Abstract
Background
Even though vitamin D is mainly produced by exposure to sunlight, little is known regarding vitamin D levels in populations living in sub-Arctic areas with little or no daylight during winter.
Objective
We describe distributions of vitamin D3 and the prevalence of adequate levels in a population living above 63°N.
Design
We sampled 1,622 randomly selected subjects, aged 25–74 years, between January and May, 2009, as part of the Northern Sweden MONICA study (69.2% participation rate). By using HPLC, 25(OH) vitamin D3 was analysed. Levels used for definitions were deficient, D3<25 nmol/l (<10 ng/ml); insufficient, D3 25–49.9 nmol/l (10–20 ng/ml); and adequate, D3≥50 nmol/l (20 ng/ml).
Results
Mean (median) level of vitamin D3 was 65.2 (63.6) nmol/l in men and 71.0 (67.7) nmol/l in women. Adequate levels were found in 79.2%, more often in women (82.7%) than in men (75.6%). Only 0.7% of the population were vitamin D3–deficient but 23.1% of men and 17.1% of women had insufficient levels. Levels of vitamin D3 increased with age and insufficient status was most common among those aged 25–34 years, 41.0% in men and 22.3% in women.
If subjects using vitamin D-supplementation are excluded, the population level of D3 is 1–2 nmol/l lower than in the general population across sex- and age groups. There were no differences between the northern or the southern parts, between urban or rural living or according to educational attainment. Those subjects born outside of Sweden or Finland had lower levels.
Conclusion
The large majority living close to the Arctic Circle in Sweden have adequate D3 levels even during the second half of the dark winter. Subjects with D3 deficiency were uncommon but insufficient levels were often found among young men.
Vitamin D, primarily produced by skin exposure to sunlight, is required for optimal bone health. Deficiency contributes to osteoporosis, reduces muscular function and increases risks for falls and fractures. Beyond this, much attention has focused on vitamin D and its expected consequences for general health, survival and specific diseases, recently summed up in 2 systematic reviews (Citation1, Citation2). Although many diseases are more common and mortality higher (Citation3) with low levels of vitamin D, evidence for causality is often lacking. The US Preventive Service Task Force in 2015 concluded that treatment with vitamin D may reduce mortality but only in institutionalized elderly, and risk for falls, but not fractures (Citation2). A meta-analysis from 2014 found a small reduction of all-cause mortality after vitamin D supplementation among older adults (Citation1).
Living in the northern part of the world, even above the Arctic Circle, provides little or no sun exposure during the winter months. For some diseases, a gradient has been identified between prevalence of vitamin D deficiency and latitude, but results are ambiguous (Citation4). In Sweden, a marked increase in the incidence of hip fracture for every degree increase in latitude (Citation5) underscores the possibility of an interaction between high latitude, low vitamin D and ill health, although the etiology of hip fractures include many other factors.
In previous Nordic studies of the domestic population, mean values are generally adequate, the seasonal variation is significant and the prevalence of vitamin D deficiency is low (Citation6–Citation15) However, in specific populations such as immigrants, both insufficiency and deficiency are significantly more common and might affect both health and quality of life (Citation16, Citation17). Direct comparisons of contemporary vitamin D levels in the population across Europe are scarce but a large multicentre study from 2013 reported higher vitamin D levels with higher latitude in Europe (Citation18). A review on vitamin D in the Arctic population underscored the importance of traditional foods to avoid deficiency of vitamin D (Citation19).
Many reports describe the situation in the 1990s (Citation7, Citation8) (Citation11, Citation12) (Citation13, Citation14) (Citation15, Citation20) although few reports include men (Citation8, Citation12) (Citation13, Citation20), and some are based on case-control studies and not cohort studies (Citation6, Citation21) (Citation22). Other shortcomings are small studies and limited age spans. Since sun exposure is proposed to be the major determinant for adequate levels, it would be important to study the northernmost parts of the Scandinavian countries and Russia during the winter months when the sun does not rise above the horizon (Citation6, Citation22). A recent report from Greenland describes increasing vitamin D deficiency with transition to modernized foods (Citation23). Large cohort studies including both adult men and women could answer if modern day living with travelling for sun holidays, using solariums and taking vitamin D supplements would counterbalance the ever dark winter.
