Abstract
Chronic obstructive pulmonary disease (COPD) is one of the leading causes of disability and death worldwide. COPD exacerbation is usually treated with antibiotics, systemic corticosteroids, and inhaled bronchodilators. We present a case of recurrent COPD exacerbation that was treated repeatedly with standard therapy. Dynamic expiratory computed tomography of the chest was done, which revealed concomitant tracheomalacia. COPD and tracheomalacia may coexist during recurrent exacerbations of COPD, and delayed diagnosis can be associated with severe comorbidities. Ordering the appropriate imaging may aid in the correct diagnosis and facilitate appropriate management.
Chronic obstructive pulmonary disease (COPD) is a common respiratory disease that carries substantial morbidity and mortality (Citation1). Acute COPD exacerbation accounts for frequent hospital admissions, relapses, and deaths during hospitalization or shortly thereafter (Citation2). In-hospital mortality rates of acute COPD exacerbation can be as high as 5.8%, and a 1-year mortality rates are up to 27.7% (Citation3). A recent postmortem analysis of the major causes of early death in hospitalized patients with COPD exacerbations included cardiac failure, pneumonia, pulmonary embolism, and respiratory failure (Citation4).
Tracheomalacia (TM) is an underrecognized condition that often escapes detection clinically and presents with non-specific symptoms such as cough, dyspnea, and recurrent infections, and can overlap with other pulmonary diseases such as asthma or COPD (Citation5, Citation6). Definitive diagnosis is crucial to avoid delayed diagnosis and the undesirable systemic side effects of corticosteroid therapy.
Case report
A 68-year-old woman presented with a 3-day history of dyspnea, wheezing, and productive cough. She used albuterol several times at home without relief. One-week prior to admission, the patient completed a 1-month course of a tapered corticosteroid regimen and gained 30 pounds. In addition, she had a 10-year history of multiple COPD exacerbations and was treated with multiple antibiotics and inhaled bronchodilators including Beta 2 agonists, long-acting muscarinic antagonist, and systemic corticosteroids. Her last hospitalization was 8 months prior to admission. She had no previous history of intubation, stridor, or reflux symptoms. Her modified Medical Research Council (mMRC) symptom score was 3. She had a 150 pack-year smoking history, but she quit smoking 1-month before. She sleeps in a seated position, and dyspnea occurs when she lies flat. She is chairbound because of her dyspnea. Her medical history was notable for hypertension, depression, obstructive sleep apnea, and end-stage renal disease on hemodialysis. Her medications included fluticasone/salmeterol, tiotropium, albuterol as needed, prednisone, and 3 L oxygen by nasal cannula, continuous positive airway pressure (CPAP) at night, simvastatin, diltiazem SR, and sertraline. The patient had completed pulmonary rehabilitation program 2 years before.
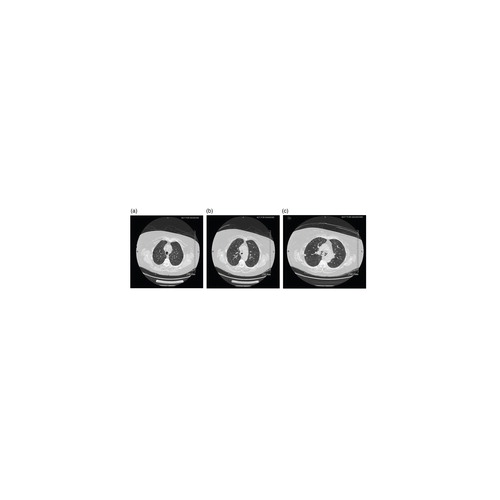
On physical examination at emergency department, she was alert and in moderate respiratory distress, with the following details: temperature 98.6 F, blood pressure 150/72, pulse rate 90/min, respiratory rate 26/min, and body mass index was 36 kg/m2. Oxygen saturation was 96% while breathing 6 L/min of oxygen by nasal cannula. General examination revealed Cushingoid facies and centripetal obesity. Cardiac examination revealed rapid regular rhythm without a murmur. Pulmonary examination revealed bilateral expiratory wheezing without pedal edema. Chest radiograph showed no infiltrates or congestion. ECG showed sinus tachycardia with non-specific ST changes. Laboratory studies revealed hemoglobin 11 g/dL, glucose 147 mg/dL, potassium 4.7 mEq/L, and creatinine 9.1 mg/dL. The patient was admitted with the diagnosis of exacerbation of COPD; received intravenous glucocorticoids, albuterol nebulizer treatments, bi-level positive airway pressure, and broad-spectrum antibiotics; and continued her scheduled hemodialysis. The patient's oxygenation and symptoms improved. Pulmonary function test (PFT) showed forced expiratory volume in 1 second/ forced vital capacity (FEV1/ FVC) ratio of 62% and FEV1 of 41% predicted. The Global initiative for chronic obstructive lung disease for classifying COPD by spirometry, the patient was considered to have a severe disease (GOLD 3). An alternative diagnosis of her dyspnea was pursued because of her recurrent symptoms despite appropriate previous treatments. A transthoracic echocardiogram showed a left ventricular ejection fraction of 70%, normal right ventricular function, Grade 1 diastolic dysfunction, and normal valves. Workup for thrombophilia was negative. A computed tomography (CT) soft tissue neck was unremarkable. A non-contrast dynamic expiratory chest CT revealed diffuse pulmonary emphysema, 11 mm right upper lobe pulmonary nodule and greater than 50% collapse in the distal trachea/multiple central bronchi and complete collapse of the bronchus intermedius, which is suggestive of tracheobronchomalacia (). The patient declined lung biopsy for the pulmonary nodule but agreed on silicone stent placement for her TM. A thoracic surgeon performed a bronchoscopy and placed a dynamic Y Boston scientific tracheobronchial stent. The patient went home the next day in stable condition. Arterial blood gases on discharge were as follows: pH 7.35, pCO2 47, and PO2 85 on oxygen at 3 L/min by nasal cannula. Her inhaler technique was good.
