1 Case presentation
A 37-year-old male patient presented to the surgical outpatients department with undefined lower abdomen pain for a period of seven months associated with mucoid diarrhea. For the last two months, he had severe dysuria with suprapubic pain, and he also noticed air in the urine during micturition. He was admitted to the urology department two months ago for urinary tract infection which was treated with antibiotics. He also gave a history of perianal abscess drainage one year ago. The patient admitted to taking a course of antibiotics whenever he had an attack of urinary tract infection. There was no history of diabetes, hypertension, or any other chronic illness. There was no family history of the same illness or complaints. Physical examination showed suprapubic tenderness. His routine biochemical tests and tumor markers were normal except for evidence of pus cells, RBCs, epithelial cells, and mucus in urine examination. Ultrasound, computed tomography (CT) scan, MRI, and colonoscopy were performed.
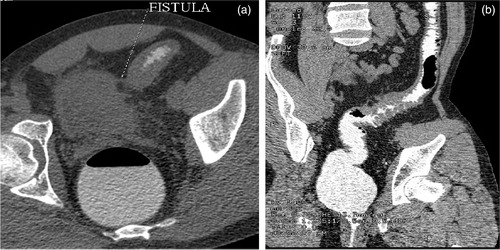
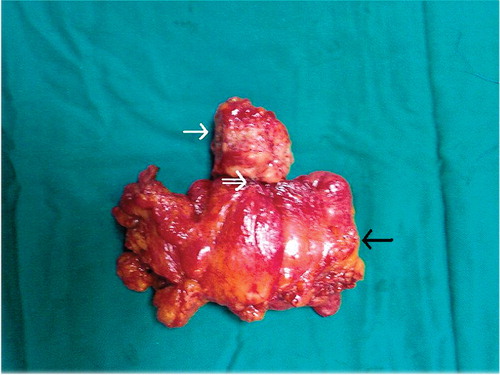
The patient underwent laparotomy which confirmed the CT scan findings. One-stage partial sigmoidectomy was done with excision of the sigmoidovesical fistula (SVF) and part of the urinary bladder ().
2 What is the diagnosis?
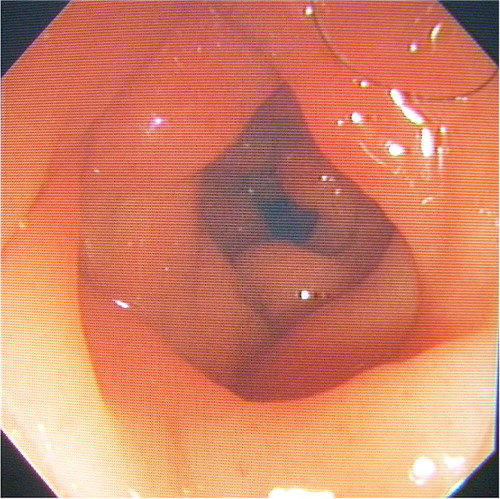
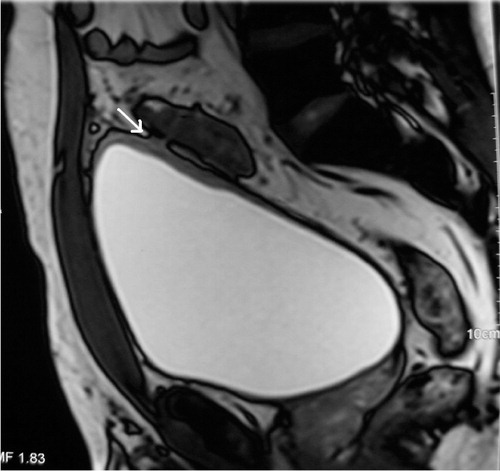
Ultrasonography of the pelvis () revealed thickened sigmoid (S) with extravasation of air into SVF (arrow), (B = urinary bladder). There was also an air-filled tract extending from the subjacent sigmoid colon with evidence of sigmoid colonic inflammation. Magnetic resonance imaging (MRI) of the pelvis () shows the apposition of sigmoid colon to the bladder wall (white arrow) but could not demonstrate the cause of pneumaturia and hence, a CT scan with per-rectal contrast was performed (a and b) which revealed an 18 cm length of inflamed sigmoid colon with multiple small diverticuli with pericolic inflammation and a SVF. Colonoscopy () revealed fleshy, indurated masses and small diverticuli in the sigmoid colon. The biopsies from the site revealed inflammatory changes and were negative for malignancy. In , excised specimen is the inflamed sigmoid colon segment (black arrow) and the bladder dome (white arrow) with SVF (double arrow). The patient had smooth recovery and was discharged in good general condition. Histopathological examination of the surgical specimen confirmed the imaging diagnosis.