The aim of this study was to evaluate the levels of vitamin D in a representative adult population of northern Sweden (above latitude 63°N) in 2009.
Material and methods
Survey participants
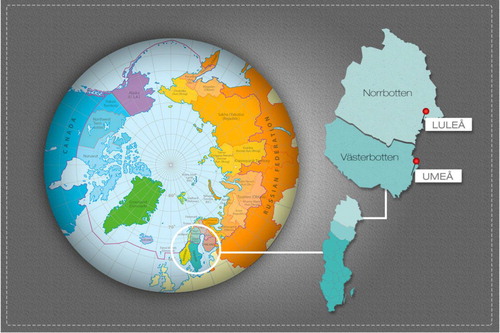
We used data from the Northern Sweden MONICA study, a population-based survey conducted in the 2 northern counties of Sweden with a target population of 312,000 inhabitants aged 25–74 years. In these counties, the 2 major population centres are Umeå at 63.8° N and Luleå at 65.6° N (). In total, 2,500 subjects aged 25–74 years were randomly selected from population registers and stratified for age and gender. Details of sampling and selection have been presented and data on non-participants have been published (Citation24, Citation25). The examinations were accomplished in January to April 2009. In total 1,729 subjects participated (69.2%).
Measurement and lab procedures
Details regarding examination and definition have previously been extensively described (Citation25). Questionnaires covering educational achievement, country of birth, type of residential area (Citation26) and current medication were administered.
Blood samples and lab
Blood samples were obtained after an overnight fast. Valid data on vitamin D were available in 1,622 subjects (94%), 50.1% men and 49.9% women. Blood samples for vitamin D (25-OH-vitamin D) were stored at −80°C, and analysed concurrently when all participants were screened. The method used for S-25(OH)D was HPLC (LC–MS/MS), the golden standard method for vitamin D analyses (Citation27–Citation29). Analyses were performed at a laboratory ascertained through DEQAS external controls. The method was calibrated with Chromsystems (Munich, Germany) calibrator for 25-OH-vitamin-D3 and 25-OH-vitamin-D2. The calibrator was directly traceable to NIST (National Institute of Standards and Technology, Gaithersburg, MD, USA). The method was also controlled with NIST SRM 972 and was within assigned values for both 25(OH)D3 and 25(OH)D2 in all 4 levels.
The limit of detection was 6 nmol/L. The inter-assay coefficients of variation (CVs) were 3% at 25D3 level 88 nmol/l and 2.6% at 25(OH)D3 level 177 nmol/l. The intra-assay CVs were 2.3% at 25(OH)D3 level 18 nmol/l and 1.7% at 25(OH)D3 level 48 nmol/l. Both 25(OH)D3 (cholecalciferol) and 25(OH)D2 (ergocalciferol) were quantified separately, but 25(OH)D2 values were low and detected only in 16 participants and therefore not included in the analyses. For readability, results of 25(OH)D3 were named vitamin D3 or just D3 in the text. Levels used for definitions were the current levels in Sweden and in accordance with the Institute of Medicine; deficient, D3<25 nmol/l (<10 ng/ml); insufficient, D3 25–49.9 nmol/l (10–20 ng/ml); and adequate, D3≥50 nmol/l (20 ng/ml) (Citation30, Citation31). One participant was excluded as an outlier with 295 nmol/l.
Statistical method
We report mean values and 95% confidence intervals of vitamin D3 levels for categorical variables and test for differences with ANOVA. Adjustment for age and gender was performed using univariate general linear models.
Ethics
The 2009 MONICA population survey is covered by ethical permission from Umeå University, number 08–106M.
