence proportion during the follow-up period was 8.3% (95% CI: 1.8–22.0%). Among 43 participants with a negative post-treatment UBT, 41 remained negative and 2 were positive. The estimated re-infection proportion during the follow-up period was 4.7% (95% CI: 0.6–16.0%). The frequency of new cases was similar in males and females. Aboriginal participants had a combined re-infection/incidence rate of 2.4% per year (95% CI: 0.8–5.9% per year). All 9 non-Aboriginal participants remained free from infection throughout the study period, as did all 23 participants aged 55 years and above.
Conclusions
The AHPP has substantially reduced the burden of infection in Aklavik since 2008. Continued monitoring, treatment, community engagement and knowledge translation activities are needed to ensure a lasting benefit of the project.
The Aklavik H. pylori Project (AHPP) is a community-driven project examining Helicobacter pylori infection and its influence on health in a diverse Aboriginal hamlet in the Northwest Territories, conducted by the Canadian North Helicobacter pylori (CANHelp) Working Group (http://www.canhelpworkinggroup.ca). The CANHelp Working Group brings together health care providers, Aboriginal government representatives, the Aklavik Health Committee (AHC), and University of Alberta researchers to address community concerns regarding the high prevalence of H. pylori infection in Aklavik and the association of this infection with stomach cancer.
Aklavik is an Arctic community of 633 people (according to the 2011 census) including predominately Inuvialuit and Gwich'in peoples, along with smaller numbers of Métis, other First Nations and non-Aboriginal residents. Overall project goals include investigating the impact of H. pylori infection on Canadian Arctic communities; identifying effective treatment strategies; developing recommendations aimed at H. pylori infection management; and effectively communicating research findings to address community concerns (Citation1, Citation2). Currently, there is no standard recommendation for community surveillance of H. pylori infection or, more generally, for testing and treating people who are not seeking medical care for relevant symptoms. However, the Maastricht IV/Florence Consensus Report (Citation3) on clinical management of H. pylori infection recommends that, “A screen-and-treat strategy of H. pylori should be explored in communities with a significant burden of gastric cancer.” With guidance from the locally organized AHC, the AHPP developed approaches to participant recruitment, enrolment, H. pylori screening, and treatment in order to provide answers to community questions about the infection and its potential health consequences. During initial project planning, the AHC wanted all residents of Aklavik to be invited to undergo screening for H. pylori infection and treatment to be made available to all participants testing positive. A treatment trial conducted from 2008 to 2010 was designed to accommodate this request as well as to find effective treatments for the strains of H. pylori that exist in Aklavik and generate information that may be useful to regional health authorities in future policy development.
Initial research revealed that of the 333 project participants who were screened between November 2007 and June 2010, 193 (58%) were H. pylori-positive by urea breath test (UBT). From 2008 to 2010, the project offered treatment to H. pylori-positive participants. The aim of this new project component is to estimate the H. pylori incidence and re-infection rates in Aklavik since the treatment component of the AHPP was conducted.
Background
H. pylori are gram-negative spiral-shaped bacteria uniquely adapted to live in the stomach lining of humans. H. pylori infection is often chronic and usually established during childhood. While a majority of those with chronic infection remain asymptomatic and free of disease consequences, it has been estimated that chronic H. pylori infection is responsible for more than 90% of peptic ulcer disease cases in developing countries where infection rates are high, and 65% of all gastric cancers worldwide (Citation4, Citation5). While the bacterium's pathogenic role in initiating gastritis, peptic ulcers and gastric cancers was described soon after H. pylori was identified in the late 20th century, H. pylori research in the public health sector has developed much more slowly. As the exact transmission pathway(s) remain unconfirmed, much current research aims to identify potential risk factors for specific populations and communities and to investigate the success and cost-effectiveness of particular surveillance and treatment programs.
Epidemiologic studies across the globe present a strong association of conditions, such as low socio-economic status (SES), low levels of education and marginalized ethnic status with H. pylori infection frequency (Citation6). Particularly in early life, poverty and related issues including household crowding are commonly associated with higher H. pylori prevalence (Citation7, Citation8). Relatively high prevalence of H. pylori infection today exists in southeast Asia, Africa, Central and South America, and throughout the Arctic. Over the past 10 years, we have learned that H. pylori infection and gastric cancers are much more frequent in the Arctic regions of the United States, Canada, Scandinavia and Russia compared to the southern, more urban regions of these nations; and in Greenland compared to Denmark (Citation9, Citation10).
