Abstract
Sclerosing encapsulating peritonitis (SEP) is a rare but serious complication of abdominal surgery, recurrent peritonitis, and continuous ambulatory peritoneal dialysis with a high morbidity and mortality. The etiology of this condition is largely unknown. Diagnosis is usually established at laparotomy in patients with recurrent attacks of non-strangulating, small bowel obstruction. We report a case of a patient who presented with intestinal obstruction and who showed typical CT findings of SEP which was diagnosed pre-operatively on a CT scan and confirmed at surgery. The interest of this case lies in its rarity and difficult pre-operative diagnosis.
Introduction
Sclerosing encapsulating peritonitis (SEP) is a dramatic complication of chronic peritoneal inflammation involving both visceral and parietal layers of the peritoneal cavity. A thickened peritoneum encloses the small intestine like a ‘cocoon’ and causes intestinal obstruction. A pre-operative diagnosis is difficult. Our report describes the imaging findings of this rare complication.
2 Case report
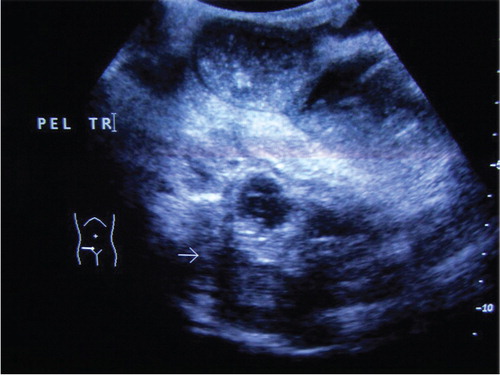
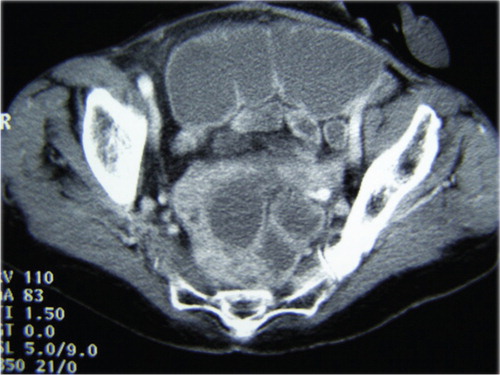
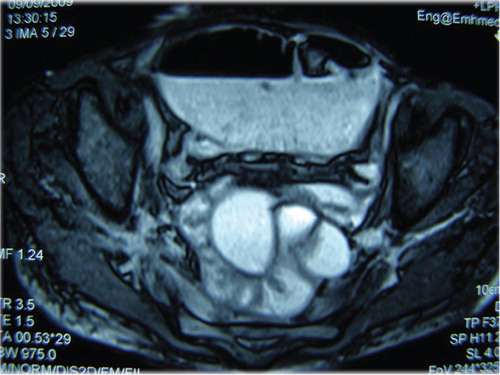
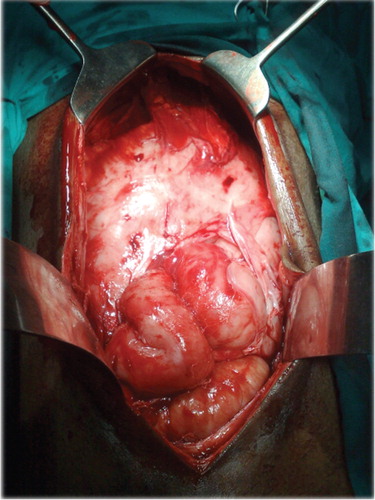
A 42-year-old Libyan female patient had been diagnosed as CA rectum (T3N1M0) and had undergone ‘R0’ A-P resection on 31 May 2009 in Tunisia. The tumor had accidentally perforated during the surgery with spillage into the peritoneal cavity. For this reason, she had received chemotherapy and adjuvant radiotherapy after the surgery. In the immediate post-operative period, she had an episode of peritonitis which was treated conservatively. She had been complaining of vague lower abdominal pain since then off and on. Now, she presented to the surgical out-patients’ department with acute intestinal obstruction. Her routine investigations were normal and the colostomy was functional. An erect abdominal X-ray showed dilated small bowel loops with multiple fluid levels. Ultrasound showed dilated small bowel loops with sluggish peristalsis and a thickened, irregular ‘sac-like’ structure in the midline in pelvis encasing small bowel loops (). CT scan and MRI had already been done in another hospital and showed congregated small bowel loops in the pelvis encased in a thick capsule with dilated small bowel loops ( and ). A diagnosis of SEP was considered on imaging. At laparotomy, it was found that a considerable length of the distal small bowel 30-cm proximal to the ileocecal valve was encased in a whitish thickened membrane (). On incising the fibrous sac, normal looking small bowel loops were freed. Some adhesions between the serosal layer and fibrous sac were also freed. The patient had an uneventful post-operative period and was discharged from the hospital on the seventh post-operative day. She is regularly attending our follow-up clinic and is symptom free. The histopathological study of the membrane revealed non-specific, chronic inflammatory changes. No recurrent disease was present.