Results
The age and sex distribution among the participants is presented in Table . The distribution of D3 in the population is presented in ; values range from 15 to 180 nmol/l. The mean level was 68.1 nmol/l, corresponding to 65.2 and 71.0 nmol/l, in men and women, respectively (p<0.001). The median level was 66 nmol/l, corresponding to 63.6 and 67.7, in men and women, respectively. When excluding subjects using vitamin D supplements (n=218), the mean level decreased among men to 64.8 and among women to 69.3 nmol/l. There were no significant differences in mean or median D3 levels between the 4 months of sampling.
Fig. 2. Distribution of vitamin D3 levels in the population of northern Sweden in 2009, aged 25–74 years.
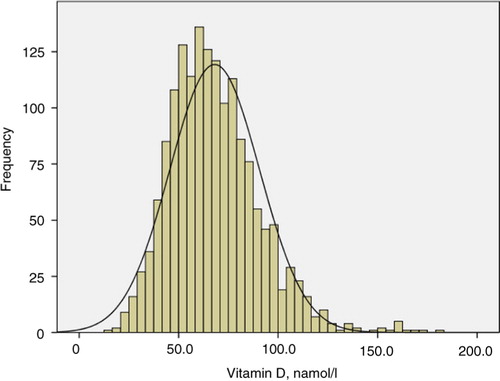
Table I. Age and sex distribution of participants in the Northern Sweden MONICA population survey 2009
Adequate levels of D3 (≥50 nmol/l) were found in 79.2%, more so in women than in men (Table , p<0.001). In men 23.1% were in the range defined as insufficient (D3 25.0–49.9 nmol/l) and in women 17.1%. Only 12 participants (0.7%) were D3-deficient (D3<25 nmol/l), 10 men and 2 women. There were no difference in the prevalence of D3 deficiency between months of survey and when excluding subjects using vitamin D supplements, prevalence of insufficiency did not change substantially.
Table II. Proportion of participants with deficient, insufficient or adequate levels of vitamin D3 according to gender (nmol/l)
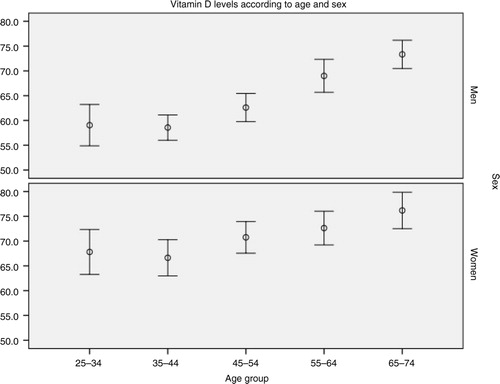
D3 levels increased with age (correlation r=0.19, p<0.001) and age group (, ANOVA linear test for trends, p<0.001 and p=0.002, for men and women, respectively). Insufficient levels were most common in the youngest age group (25–34 years), 41.0% in men and 22.3% in women.
Fig. 3. Mean levels of vitamin D3 in the population of northern Sweden in 2009 according to age, group and gender (bars mark 95% confidence intervals).
There were no differences in D3 between the northernmost county of Norrbotten and the more southern county of Västerbotten, the 2 regions sampled in the Northern Sweden MONICA Study, nor were there any differences in urban versus rural living (data not shown). Subjects born outside of Sweden or Finland, especially from outside of Europe, had lower D3 than native Swedes and Finns (p<0.001), but foreign-born subjects were few (n=53, Finland excluded). D3 did not differ according to level of education.
The 218 participants who reported supplementation with vitamin D had a mean D3 level of 75.6 nmol/l compared to 67.0 in those who did not use supplementation. After age and sex adjustment, vitamin D supplementation remained strongly associated with higher levels of vitamin D (p<0.001).
Discussion
Sun exposure is the most important source of vitamin D in some populations (Citation32). People living in the sub-arctic area of Sweden receive few or no hours of sun during winter. The sun never rises more than 30° over the horizon during winter, which is the limit under which there is no vitamin D production at all. Despite these facts, we found that D3 deficiency is very uncommon even during winter and that young men are those who are most D3 insufficient, up to 40%. Insufficiency occurs in about 20% of the population aged between 25 and 74 years. Supplementation with vitamin D contributed little to population levels. Notwithstanding, D-vitamin supplementation was strongly associated with higher levels although rarely used in this population.
