Abstract
Acute myelopathy with sudden paraplegia is a very rare manifestation of meningococcal meningitis, with only a few cases reported in the literature. In almost all previously reported cases, other clinical manifestations of meningitis, such as fever, headache, and neck stiffness preceded acute myelopathy. In this paper, we report a case of acute myelopathy with sudden paraplegia as the sole manifestation of meningococcal meningitis, in the absence of other clinical manifestations of meningitis.
Introduction
Neisseria meningitidis, a gram-negative diplococcus, is a common pathogen associated with bacterial meningitis. Well-known neurological complications of meningococcal meningitis include brain edema, obstructive hydrocephalus, cranial nerve palsies, and septic shock Citation1Citation2. Acute myelopathy with sudden paraplegia is a very rare complication of N. meningitidis infection with only a few cases reported in the literature Citation2Citation3. Most of the previously reported cases of acute myelopathy complicating meningococcal meningitis develop during or following treatment for meningitis. In this paper, we report acute myelopathy as the sole manifestation of meningococcal meningitis in the absence of other manifestations, such as fever, headache, and neck stiffness.
2 Case report
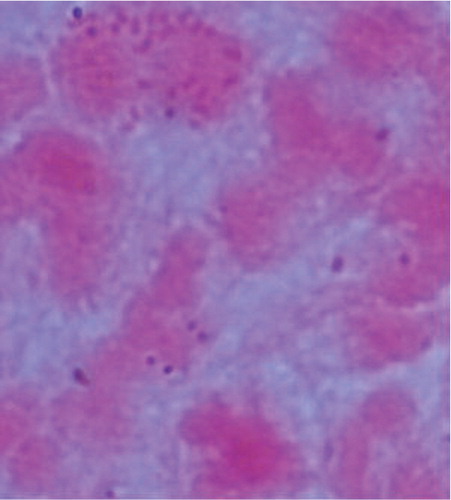
A 28-year old previously healthy male was referred to Hamad General Hopsital with six days history of low back pain and one day history of lower limb weakness and urinary retention. The weakness was acute and the patient was unable to move his lower limbs. He denied any history of fever, headache, photophobia, or neck pain. He worked as a camel keeper and denied any history of trauma to the back. Examination at admission revealed normal temperature, absence of signs of meningeal irritation, with normal cranial nerves and fundus examination. His chest, heart, and abdominal examinations were normal apart from distended urinary bladder. Lower limb examination revealed flaccid paraplegia with grade 0/5 power in lower limbs, absent reflexes, and equivocal plantar response. Last normal sensory level was T4. Complete blood count, urea, electrolytes, and two sets of blood culture were normal. Magnetic resonance imaging (MRI) of the spinal cord before and after gadolinium revealed long segment of intramedullary spinal cord T2 abnormal subtle bright signal with element of post-contrast spotty enhancement extending from T5 level to the tip of the conus medullaris impressive of transverse myelitis (). Cerebrospinal fluid (CSF) examination revealed hazy appearance with white cell count of 165/µl (with majority of cells being lymphocytes), protein of 1.15 g/l, and glucose of 2.2 mmol/l. Gram staining of the CSF revealed gram-negative intracellular diplococci impressive of N. meningitidis (). Latex bacterial antigen detection for the CSF sample was positive for N. meningitidis ABCYW135; however, CSF culture did not grow any organism. The patient was initially started on ceftriaxone 2 g bid for 10 days and 1 g of intravenous methylprednisolone for five days. Two cycles of plasmapharesis were then performed after showing no improvement with corticosteroid therapy. Bladder and bowel care, in addition to physiotherapy were continued. Despite all these therapies, there was no improvement in his lower limb and bladder condition at one month.
