Abstract
Stercoral colitis with perforation of the colon is an uncommon, yet life-threatening cause of the acute abdomen. No one defining symptom exists for stercoral colitis; it may present asymptomatically or with vague symptoms. Diagnostic delay may result in perforation of the colon resulting in complications, even death. Moreover, stercoral perforation of the colon can also present with localized left lower quadrant abdominal pain masquerading as diverticulitis. Diverticular diseases and stercoral colitis share similar pathophysiology; furthermore, they may coexist, further complicating the diagnostic dilemma. The ability to decide the cause of perforation in a patient with both stercoral colitis and diverticulosis has not been discussed. We, therefore, report this case of stercoral perforation in a patient with diverticulosis and include a discussion of the epidemiology, clinical presentation, and a review of helpful diagnostic clues for a rapid differentiation to allow for accurate diagnosis and treatment.
Stercoral perforation of the colon is an uncommon life-threatening cause of the acute abdomen and must be recognized promptly to ensure proper treatment. Stercoral colitis may be asymptomatic or initial symptoms may be vague. When associated with an acute abdomen, the diagnosis becomes evident with diagnostic imaging by computed tomography (CT) scan. Diagnostic delay may result in perforation of the colon with peritonitis and septic shock (Citation1–(Citation4)). The primary differential diagnostic consideration is diverticulitis in a patient with left lower quadrant pain, and if there is right lower quadrant pain, it is appendicitis (Citation5, Citation6). Diverticular diseases and stercoral colitis share many pathological features (Citation1, Citation2) (Citation7, Citation8), and they can coexist in a patient, thus, further complicating the diagnostic dilemma. We report a case of stercoral perforation of the colon in a patient with diverticulosis.
Case report
A 55-year-old, postmenopausal woman was presented to the emergency department with a chief complaint of left lower quadrant pain, constipation, anorexia, nausea and vomiting of 4 days duration. Medical history was significant for chronic constipation, osteoarthritis, and seasonal allergies. She had a remote history of bilateral oophorectomy for benign ovarian cysts. Two years before the current admission, routine colonoscopy revealed only internal hemorrhoids. She denied smoking, drinking alcoholic beverages, or using street drugs. Her medications included calcium, vitamin D, acetaminophen, glucosamine, and chondroitin sulfate.
On physical examination, she had a pulse of 113/min, blood pressure of 108/72 mmHg, respiratory rate of 18/min, and temperature of 37°C. She had left lower quadrant distension and tenderness without rebound tenderness. The rectal examination revealed impacted stool. The remaining physical examination was unremarkable.
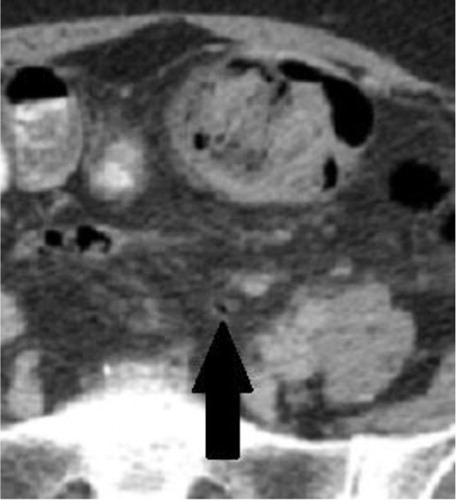
Laboratory studies included WBC 18,700/µL with 89.6% granulocytes, hemoglobin 13.4 g/dL, and platelet count 234,000/µL. The glucose, electrolytes, bicarbonate, lactate, and renal and liver function tests were all within normal limits. Blood cultures were obtained, which subsequently were negative. CT scan of the abdomen and pelvis with oral and intravenous contrast showed abundant stool in the colon, particularly in the sigmoid colon with surrounding extensive infiltrative changes, wall thickening, and 6.5 cm dilation of the colon (). There was sigmoid diverticulosis and multiple foci of extraluminal air ().
Fig. 1 Image depicting large fecal load, sigmoid wall thickening and extensive peri-colonic infiltrative change.

Fig. 2 Magnified image depicting a single focus of free air within the peritoneal cavity indicative of perforation. Peri-colonic infiltrative changes are also seen.
The patient was admitted to the medical service and given intravenous fluids, ciprofloxacin, and metronidazole. Oral Colace and tap water enemas were administered. On the third day of hospitalization, she complained of severe abdominal pain and had diffuse abdominal tenderness with rebound tenderness and further abdominal distension. Surgical consultation was obtained and an emergent exploratory laparotomy was performed which revealed extensive fecal peritonitis. The peritoneal cavity was thoroughly lavaged and a Hartmann procedure was performed with resection of the perforated sigmoid colon, creation of a proximal end colostomy, and closure of the rectal stump. The resected specimen was sent to the pathology department and peritoneal fluid was sent for cultures.