To facilitate a comparison with other studies, a literature review was performed searching for population-based studies on D3 levels in Sweden (Citation9, Citation11) (Citation13, Citation14) (Citation20, Citation33), Norway (Citation6, Citation10) (Citation12), Finland (Citation8), Denmark (Citation7), Iceland (Citation15) and northern Russia (Citation22) (Table ). Even though many studies are old and include narrow age ranges, our population mean of 68 nmol/l is clearly above the large Danish (Citation7) and Norwegian studies (Citation12). Although very high D3 levels were reported from a Swedish case-control study (Citation13), these samples were from the 1980s and should be cautiously interpreted.
Table III. Studies from northern Europe on D3 levels (nmol/l) in the population sorted according to northern latitude
Vitamin D status has been extensively studied in Greenland over the past years and compared to people living in Denmark, both of Inuit and Danish origin (Citation23, Citation34–Citation36), and were recently reviewed (Citation37). Even though Greenlanders may have an enhanced renal production of vitamin D and an effective dermal production even at latitude of 70°N, a decrease in vitamin D levels has been found and explained by the less traditional Inuit diet.
Most studies focus on women, often post-menopausal, mirroring the previous narrow focus on bone health. Excluding the case-control study with young subjects (Citation13), 2 studies from Malmö stand out with high levels among women (Citation11, Citation14) and very low prevalence of insufficiency. Otherwise most studies in women (Citation6) (Citation8, Citation9) (Citation10, Citation12) (Citation15, Citation20) (Citation33) are in the range of 42–73 nmol/l. Extending the geographical area to Scotland (latitude 57°N), D3 levels in women were as low 28 nmol/l (Citation32). This leads us to conclude that among women in northern Sweden, the population mean of 71 nmol/l is high. This may possibly be explained by high consumption of fatty fishes, such as salmon, vitamin supplementation and sun bathing holidays during the winter although this was not measured in our study. We are well aware that direct comparison between studies is difficult due to separate assay methods, populations and secular trends, though.
The 4 cohort studies on men (Citation8, Citation12) (Citation20, Citation33) all report similar levels, ranging from 45 to 66 nmol/l, well in accordance with men in MONICA 2009 having 65 nmol/l.
In Table we sorted the studies according northern latitude but no clear trend in D3 according to a north–south gradient was found. However, among the most northerly studies is evident that northern Sweden has higher D3 levels than Tromsö (Citation6), the HUNT study from Mid-Norway (Citation12) and Iceland (Citation15). That more northern latitude does not necessarily lead to lower D3 levels was evident in a European multicentre study, using similar sampling and assays, where D3 increased from Italy to Finland and Sweden (Citation18). Perhaps this is due to dietary habits and vitamin D–supplemented food. In a large recent study from Greenland, higher latitude (ranging between 60 and 77°N) was associated with lower vitamin D levels (Citation35) and dermal production of vitamin D during sun exposure contributes strongly (Citation34).
In most studies, just as in MONICA, women have slightly higher levels of vitamin D. This may be due to more sunbathing (Citation6), outdoor activities (Citation6, Citation7), sun holidays (Citation9, Citation17) and a more frequent use of vitamin D supplementation among women (Citation9, Citation14).
A recent review discussed the common finding of vitamin D deficiency among northern native people (Citation21). However, it is important to keep in mind that although our study area is well within the circumpolar area, only approximately 5% of the inhabitants are of Sami descent (Citation38). The lower levels we found among participants born in countries outside Scandinavia is also well known (Citation17).
If there is no, or possible even an inverse, gradient between latitude and D3 in the population, both within Sweden and within Europe, how is this reconciled with the notion of sun exposure as the most important source of vitamin D? Northerners have lighter skin pigmentation, which allows greater vitamin D synthesis. Additional adaptions include sun-seeking behaviour and supplemented foods which could counterbalance the lack of sun. The finding of a north–south gradient in Greenland (Citation35) raises the possibility that modern, mainly urban, living diminishes the influence of sun exposure.