Research in the AHPP has revealed that similar social issues including income, ethnic status, parent education level and household crowding are associated with H. pylori infection (Citation11). While we know that H. pylori is highly prevalent in several remote Arctic communities such as Aklavik, we know very little about H. pylori incidence and re-infection rates in the North. A systematic search reveals just one report of H. pylori incidence in northern Canada – from a follow-up study of Aboriginal children in northern Manitoba (Citation12) – and no reports on re-infection. As a large proportion of Aklavik's community participated in screening and treatment for H. pylori, we were able to design an incidence and re-infection study, having identified participants who were negative for infection at the start of the study period. Our aim in this analysis is to estimate the incidence of new H. pylori infections in AHPP participants who initially tested negative (baseline-negative) and the re-infection frequency in initially positive participants who were successfully treated during the project (H. pylori-cleared).
Methods
In 2008, the AHPP offered UBT screening to all Aklavik residents without restriction. During 2008–2010, 333 participants received a UBT to assess their infection status. The ages of the 333 project participants ranged from infancy to 80 years; 54% were female and 87% of them were Aboriginals (56% Inuvialuit, 27% Gwich'in and 4% other Aboriginal groups). A previous analysis compared demographic characteristics of project participants and the community population (Citation13). The characteristics of the community population of Aklavik were estimated by the community profile of 2006 census. The findings suggested that the study population was older and comprised a slightly greater proportion of females than the community population.
From 2008 to 2010, the AHPP offered treatment to H. pylori-positive participants and 113 consented to treatment. The details and results of the trial have been presented elsewhere (Citation14). Participants were randomized to receive either the standard triple therapy used across Canada (rabeprazole 20 mg po bid, amoxicillin 1 g po bid and clarithromycin 500 mg po bid for 10 days) or a sequential therapy (10 days of rabeprazole 20 mg po bid, days 1–5 amoxicillin 1 g po bid, days 6–10 clarithromycin 500 mg po bid and metronidazole 500 mg po bid), unless antibiotic susceptibility testing showed evidence of resistance to clarithromycin. For clarithromycin-resistant cases, individuals were randomized to receive either the sequential therapy or a quadruple therapy (10 days of bisthmuth 2 tablets qid, tetracycline 500 mg po qid, metronidazole 500 mg po tid and rabeprazole 20 mg po bid). Treatment success was assessed with a post-treatment UBT at least 10 weeks after the completion of treatment. Participants with treatment failures were treated again with a different regimen and reassessed at least 10 weeks after the completion of treatment.
For the new AHPP component aimed at estimating H. pylori incidence and re-infection rates, participants aged 15 years or above who were previously shown to be free of H. pylori infection were eligible for inclusion. All AHPP participants (n=179) who initially tested H. pylori-negative (n=107) or were negative after treatment (n=72) as of October 31, 2011 were invited to undergo a repeated UBT to classify their current H. pylori status. From November 2011 to June 2012, we offered participants UBT screening for H. pylori infection at the Susie Husky Health Centre in Aklavik. Breath samples were analyzed using infrared spectroscopy (IRIS) at the University of Alberta. We classified UBT results as positive (delta-over-baseline test values =4), negative (delta-over-baseline test values from −2 to 2.5) or borderline (test values between 2.5 and 4). For borderline results or breath samples with insufficient CO2 concentration, participants were asked to repeat the test. If a sample with a sufficient CO2 concentration could not be obtained, the result was considered unclassifiable and the participant was excluded from the analysis. When a repeat result was borderline, the borderline classification was retained. Participants with a positive test result were classified as new cases: incident cases in the baseline-negative group and re-infection cases in the H. pylori-cleared group.
We estimated two incidence measures: (a) the incidence proportion (the number of new cases divided by the number of infection-free participants who were retested for the incidence study) pertaining to the time between the negative UBT and the subsequent UBT and; (b) the incidence rate (the number of new cases divided by the person-time at risk). For estimating rates of incidence and re-infection events, we define the person-time at risk as the time period between the date of the last negative test and the date of the follow-up test for each person, subtracting half of this interval for participants with new infection onsets. We calculated the incidence rates by dividing the number of positive cases by the sum of person-time at risk.
Given its community-based research design, the AHPP is guided by community priorities. Previous analysis has shown that H. pylori infection is less frequent among non-Aboriginal community residents, and some community members requested that we examine whether there is a difference in infection frequency between the various Aboriginal groups residing in Aklavik (classified as “Inuvialuit,” “Gwich'in” and “other Aboriginal”). We report estimated incidence and re-infection frequencies with 95% confidence intervals (CI) for the total study population (n=79) and for demographic subgroups by age, sex and self-identified ethnicity. To compare incidence across groups, we estimated incidence rate differences and 95% CI. As individual follow-up periods vary, we do not compare incidence proportions in our analysis.