3 Discussion
Bacterial meningitis generally manifests with acute-onset fever, generalized headache, vomiting, and stiff neck. Myalgias (particularly in meningococcal disease), backache, and generalized weakness are common symptoms. The illness usually progresses rapidly with development of confusion, obtundation, and loss of consciousness. Complications of bacterial meningitis include cranial nerve palsies, sensorineural hearing loss, brain edema resulting in seizures, reduced consciousness or coma, dilated and poorly reactive pupils, decerebrate posturing, hypertension, bradycardia, and irregular respirations. It may also lead to temporal lobe herniation in some cases. Focal cerebral signs (principally hemiparesis, dysphasia, visual field defects, and gaze preference) occur in a considerable number of patients. Spinal cord dysfunction is a very rare complication of bacterial meningitis and its occurrence is limited to case reports only Citation2Citation3Citation4Citation5. Reported mechanisms for spinal cord dysfunction include infarction due to vasculitis, direct infection of the cord with abscess formation, and immune-mediated inflammatory myelopathy (myelitis) Citation2Citation3Citation4Citation5Citation6. Among bacteria causing meningitis, N. meningitidis and Streptococcus pneumoniae are the most frequent bacterial pathogens associated with spinal cord involvement Citation4Citation7. Myelitis during bacterial meningitis has been rarely reported and seems to have unfavorable prognosis with persistence of paresis, and bladder and bowel incontinence Citation4. Most of the cases of spinal cord dysfunction associated with bacterial meningitis occur during treatment or as a late complication of bacterial meningitis Citation2Citation4. In our case, spinal cord dysfunction as the initial and sole manifestation of meningococcal meningitis (in absence of fever, neck stiffness, and other manifestations of meningitis) makes it an unusual and unique case. Furthermore, the presence of meningococci in the CSF and the positive latex agglutination test for meningococci confirm the implication of these organisms in the pathology of spinal cord dysfunction. Two important findings that are not fully understood in this case are the presence of lymphocytosis in the CSF and the negative CSF culture. Although our laboratory did not specify the exact percentage of lymphocytes in CSF, it was reported to be a majority. One explanation was that the patient might have received an antibiotic by referring doctor prior to arrival at our hospital. Unfortunately, we could not contact the referring doctor for confirmation. Another explanation was that the spinal cord involvement might be merely an immune-mediated complication to the presence of meningococci, similar to that seen in idiopathic transverse myelitis. Nevertheless, the gram stain result and the positive latex agglutination test confirm the presence of meningococci in the CSF of this patient. The lower limb weakness and bladder involvement in our patient did not improve with corticosteroid and plasmapharesis therapy suggesting unfavorable prognosis.
4 Conclusion
Acute myelopathy may be the sole manifestation of meningococcal meningitis and it may have an unfavorable prognosis. Immune-mediated reaction to certain microorganisms may be implicated in the pathogenesis of some spinal cord diseases like idiopathic transverse myelitis. This may constitute a fruitful field for future studies.
5 Conflict of interest and funding
The authors have not received any funding or benefits from industry to conduct this study.
References
- Tunkle AR, Scheld WM. Acute bacterial meningitis. Lancet. 1995; 346: 1675–80.
- Rathore MF, Gill ZA, Malik AA, Farooq F. Acute flaccid paraplegia: a rare complication of meningococcal meningitis. Spinal Cord. 2008; 46: 314–6.
- Choudhuary N, Kumar N, Ahlawat R, Jain K, Rizvi Y, Agrawal G, et al.. Meningococcal meningitis with myelopathy: case report and review of literature. Cent Eur J Med. 2007; 2: 122–7.
- Kastenbauer S, Winkler F, Fesl G, Schiel X, Ostermann H, Yousry TA, et al.. Acute severe spinal cord dysfunction in bacterial meningitis in adults. Arch Neurol. 2001; 58: 806–10.
- Kan J, Altafullah I, Ishaq M. Spinal cord dysfunction complicating meningococcal meningitis. Postgrad Med J. 1990; 66: 302–3.
- Bhojo A, Akhter N, Bakshi R, Wasay M. Thoracic myelopathy complicating acute meningococcal meningitis: MRI findings. Am J Med Sci. 2002; 323: 263–5.
- Moffett KS, Berkowitz FE. Quadriplegia complicating Escherichia coli meningitis in a new born infant: case report and review of 22 cases of spinal cord dysfunction in patients with acute bacterial meningitis. Clin Infect Dis. 1997; 25: 211–4.