Figure 1. Ultrasound reveals thickened sigmoid (S) with extravasation of air into SVF (arrow). (B = Urinary bladder).
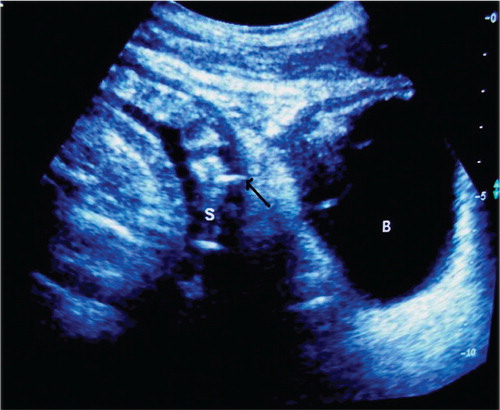
Figure 2. MRI shows the apposition of sigmoid colon to the bladder wall (white arrow). Fistula was not detected.
3 The diagnosis is
Diverticulitis complicated by SVF.
4 Discussion
Colonic diverticulitis occurs when diverticula within the colon become infected or inflamed. Acute diverticulitis is a disease with a wide clinical spectrum, ranging from a phlegmon (Stage Ia), to localized abscesses (Stages Ib and II), to free perforation with purulent (Stage III) or feculent peritonitis (Stage IV). In late stages, patients may present with complications like colovesical fistula (CVF). Other causes of CVF are colonic carcinoma and Crohn's disease. A high index of suspicion is required in patients who have non-specific symptoms where clinical diagnosis is difficult in order to avoid a significant delay in arriving at the correct diagnosis. The clinical diagnosis is often difficult to make and several radiological studies have been used over the past decades to clinch the diagnosis. These include barium enema, water-soluble contrast enema, ultrasound, and CT. Recently, MRI has been extensively used to evaluate this condition. With the advent of multidetector CT with its multiplanar reformation capability, this modality has surpassed all the other imaging techniques in its ability to demonstrate not only the extent of intramural inflammation, but also the degree of pericolic disease and accurate demonstration of the presence and site of unusual complications like CVF Citation1. Ultrasound remains the first line of investigation and can demonstrate colonic wall thickening and CVF, as in our case.
However, as it is operator dependent and subjective, we recommend a CT scan with per-rectal water-soluble contrast medium as the second line of investigation followed by colonoscopy. However, most of the studies published after 2005 have focused on the role of CT in the early diagnosis of acute colonic diverticulitis and its complications Citation2Citation3Citation4. Pneumaturia is sometimes the first symptom of CVF and should always raise the suspicion of this rare complication.
Surgery is the best treatment option with multiple surgical techniques like resection and primary anastomosis, hemicolectomy, one-stage colectomy with partial cystectomy, laparoscopic resections, diverting colostomy, or Hartmann intervention. In our center, primary resection of sigmoid colon with partial cystectomy and colorectal anastomosis performed as a one-step procedure is the treatment of choice, with an acceptable risk of anastomotic leak and mortality.
5 Conflict of interest and funding
The authors have not received any funding or benefits from industry to conduct this study.
References
- Sarma D, Longo WE. Diagnostic imaging for diverticulitis. J Clin Gastroenterol. 2008; 42: 1139–41.
- Sebastii Cerqueda C, Merino Peita E, Quiroga Gomez S, Alvarez-Castells A. Vesicosigmoid fistulas secondary to diverticulitis: helical CT diagnosis. Radiologia. 2007; 49: 343–5.
- Martin Aricvalo J, Garcia-Granero E, Garcia Botello S, Muitoz E, Cervera V, Flor Lorente B, et al.. Early use of CT in the management of acute diverticulitis of the colon. Rev Esp Enferm Dig. 2007; 99: 320–4.
- Kaewlai R, Nazinitsky KJ. Acute colonic diverticulitis in a community-based hospital: CT evaluation in 138 patients. Emerg Radiol. 2007; 13: 171–9.