Results
We retested 81 participants for this study (). Of these 81, age at the entry into this study period ranged from 18 to 80 years (mean: 43, median: 44); 45 were female (56%) and 66 self-identified as Aboriginal (81%). Among the 38 participants who had tested negative on initial screening, 33 remained negative on the follow-up UBT, 3 were positive and 2 had uncertain results. In this group, the estimated incidence proportion during the follow-up period was 8.3% (95% CI: 1.8–22%). Among the 43 participants with a previous negative post-treatment UBT, 41 remained negative and 2 were positive. The estimated re-infection proportion during the follow-up period was 4.7% (95% CI: −0.6–16.0%). We report person-years and mean and median person years-at-risk in . As individual follow-up periods vary, we report both incidence proportions and rates, but only compared rates in our analysis.
Table I Frequency of new H. pylori infections among participants in the Aklavik H. pylori Project, Northwest Territories, Canada
Among the participants with follow-up results (n=79), the estimated rate of new cases was 2.1% per year () over an average follow-up of 3 years. Among people with a negative UBT at study entry, the estimated incidence rate was 1.8% per year; among people who had previously cleared an infection, the estimated re-infection rate was 2.4% per year. The rates in the 2 groups are similar, with the 95% CI for the rate difference of −0.6% per year comparing re-infection to new cases in those who were infection-free at baseline ranging from −4.2 to 3.0% per year.
Results across groups: sex, age, ethnicity
Among participants with classifiable follow-up results, incidence proportions and rates (combining new cases of infection in participants who were H. pylori-negative at baseline and those who were successfully treated) were estimated for categories of sex, age and self-reported ethnic status. The estimated incidence proportion for the follow-up period was 3.1% (95% CI: 0.1–16.0%) in males and 8.5% (95% CI: 2.4–20%) in females. The estimated incidence rate was 1.1% per year in males and 2.8% per year in females. The estimated incidence rate difference comparing males to females was −1.7% per year (95% CI: −5.1–1.7% per year).
Age cohorts were grouped by two-decade intervals starting at age 15 (15–34; 35–54; 55 and above). The rate of new cases declined notably by age: 7.3% per year (95% CI: 1.5–21.0% per year) in those aged 15–34; 1.6% per year (95% CI: 0.2–5.8% per year) in those aged 35–54; and 0 (97.5% CI: 0.0–5.0% per year) in those over age 55.
Aboriginal participants had a combined re-infection/incidence rate of 2.5% (95%CI: 0.8–5.9% per year), while all non-Aboriginal participants remained free from infection during the study period. Of 41 self-identified Inuvialuit participants, the rate of new cases was 3.3% per year (95% CI: 0.9–8.4% per year); among 24 self-identified Gwich'in participants the rate of new cases was 1.5% per year (95% CI: 0.4–8.2% per year). The estimated incidence rate difference comparing Gwich'in to Inuvialuit is −1.8% per year (95% CI: −6.1–2.5% per year); the wide CI indicates that this study is too small to accurately estimate the difference between these groups in the rate of new cases. The 2 participants who identified as “other Aboriginal” remained free from infection during the study period. Four out of 79 participants chose to not report their ethnic status.
Discussion
Among participants in the AHPP aged 15 years and above, we observed an incidence proportion of 6.3% over an average follow-up of 3 years. In this population, the rate of new cases of H. pylori infection declined notably with age and was similar in males and females. Of note, all participants in this study aged 55 years and above remained free from infection throughout the study period, as did all non-Aboriginal participants. Due to the low incidence of new cases, we do not have enough data in this population sample to precisely estimate differences between ethnic and age groups. More data are needed from additional Canadian Arctic communities so that we can increase the size of regional population samples.