In the MONICA Study, D3 levels increased linearly with age and insufficiency was common among men 25–34 years of age, which is at odds with the HUNT Study where no age dependency was reported (Citation12). The MONICA Study is in accordance with a Finnish report on younger adults (Citation8) and Swedish women (Citation14). We did not evaluate the reason, but low dietary intake of D-vitamin, low use of D-vitamin supplementation and less travelling to sunnier regions among younger adults compared to older adults might contribute to this.
Strengths and limitations
When interpreting these studies on vitamin D, many methodological considerations must be taken into account. Choice of assay used to analyse vitamin D gives largely diverging results (Citation29). In contrast to many of the older studies, we used HPLC, the method seen as the gold standard (Citation28), using a laboratory with external quality control. However, the definition of vitamin D deficiency is controversial (Citation39, Citation40) and Sweden lacks a consensus though the definition in this study is recommended (Citation41). Many other studies have sampled throughout the year, but we collected our data between January and April so we probably measured the lowest values in the yearly variation (Citation7). Using the truly randomly selected population sample from the MONICA Study gives further credibility that our results have a high validity.
Data on sun exposure, diet, and travelling habits would have improved our analysis attempting to explain these finding but our limited scope was primarily to study the prevalence of insufficiency or deficiency of vitamin D in a northern population during the darkest part of the year.
Conclusion
The large majority of adults living close to the Arctic Circle in Sweden have adequate D3 levels even during the second half of the dark winter. Subjects with D3 deficiency were uncommon but insufficient levels were often found among young men. The causes of this must be the topic of further studies.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
Acknowledgements
The Northern Sweden MONICA Study is supported by the County Councils of Norrbotten and Västerbotten (“Spjutspetsanslag”) and the Joint Committee of County Councils in northern Sweden.
References
- Chowdhury R, Kunutsor S, Vitezova A, Oliver-Williams C, Chowdhury S, Kiefte-de-Jong JC, etal. Vitamin D and risk of cause specific death: systematic review and meta-analysis of observational cohort and randomised intervention studies. BMJ. 2014; 348: g1903.
- LeBlanc E, Chou R, Zakher B, Daeges M, Pappas M. Screening for vitamin D deficiency. systematic review for the U.S. Preventive Services Task Force Recommendation. 2014. [PubMed CentralFull Text] Report No.: 13-05183-EF-1. Rockville, MD: Agency for Healthcare Research and Quality.
- Johansson H, Oden A, Kanis J, McCloskey E, Lorentzon M, Ljunggren O, etal. Low serum vitamin D is associated with increased mortality in elderly men: MrOS Sweden. Osteoporos Int. 2012; 23: 991–9.
- Lips P. Worldwide status of vitamin D nutrition. J Steroid Biochem Mol Biol. 2010; 121: 297–300.
- Oden A, Kanis JA, McCloskey EV, Johansson H. The effect of latitude on the risk and seasonal variation in hip fracture in Sweden. J Bone Miner Res. 2014; 29: 2217–23.
- Brustad M, Alsaker E, Engelsen O, Aksnes L, Lund E. Vitamin D status of middle-aged women at 65–71 degrees N in relation to dietary intake and exposure to ultraviolet radiation. Public Health Nutr. 2004; 7: 327–35. [PubMed Abstract].
- Thuesen B, Husemoen L, Fenger M, Jakobsen J, Schwarz P, Toft U, etal. Determinants of vitamin D status in a general population of Danish adults. Bone. 2012; 50: 605–10.
- Lamberg-Allardt CJ, Outila TA, Karkkainen MU, Rita HJ, Valsta LM. Vitamin D deficiency and bone health in healthy adults in Finland: could this be a concern in other parts of Europe?. J Bone Miner Res. 2001; 16: 2066–73.
- Burgaz A, Akesson A, Oster A, Michaelsson K, Wolk A. Associations of diet, supplement use, and ultraviolet B radiation exposure with vitamin D status in Swedish women during winter. Am J Clin Nutr. 2007; 86: 1399–404. [PubMed Abstract].