The pathology department received a 14.3×6.5×5.5 cm segment of colon focally covered with gray–green exudate and multiple adhesions. Gross examination showed a 2.0-cm perforation, which was 5.5 cm from one resection margin. A mucosal ulceration with an overlying fecaloma (hard localized accumulation of stool) was seen around the perforation. The mucosal surface of the colon also showed prominent pink–tan to red, congested circular folds and there were multiple diverticula. Microscopic examination showed a perforation of the colonic wall with mucosal necrosis, acute and chronic inflammation and granulation tissue ().
Fig. 3 Hematoxylin and eosin staining of colonic biopsy specimen showing acute and chronic inflammation.

Postoperatively, the patient was continued on intravenous antibiotics. The culture of the peritoneal fluid was positive for extended-spectrum beta-lactamase negative Escherichia Coli sensitive to cephalosporins and carbapenems. Her postoperative course was complicated by hospital-acquired pneumonia, which was successfully treated with intravenous cefepime. The patient was discharged on day 11 and prescribed intravenous ertapenem for 7 days.
Discussion
Stercoral perforation of the colon was initially described by Berry in 1894 (Citation9). Fewer than 90 cases were reported by the year 2000 (Citation1). However, it was the cause of 3.2% of colonic perforations in one series (Citation1) and present in 2.2% of randomly selected autopsy examinations (Citation10). Cases of stercoral perforation of the colon are likely both under-reported and are often not recognized. With an aging population and an increase in life expectancy, there are many people who survive with debilitating conditions. Sick elderly people, bed bound or minimally active, who are on multiple medications that affect bowel motility are prone to constipation. Long-standing constipation and fecaloma formation in the distal colon exert persistent pressure over the bowel wall leading to ischemic necrosis of the colonic mucosa and ultimately stercoral perforation (Citation1, Citation2). Old age, chronic constipation, abnormal bowel motility, and increased intraluminal colonic pressure underlie the pathogenesis of both stercoral colitis and diverticular diseases (Citation1, Citation2) (Citation7, Citation8). Despite some similarities in pathogenesis, the ability to differentiate the cause of perforation in a patient with both of these entities has not been addressed. The two disease processes are compared in .
Table 1 Comparison between stercoral perforation and diverticular disease
Both stercoral perforation and diverticular disease commonly occur in the sigmoid colon because this is the narrowest portion of the large intestine and stool gets progressively more dehydrated as water gets absorbed along the colon. These factors all contribute to significantly increased intraluminal pressure in the sigmoid colon (Citation1, Citation2) (Citation7, Citation8). Fecalomas have difficulty passing the relatively narrow rectosigmoid junction. At this location, they exert prolonged localized pressure and compromise microcirculation of the bowel wall, particularly over the antimesenteric aspect where the blood supply is poor. These events culminate in stercoral ulcer formation and perforation (Citation1, Citation2).
The clinical presentation of stercoral perforation and diverticulitis with or without perforation can be similar ( (Citation1, Citation2) (Citation3, Citation4) (Citation11) ). Stercoral perforation of the sigmoid colon usually presents with features of diffuse peritonitis and pneumoperitoneum (Citation4) but can present with localized peritonitis (17–20%) (Citation1, Citation2) and can masquerade as diverticulitis or diverticular perforation (Citation5). Signs of hollow viscus perforation mandate urgent exploratory laparotomy regardless of the cause; however, identifying the cause of localized peritonitis guides appropriate management. In contrast to diverticular perforations, stercoral perforations present with the proximal colon loaded with multiple fecalomas (63%). Inflammatory and necrotic process involves a longer segment of colon beyond the area of perforation. The perforations can be multiple (21–28%) (Citation1, Citation2). In selected cases of perforated diverticulitis, medical management or CT-guided percutaneous drainage is appropriate (Citation11). However, stercoral perforation mandates immediate surgical intervention (Citation1, Citation2).
In a patient with history of constipation, local or generalized peritonitis, palpable abdominal mass, stool impaction on rectal examination, pneumoperitoneum, fecal loading, or calcified feces on abdominal radiograph, a diagnosis of stercoral perforation should be considered (Citation2). Therefore, early CT scanning should be performed. CT scan findings of fecal impaction or fecaloma, focal thickening of colonic wall, stranding of pericolonic fat, and presence of extraluminal gas bubbles or an abscess can assist in the preoperative diagnosis of stercoral perforation with the latter three findings absent in simple fecal impaction (Citation3). Intraoperative findings and histologic examination confirm the diagnosis of stercoral perforation. The intraoperative findings include generalized peritonitis, fecaloma formation, colonic dilatation, edema of adjacent bowel wall, and ulcerations on the antimesenteric border usually measuring 1–10 cm, which are occasionally multiple (21–28%). If frank perforation occurs, fecal material is found within the peritoneal cavity in close proximity to the perforation site (Citation1, Citation2). Histopathological findings include ischemic necrosis and nonspecific inflammatory changes (Citation1, Citation2) (Citation10).