Fig. 1 (Left) Axial non-contrast computed tomography (CT) during inspiration showing a normal tracheal lumen. During expiration, axial non-contrast CT (center) showing thin crescent tracheal lumen and (right) both main stem bronchi (arrows).
The next day, she was found hypotensive and unresponsive by the emergency medical team. She was found to have acute hypoxic respiratory failure and admitted to the intensive care unit (ICU) for endotracheal intubation, intravenous vasopressors, systemic corticosteroids, broad-spectrum antibiotics, nebulized bronchodilator treatment, and mucolytic agents. Chest radiograph showed no infiltrates, edema, or pneumothorax and normal position of the tracheobronchial stent. Sepsis and myocardial ischemia were ruled out. The patient's COPD exacerbation improved. The patient wanted to be placed on home hospice and was discharged.
Discussion
Management of COPD exacerbation can be challenging. After excluding infection, congestive heart failure, and pulmonary embolism as causes of acute COPD exacerbation, patients are usually given systemic corticosteroid treatment, antibiotics, and bronchodilators. Many patients will experience systemic side effects of corticosteroids, such as hyperglycemia, weight gain, infections, myopathy, and/or adrenal insufficiency (Citation7). Treatment of recurrent COPD patients begins with confirmation of the diagnosis and consideration of other conditions that mimic COPD, especially when symptoms remain despite standard medical therapy (Citation5, Citation8–Citation10)). Our patient had advanced COPD disease (Stage D) based on her mMRC symptom score, GOLD spirometric classification, and recurrent hospitalizations. Her previous physicians were likely satisfied with the diagnosis of COPD as the etiology of her symptoms. However, a long delay in the correct diagnosis of TM may expose patients to extended courses of costly and potentially harmful treatment (Citation7). Long-term use of glucocorticoids and cigarette smoking are reported as risk factors for TM (Citation8).
Weak tracheal and main bronchial walls characterize tracheobronchomalacia. Normal intrathoracic airways dilate during inspiration and narrow during expiration due to changes in intrathoracic pressure. In patients with TM, expiratory narrowing is exaggerated. TM can be congenital or acquired, but it is more common in the latter. Common etiologies of acquired TM include prolonged intubation, tracheostomy, smoking, and external pressure on the trachea (e.g., substernal goiter) (Citation8).
The pathogenesis of TM is uncertain; however, limited autopsy data suggest that atrophy of longitudinal elastic fibers is a contributing factor. The prevalence of TM in adults is unknown; however, in bronchoscopies done in 4,283 patients with pulmonary disease, 12.7% of patients were found to have TM (Citation11).
TM and COPD may coexist. A retrospective review in stable patients with COPD who were imaged with inspiratory and dynamic expiratory multidetector CT found airway malacia in 38 of 71 patients (53%). Almost all TM cases (23/25, 92%) were characterized by an expiratory anterior bowing of the posterior membranous wall. In patients with advanced COPD, they may develop a distinctive form of TM in which distortion of the cartilaginous rings leads to lateral narrowing of the trachea, known as ‘saber-sheath’ trachea, which becomes exaggerated on exhalation (Citation12, Citation13). Management can be challenging when COPD coexists with TM because bronchodilators relax the smooth muscles in the airway and, therefore, may worsen airway collapsibility (Citation14).
TM is a form of dynamic airway collapse. Diagnosis can be easily missed with standard protocol lung images, and PFT has poor sensitivity for its diagnosis (Citation15). Bronchoscopy is a good diagnostic and therapeutic modality in evaluating pneumonia of unclear etiology, lung masses, or for foreign body removal, but it is not a common tool in management of COPD exacerbation. Once TM is suspected, patients should undergo dynamic expiratory CT or bronchoscopy with forced exhalation maneuvers to visualize the anterior bulging of the posterior tracheal wall that can lead to a crescent shape configuration (Citation16).