- Olsen KS, Aksnes L, Frøyland L, Lund E, Rylander C. Vitamin D status and PUFA ratios in a national representative cross-section of healthy, middle-aged Norwegian women – the Norwegian Women and Cancer Post-Genome Cohort. Scand J Public Health. 2014; 42: 814–20.
- Gerdhem P, Ringsberg KA, Obrant KJ, Akesson K. Association between 25-hydroxy vitamin D levels, physical activity, muscle strength and fractures in the prospective population-based OPRA study of elderly women. Osteoporos Int. 2005; 16: 1425–31.
- Larose TL, Chen Y, Camargo CAJr, Langhammer A, Romundstad P, Mai XM. Factors associated with vitamin D deficiency in a Norwegian population: the HUNT Study. J Epidemiol Community Health. 2014; 68: 165–70.
- Littorin B, Blom P, Scholin A, Arnqvist HJ, Blohme G, Bolinder J, etal. Lower levels of plasma 25-hydroxyvitamin D among young adults at diagnosis of autoimmune type 1 diabetes compared with control subjects: results from the nationwide Diabetes Incidence Study in Sweden (DISS). Diabetologia. 2006; 49: 2847–52.
- Shirazi L, Almquist M, Malm J, Wirfalt E, Manjer J. Determinants of serum levels of vitamin D: a study of life-style, menopausal status, dietary intake, serum calcium, and PTH. BMC Womens Health. 2013; 13: 33.
- Sigurdsson G, Franzson L, Steingrimsdottir L, Sigvaldason H. The association between parathyroid hormone, vitamin D and bone mineral density in 70-year-old Icelandic women. Osteoporos Int. 2000; 11: 1031–5.
- Andersen R, Molgaard C, Skovgaard LT, Brot C, Cashman KD, Jakobsen J, etal. Pakistani immigrant children and adults in Denmark have severely low vitamin D status. Eur J Clin Nutr. 2008; 62: 625–34.
- Bjork A, Andersson A, Johansson G, Bjorkegren K, Bardel A, Kristiansson P. Evaluation of sun holiday, diet habits, origin and other factors as determinants of vitamin D status in Swedish primary health care patients: a cross-sectional study with regression analysis of ethnic Swedish and immigrant women. BMC Fam Pract. 2013; 14: 129.
- Deleskog A, Piksasova O, Silveira A, Gertow K, Baldassarre D, Veglia F, etal. Serum 25-hydroxyvitamin D concentration in subclinical carotid atherosclerosis. Arterioscler Thromb Vasc Biol. 2013; 33: 2633–8.
- Sharma S, Barr AB, Macdonald HM, Sheehy T, Novotny R, Corriveau A. Vitamin D deficiency and disease risk among aboriginal Arctic populations. Nutr Rev. 2011; 69: 468–78.
- Landin-Wilhelmsen K, Wilhelmsen L, Wilske J, Lappas G, Rosen T, Lindstedt G, etal. Sunlight increases serum 25(OH) vitamin D concentration whereas 1,25(OH)2D3 is unaffected. Results from a general population study in Goteborg, Sweden (The WHO MONICA Project). Eur J Clin Nutr. 1995; 49: 400–7. [PubMed Abstract].
- Frost P. Vitamin D deficiency among northern native peoples: a real or apparent problem?. Int J Circumpolar Health. 2012; 71 18001, doi: http://dx.doi.org/10.3402/ijch.v71i0.18001.
- Kozlov A, Khabarova Y, Vershubsky G, Ateeva Y, Ryzhaenkov V. Vitamin D status of northern indigenous people of Russia leading traditional and “modernized” way of life. Int J Circumpolar Health. 2014; 73 26038, doi: http://dx.doi.org/10.3402/ijch.v73.26038.
- Andersen S, Laurberg P, Hvingel B, Kleinschmidt K, Heickendorff L, Mosekilde L. Vitamin D status in Greenland is influenced by diet and ethnicity: a population-based survey in an Arctic society in transition. Br J Nutr. 2013; 109: 928–35.