In this study, we have shown evidence suggesting that most AHPP participants treated for H. pylori infection remained free of infection during the follow-up period. Thus, we can infer that there was a corresponding decrease in the prevalence of H. pylori infection, bringing the prevalence in Aklavik closer to the average seen in southern Canada. This suggests a potential for reducing the burden of infection in communities like Aklavik through the application of screen and treat programs with long-term follow up. Before recommending such a strategy at the community level, however, a full assessment of costs and benefits is needed. Widespread antibiotic treatment may pose a risk to populations by increasing antibiotic resistance among H. pylori strains as well as other bacteria in the community. Our choice to screen and offer treatment to all positive participants is the result of consultation and consensus-building with the AHC, and it is appropriate in this community for a number of reasons. The AHPP has documented that H. pylori infection is highly prevalent in Aklavik, as is severe chronic gastritis and precancerous conditions of the stomach. The pattern observed in Aklavik fits with the observation that men in regional centres of the Northwest Territories have three times the rate of gastric cancer compared to men across Canada (Citation15). The AHPP is part of a research program that is gathering similar data from other Canadian Arctic communities. In addition to assessing the burden of disease from H. pylori infection in this region, we will assess the cost-effectiveness of regional health care practices, which currently include testing for and treatment of H. pylori in patients presenting with a wide array of gastric symptoms that can be caused by factors other than H. pylori infection. The adoption of community health strategies aimed at reducing health risks from H. pylori infection requires careful generation and analysis of the full array of evidence that must be considered for effective public policy. An international analysis of reported re-infection rates estimated summary rates of 2.7% for developed countries (3,014 patients followed for 24–60 months) and 13% for developing countries (2,071 patients followed for 12–60 months) (Citation16, Citation17), but there is extensive variation within these groupings depending on the population studies. One study, for example, estimated the re-infection rate at 1.8% per year in a population of Brazilian patients with dyspeptic diseases (Citation18). The AHPP is one of a very few sources of data on H. pylori incidence and re-infection rates in the circumpolar north. Our literature search identified just one report from this region. A 2-year prospective study of urban Alaska Native gastroenterology patients aged 18 years or above yielded an estimated re-infection proportion following successful treatment for H. pylori infection of 5.1% at 4 months, increasing to 7.2% at 6 months, 10.3% at 1 year and 14.6% at 2 years (Citation19). Among Aklavik project participants who were treated for H. pylori infection, the estimated re-infection proportion was considerably lower at 4.7% over an average of 2.6 years at risk. Some of this difference may be attributable to differences between gastroenterology patients and a community-based study population as well as random variation; the Aklavik study population was younger on average than the Alaskan study population, so if H. pylori incidence decreases with age, differences in age distribution would not explain the observed difference re-infection frequencies. While H. pylori infection is generally more prevalent throughout North American Arctic communities for which we have data, compared to southern Canada and the United States, these findings suggest variation across Arctic communities, and demonstrate the need for data from additional communities to add to our knowledge of H. pylori infection and its related human health outcomes in the North.
Conclusions
This incidence and re-infection study indicates that the screening and treatment components of the AHPP have substantially reduced the prevalence of H. pylori infection among project participants since the treatment component began in 2008. The CANHelp Working Group is continuing to collect data on determinants of treatment success as well as benefits of treatment in order to achieve our collaborative team's goals of addressing community concerns about health risks from H. pylori infection, and ultimately reducing these risks. Participant follow-up in Aklavik combined with epidemiological and ethnographic assessments of associated risk factors, and on-going community engagement and knowledge translation activities, are continuing in order to assess the long-term implications of community-wide test-and-treat programs for controlling H. pylori infection.
Conflict of interest and funding
None of the authors have any conflicts of interest to report. Additional funding to support extended accommodation in Aklavik for the lead author was provided by the Arctic Institute of North America; the McMaster University Indigenous Health Research Development Program Graduate Scholarship, funded by the Canadian Institutes of Health Research Institute of Aboriginal People's Health; and by the McMaster University School of Graduate Studies. At the time this research was conducted, the CANHelp Working Group research program was supported by grants from the Canadian Institute of Health Research (RNF: 115031) and ArcticNet Network of Centres of Excellence. Karen J Goodman is a Health Senior Scholar supported by Alberta Innovates Health Solutions.
Acknowledgements
The AHPP is made possible through partnerships with territorial health authorities (NWT Health and Social Services; Stanton Territorial Health Authority; Beaufort-Delta Regional Health and Social Services Authority; and the Arctic Health Research Network); and local government and organizations (the Hamlet of Aklavik; the Aklavik Indian Band; the Aklavik Community Corporation, and the AHC). This study was developed in consultation with the AHC and approved by ethics review boards at the University of Alberta and McMaster University. The AHPP has current research licenses from the Aurora Research Institute for the NWT, as well as letters of support from the Aboriginal governance bodies and the Hamlet of Aklavik. Prior to publication, our results were shared with the AHC, who provided us with helpful feedback from a community perspective. The authors acknowledge several Aklavik community members: Aklavik resident Tammy Tyrrell for her excellent services as a field research assistant; the staff at the Susie Husky Health Centre and the Joe Greenland Centre; Adult Education Coordinator Katie McRae at the Aurora Learning Centre, and Principal Velma Illasiak and Vice-Principal Frank Galway of Moose Kerr School, Aklavik. Thank you, Quyanainni, and Mahsi cho, to everyone for making this study possible!