Treatment should be focused on treating coexisting conditions by optimizing medical regimen for COPD or asthma, smoking cessation, and pulmonary rehabilitation. CPAP can maintain an open airway; however, it does not alleviate dyspnea or cough. Silicone Y-shaped stents are preferred, and insertion requires rigid bronchoscopy and general anesthesia. Surgical repair has been described and tracheobronchoplasty improves quality of life, dyspnea, and functional status (Citation17).
Conclusion
TM and COPD may coexist during recurrent exacerbations of COPD, and delayed diagnosis can be associated with severe comorbidities. High index of suspicion is needed when patients with COPD remain symptomatic despite maximum standard medical therapy. Ordering the appropriate imaging or performing bronchoscopy may identify the disease in early stages and facilitate appropriate management.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
References
- Criner GJ, Bourbeau J, Diekemper RL, Ouellette DR, Goodridge D, Hernandez P, etal. Executive summary. Prevention of acute exacerbation of COPD: American College of Chest physicians and Canadian Thoracic Society guideline. Chest. 2015; 147(4): 883–93.
- Vestbo J. Hospitalized for chronic obstructive pulmonary disease: On a dangerous route. Respiration. 2013; 85: 11–12.
- Slenter RH, Sprooten RT, Kotz D, Wesseling G, Wouters EF, Rohde GG. Predictors of 1-year mortality at hospital admission for acute exacerbations of chronic obstructive pulmonary disease. Respiration. 2013; 85: 15–26.
- Zvezdin B, Milutinov S, Kojicic M, Hadnadjex M, Hromis S, Markovic M, etal. A postmortem analysis of major causes of early death in patients hospitalized with COPD exacerbation. Chest. 2009; 136: 376–80.
- Alici IO, Kurt OK, Dursun AB, Yilmaz A, Erkekol FO. Two cases of tracheal disease misdiagnosed as difficult-to-treat asthma. Respir Care. 2013; 58(11): e133–7.
- Demajumdar R, Rajesh PB. Have we got the full picture?. J Laryngol Otol. 1998; 112(8): 788–9.
- Niewoehner DE, Erbland ML, Deupree RH, Collins D, Gross NJ, Light RW, etal. Effect of systemic glucocorticosteroids on exacerbations of chronic obstructive pulmonary disease. N Engl J Med. 1999; 340: 1941–7.
- Solomon DA, Fanta CH, Levy BD, Loscalzo J. Clinical problem – Solving. Whistling in the dark. N Engl J Med. 2012; 366: 1725–30.
- Kumutala LA, Joshi M, Kamath H, Yarmush J. A surprising cause of wheezing in a morbidly obese patient: A case report. Int Med Case Rep J. 2014; 7: 143–5.
- Nagappan R, Parkin G, Wright CA, Walker CS, Vallance N, Buchanan D, etal. Adult long-segment tracheal stenosis attributable to complete tracheal rings masquerading as asthma. Crit Care Med. 2002; 30(1): 238–40.
- Ikeda S, Hanawa T, Konishi T, Adachi M, Sawai S, Chiba W, etal. Diagnosis, incidence, clinicopathology and surgical treatment of acquired tracheobronchomalacia. Nihon Kyobu Shikkan Gakkai Zasshi. 1992; 30: 1028–35.
- Kandaswamy C, Balasubramanian V. Review of adult tracheomalacia and its relationship with chronic obstructive pulmonary disease. Curr Opin Pulm Med. 2009; 15: 113–19.
- Sverzellati N, Rastelli A, Chetta A, Schembri V, Fasano L, Pacilli AM, etal. Airway malacia in chronic obstructive pulmonary disease: Prevalence, morphology and relationship with emphysema, bronchiectasis and bronchial wall thickening. Eur Radiol. 2009; 19: 1669–78.
- Panitch HB, Kekllkian EN, Motley RA, Wolfson MR, Schidlow DV. Effect of altering smooth muscle tone on maximal expiratory flows in patients with tracheomalacia. Pediatr Pulmonol. 1990; 9: 170–6.
- Majid A, Sosa AF, Ernst A, Feller-Kopman D, Folch E, Singh AK, etal. Pulmonary function and flow-volume loop patterns in patients with tracheobronchomalacia. Respir Care. 2013; 58: 1521–6.
- Lee KS, Sun MR, Ernst A, Feller-Kopman D, Majid A, Boiselle PM. Comparison of dynamic expiratory CT with bronchoscopy for diagnosing airway malacia: A pilot evaluation. Chest. 2007; 131: 758–64.
- Ernst A, Majid A, Feller-Kopman D, Gruerroro J, Boiselle P, Loring SH, etal. Airway stabilization with silicone stents for treating adult tracheomalacia: A prospective observational study. Chest. 2007; 132: 609–16.