- Stegmayr B, Lundberg V, Asplund K. The events registration and survey procedures in the Northern Sweden MONICA Project. Scand J Public Health Suppl. 2003; 61: 9–17.
- Eriksson M, Holmgren L, Janlert U, Jansson JH, Lundblad D, Stegmayr B, etal. Large improvements in major cardiovascular risk factors in the population of northern Sweden: the MONICA study 1986–2009. J Intern Med. 2011; 269: 219–31.
- Lindroth M, Lundqvist R, Lilja M, Eliasson M. Cardiovascular risk factors differ between rural and urban Sweden: the 20 09 Northern Sweden MONICA cohort. BMC Public Health. 2014; 14: 825.
- Zerwekh JE. Blood biomarkers of vitamin D status. Am J Clin Nutr. 2008; 87: 1087S–91S. [PubMed Abstract].
- Lai JK, Lucas RM, Banks E, Ponsonby AL, Ausimmune Investigator Group. Variability in vitamin D assays impairs clinical assessment of vitamin D status. Intern Med J. 2012; 42: 43–50.
- Snellman G, Melhus H, Gedeborg R, Byberg L, Berglund L, Wernroth L, etal. Determining vitamin D status: a comparison between commercially available assays. PLoS One. 2010; 5: e11555.
- Pearce SH, Cheetham TD. Diagnosis and management of vitamin D deficiency. BMJ. 2010; 340: b5664.
- Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, Clinton SK, etal. The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metabol. 2011; 96: 53–8.
- Macdonald HM, Mavroeidi A, Fraser WD, Darling AL, Black AJ, Aucott L, etal. Sunlight and dietary contributions to the seasonal vitamin D status of cohorts of healthy postmenopausal women living at northerly latitudes: a major cause for concern?. Osteoporos Int. 2011; 22: 2461–72.
- Deleskog A, Hilding A, Brismar K, Hamsten A, Efendic S, Ostenson CG. Low serum 25-hydroxyvitamin D level predicts progression to type 2 diabetes in individuals with prediabetes but not with normal glucose tolerance. Diabetologia. 2012; 55: 1668–78.
- Andersen S, Jakobsen A, Laurberg P. Vitamin D status in North Greenland is influenced by diet and season: indicators of dermal 25-hydroxy vitamin D production north of the Arctic Circle. Br J Nutr. 2013; 110: 50–7.
- Nielsen NO, Jorgensen ME, Friis H, Melbye M, Soborg B, Jeppesen C, etal. Decrease in vitamin D status in the Greenlandic adult population from 1987–2010. PLoS One. 2014; 9: e112949.
- Rejnmark L, Jorgensen ME, Pedersen MB, Hansen JC, Heickendorff L, Lauridsen AL, etal. Vitamin D insufficiency in Greenlanders on a westernized fare: ethnic differences in calcitropic hormones between Greenlanders and Danes. Calcif Tissue Int. 2004; 74: 255–63.
- Andersen S, Jakobsen A, Rex HL, Lyngaard F, Kleist IL, Kern P, etal. Vitamin D status in Greenland–dermal and dietary donations. Int J Circumpolar Health. 2013; 72 21225, doi: http://dx.doi.org/10.3402/ijch.v72i0.21225. eCollection 2013.
- Young TK. Circumpolar health atlas. 2012; Toronto: University of Toronto Press.
- Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, etal. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metabol. 2011; 96: 1911–30.
- Rosen CJ, Abrams SA, Aloia JF, Brannon PM, Clinton SK, Durazo-Arvizu RA, etal. IOM committee members respond to Endocrine Society vitamin D guideline. J Clin Endocrinol Metabol. 2012; 97: 1146–52.
- Lorentzon M, Akesson K, Mellström D, Landin-Wilhelmsen K, Pernow Y, Bergström I, etal. D-vitamin-behandling och skeletthälsa-svenska riktlinjer behövs-Rekommendationer från Svenska osteoporossällskapets kliniska expertgrupp. Lakartidningen. 2013; 111: 1508–10.