References
- Cheung J, Goodman KJ, Munday R, Heavner K, Huntington J, Morse J, etal. Helicobacter pylori infection in Canada's Arctic: searching for the solutions. Can J Gastroenterol. 2008; 22: 912–6.
- Huntington J, Goodman KJ, Munday R, Gordon G, Fletcher C, CANHelp Working Group . Strategies for communicating health research findings to members of an Arctic Aboriginal community. Am J Epidemiol. 2009; 169: S89.
- Malfertheiner P, Megraud F, O'Morain CA, Atherton J, Axon ATR, Bazzoli F, etal. Management of Helicobacter pylori infection: the Maastricht IV/Florence Consensus Report. Gut. 2012; 61: 646–64.
- Walker MM, Teare L, McNulty C. Gastric cancer and Helicobacter pylori: the bug, the host, or the environment?. Postgraduate Med J. 2008; 84: 169–70.
- Perry S, de Martel C, Parsonnet J, Brachman P. S, Abrutyn E. Helicobacter pylori. 2009; 4th edition, New York: Springer Press. 369–94. Bacterial infections of humans: epidemiology and control.
- Khalifa MM, Sharaf RR, Aziz RK. Helicobacter pylori: a poor man's gut pathogen?. Gut Pathog. 2010; 2: 1–12.
- Malcolm CA, MacKay WG, Shepherd A, Weaver LT. Helicobacter pylori in children is strongly associated with poverty. Strat Manag J. 2004; 49: 136–8.
- Wizla-Derambure N, Michaud L, Ategbo S, Vincent P, Ganga-Zandzou S, Turck D, etal. Familial and community environmental risk factors for Helicobacter pylori infection in children and adolescents. J Pediatr Gastroenterol Nutr. 2001; 33: 58–63.
- Goodman KJ, Jacobson K, Veldhuyzen van Zanten S. Helicobacter pylori infection in Canadian and related Arctic Aboriginal populations. Can J Gastroenterol. 2008; 22: 289–95.
- Goodman KJ, the CANHelp Working Group . Update on H. pylori infection in northern Canada. 2010. Circumpolar H. pylori Conference, Copenhagen; September 22.
- Aplin L, Fagan-Garcia K, Chang HS, Geary J, Goodman KJ, CANHelp Working Group . Household factors associated with Helicobacter pylori infection in Aklavik, Northwest territories. Am J Epidemiology. 2011; 173: S230.
- Sinha SK, Martin B, Sargent M, McConnell JP, Bernstein CN. Age at acquisition of Helicobacter pylori in a pediatric Canadian First Nations population. Helicobacter. 2002; 7: 76–85.
- Jayanthan J, Tweedie K, Lazarus L. A demographic analysis of Aklavik: a comparison between Statistics Canada community profiles and survey data from the CANHelp Working Group Aklavik H. pylori Project. November 2009. (Unpublished).
- Morse A, Goodman KJ, Munday R, Morse JW, van Zanten S, CANHelp Working Group . Aklavik H. pylori project treatment phase: seeking an effective therapy for a Canadian Arctic Hamlet. 2009. International Congress on Circumpolar Health, Yellowknife; July 11–14.
- Department of Health and Social Services, Government of the Northwest Territories. Cancer in the Northwest Territories, 1990–2000. 2003. A descriptive report, Yellowknife, NWT: Government of the Northwest Territories.
- Niv Y, Hazazi R. Helicobacter pylori recurrence in developed and developing countries: meta-analysis of 13C urea breath test follow-up after eradication. Helicobacter. 2008; 13: 56–61.
- Parsonnett J. What is the Helicobacter pylori global reinfection rate?. Can J Gastroenterol. 2003; 17(Suppl B): 46–8.
- Silva FM, Navarro-Rodriguez T, Barbuti RC, Mattar R, Hasimoto CL, Elsifh JN. Helicobacter pylori reinfection in Brazilian patients with peptic ulcer disease: a 5-year follow-up. Helicobacter. 2010; 15: 46–52.
- McMahon BJ, Bruce MG, Hennessy TW, Bruden DL, Sacco F, Peters H, etal. Re-infection after successful eradication of Helicobacter pylori: a 2-year prospective study in Alaska Natives. Aliment Pharmacol Therapeut. 2009; 23: 1215–23.