3 Discussion
SEP is a rare condition of unknown cause in which intestinal obstruction results from the encasement of variable lengths of bowel by a dense fibrocollagenous membrane that gives the appearance of a cocoon. It can be primary/idiopathic (abdominal cocoon) or secondary. The condition is not often suspected pre-operatively and the diagnosis is usually made at laparotomy. The cause and pathogenesis of the condition have not been elucidated. A history of previous abdominal surgery or peritonitis, chronic ambulatory peritoneal dialysis, and the prolonged use of Practolol have been implicated as causative factors. The pre-operative diagnosis is difficult because of its non-specific imaging findings and reports are few in the literature on its radiologic imaging findings. Various abdominal disorders (such as tuberculosis, sarcoidosis, familial Mediterranean fever, gastrointestinal malignancy, protein S deficiency, liver transplantation, fibrogenic foreign material, and luteinized ovarian thecomas) are the other rare causative factors. Abdominal distension, pain and vomiting, and presence of a soft non-tender mass at abdominal palpation, are the clinical features that may help in the pre-operative diagnosis of SEP.
In the appropriate clinical setting, recognition of the entire dilated small bowel at the center of the abdomen and encased within a thick fibrocollageneous membrane, as though it were in a ‘cocoon,’ on a CT image is diagnostic of SEP. Yamada et al. reported a case of SEP associated with liver cirrhosis and complicated by diffuse, large B cell lymphoma Citation1. There are reports of perforation of cocoon, particularly in immune-compromised patients which carries a high risk of mortality. Bani-hani et al. have reported perforation complicating tuberculous cocoon in immune competent patients Citation2. Multidetector row CT is invaluable for pre-operative diagnosis of this condition and shows typical features of congregated, small bowel loops confined to a single area and encased in a thick membrane Citation3. Multiplanar reformations may provide more diagnostic clues Citation4. It has been reported in the literature to complicate liver transplantation Citation5Citation6. Surgery is mandatory in all the cases and involves excision of the thick membrane and lysis of adhesions Citation7. Few authors have also reported laparoscopic management for this condition Citation8.
We conclude that SEP is a rare complication of abdominal surgery or peritoneal dialysis and should always be considered in differential diagnosis of such patients presenting with intestinal obstruction. Multidetector row CT is the best modality for pre-operative diagnosis and planning elective surgery.
4 Conflict of interest and funding
The authors have not received any funding or benefits from industry to conduct this study.
References
- Yamada S, Tanimoto A, Matsuki Y, Hisada Y, Sasaguri Y. Sclerosing encapsulating peritonitis (abdominal cocoon) associated with liver cirrhosis and diffuse large B-cell lymphoma: autopsy case. Pathol Int. 2009; 59: 681–6.
- Bani-Hani MG, Al-Nowfal A, Gould S. High jejunal perforation complicating tuberculosis abdominal cocoon: a rare presentation in immune-competent male patient. J Gastrointest Surg. 2009; 13: 1373–5.
- Mohanty D, Jain BK, Agrawal J, Gupta A, Agrawal V. Abdominal cocoon: clinical presentation, diagnosis, and management. J Gastrointest Surg. 2009; 13: 1160–2.
- Wang Q, Wang D. Abdominal cocoon: multi-detector row CT with multiplanar reformation and review of literatures. Abdom Imaging. 2010; 35: 92–4.
- Lin CH, Yu JC, Chen TW, Chan DC, Chen CJ, Hsieh CB. Sclerosing encapsulating peritonitis in a liver transplant patient: a case report. World J Gastroenterol. 2005; 11: 5412–3.
- Maguire D, Srinivasan P, O'Grady J, Rela M, Heaton ND. Sclerosing encapsulating peritonitis after orthotopic liver transplantation. Am J Surg. 2001; 182: 151–4.
- Wei B, Wei HB, Guo WP, Zheng ZH, Huang Y, Hu BG, et al.. Diagnosis and treatment of abdominal cocoon: a report of 24 cases. Am J Surg. 2009; 198: 348–53.
- Makam R, Chamany T, Ramesh S, Potluri VK, Varadaraju PJ, Kasabe P. Laparoscopic management of abdominal cocoon. J Minim Access Surg. 2008; 4: 15–17.