Surgical management of stercoral perforation includes open laparotomy, massive peritoneal lavage, and Hartmann's procedure with colostomy or segmental resection with primary anastomosis and diverting colostomy. The latter can be performed in patients with limited intraperitoneal septic condition and acceptable general condition and has the advantage of simple closure of diverting colostomy in future (Citation1, Citation4) (Citation17). In patients with stercoral perforation of colon, additional stercoral ulcers initially not visible may extend over a large colonic segment, bearing the risk of second perforation (Citation1). Substantial colonic dilation and the presence of multiple fecalomas may indicate additional stercoral ulcers (Citation1). In fact, stercoral perforation has been reported to recur proximal to an end colostomy (Citation18). Therefore, the management of the proximal colon should be a definitive part of the operative management (Citation2). Intraoperatively, colon disimpaction, colonoscopy, identification of additional stercoral ulcers, and removal of entire pathologically altered or dilated colon segments may avoid second perforation and further complications. Treatment of intra-abdominal sepsis can be achieved by massive peritoneal lavage, perforation control, and institution of broad-spectrum intravenous antibiotics. Peritoneal fluid culture in stercoral perforation is positive for gram-negative and anaerobic organism (e.g., E. coli, Enteroccocus faecalis, and B. fragilis), so patients should at least be treated with antibiotics effective against these organisms (Citation4).
A favorable outcome in the treatment of stercoral perforation depends on adequate resuscitation, generous removal of all diseased colonic tissue, extensive peritoneal lavage, aggressive therapy to counteract peritonitis, including broad-spectrum antibiotics, and appropriate treatment of any comorbid medical condition (Citation4).
Most importantly, fecaloma may be present for months to years, before they cause complications (Citation2), hence, chronic constipation and fecal impaction should be managed timely and adequately to avoid potential life-threatening complications.
Conclusion
Cases of stercoral perforation of the colon are likely to go unrecognized. High index of suspicion is needed to diagnose stercoral perforation of the colon in patients presenting with localized or generalized peritonitis. Early recognition of stercoral perforation in patients with concomitant diverticular diseases is important as it can help the physician to decide the appropriate treatment plan.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
References
- Maurer CA, Renzulli P, Mazzucchelli L, Egger B, Seiler CA, Buchler MW. Use of accurate diagnostic criteria may increase incidence of stercoral perforation of the colon. Dis Colon Rectum. 2000; 43(7): 991–8.
- Serpell JW, Nicholls RJ. Stercoral perforation of the colon. Br J Surg. 1990; 77(12): 1325–9.
- Heffernan C, Pachter HL, Megibow AJ, Macari M. Stercoral colitis leading to fatal peritonitis: CT findings. AJR Am J Roentgenol. 2005; 184(4): 1189–93.
- Huang WS, Wang CS, Hsieh CC, Lin PY, Chin CC, Wang JY. Management of patients with stercoral perforation of the sigmoid colon: Report of five cases. World J Gastroenterol. 2006; 12(3): 500–3.
- Park J, LaBella G, McDonough S, Tender PM, Isho M, Tangen L. A stercoral sigmoid ulcer masquerading as perforated diverticulitis. Am Surg. 2010; 76(3): 346–7.
- Hsiao TF, Chou YH. Stercoral perforation of colon: A rare but important mimicker of acute appendicitis. Am J Emerg Med. 2010; 28(1): 112.e1–2.
- Bassotti G, Chistolini F, Morelli A. Pathophysiological aspects of diverticular disease of colon and role of large bowel motility. World J Gastroenterol. 2003; 9(10): 2140–2.
- Morris CR, Harvey IM, Stebbings WS, Speakman CT, Kennedy HJ, Hart AR. Epidemiology of perforated colonic diverticular disease. Postgrad Med J. 2002; 78(925): 654–8.
- Berry J. Dilatation and Rupture of sigmoid flexure short report. BMJ. 1894; 1: 301.
- Grinvalsky HT, Bowerman CI. Stercoraceous ulcers of the colon: Relatively neglected medical and surgical problem. J Am Med Assoc. 1959; 171: 1941–6.
- Jacobs DO. Clinical practice. Diverticulitis. N Engl J Med. 2007; 357(20): 2057–66.
- Hollingworth J, Alexander-Williams J. Non-steroidal anti-inflammatory drugs and stercoral perforation of the colon. Ann R Coll Surg Engl. 1991; 73(6): 337–9.
- Patel VG, Kalakuntla V, Fortson JK, Weaver WL, Joel MD, Hammami A. Stercoral perforation of the sigmoid colon: Report of a rare case and its possible association with nonsteroidal anti-inflammatory drugs. Am Surg. 2002; 68(1): 62–4.
- Dubinsky I. Stercoral perforation of the colon: Case report and review of the literature. J Emerg Med. 1996; 14(3): 323–5.
- West AB, Losada M. The pathology of diverticulosis coli. J Clin Gastroenterol. 2004; 38(5 Suppl 1): S11–6.
- West AB. The pathology of diverticulitis. J Clin Gastroenterol. 2008; 42(10): 1137–8.
- Guyton DP, Evans D, Schreiber H. Stercoral perforation of the colon. Concepts of operative management. Am Surg. 1985; 51(9): 520–2.
- Serpell JW, Sen M, Giddins G, Nicholls RJ, Bradfield WJ. Stercoral perforation of the colon proximal to an end colostomy. Postgrad Med J. 1991; 67(785): 299–300.
