Case Report
A 40-year-old male patient was admitted with the symptoms of progressive dyspnea, orthopnea, and abdominal distension of 2 months duration. On examination, vitals were as follows: BP 100/80 mmHg, pulse rate 120/min, and respiratory rate 36/min. He had small bilaterally supraclavicular nodes, a large right axillary lymph node, and the jugular venous pressure was elevated. On auscultation, breath sounds were decreased over both lung bases and heart sounds were only faintly audible. The clinical signs suggestive of free fluid were present in the abdomen.
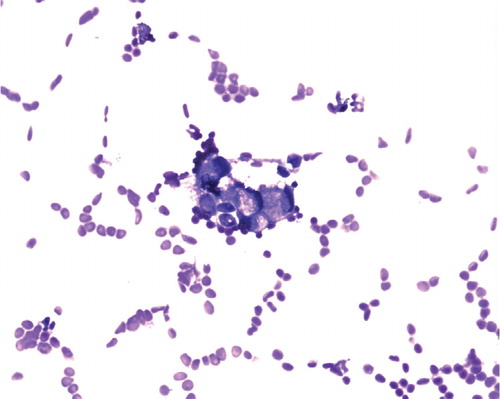
Laboratory findings revealed elevated serum creatinine (2.0 mg/dl) with normal hematocrit, liver function test (LFT), and electrolyte. Chest X-ray posteroanterior (PA) view showed bilateral pleural effusion and pericardial effusion. Thoracocentesis yielded a milky fluid with the following biochemical composition: total protein 3.6 g/dl, albumin 2.0 g/dl, glucose 118 mg/dl, and LDH 121 U/l. Cell count of the fluid showed 1,300/mm3 of WBCs; of which 96% were lymphocytes and 4% polymorphs, triglycerides 411 mg/dl, cholesterol 70 mg/dl, and chylomicron 260 mg/dl. Pleural fluid cytology showed atypical cells and closed pleural biopsy revealed non-specific chronic inflammation. Cultures of the fluid including mycobacterial culture, of peritoneal and pleural fluid were non-contributory. Two dimensional (2D) ECHO-cardiograph showed moderate pericardial effusion with collapse of right atrium and right ventricle, suggesting cardiac tamponade. Pericardiocentesis was done immediately which revealed hemorrhagic fluid. Pericardial fluid cytology showed atypical cells suggestive of malignancy, although biochemical analysis confirmed that it was not chylous. The fine needle aspiration cytology (FNAC) of the axillary lymph node revealed signet ring cell adenocarcinoma (). Computed tomography (CT) of the thorax was done after thoracocentesis to find out the possible etiology. It showed bilateral pleural effusion, pericardial effusion, paratracheal, and mediastinal lymph nodes up to 8 mm with a calcified granuloma in the left upper lobe (). FNAC of these lymph nodes were not done in view of smaller size of lymphnode. Abdominal ultrasonography and CT of the abdomen showed left sided hydorneprhosis with moderate ascites. No lymphadenopathy or tumors were detected during abdominal CT. Other investigations to locate primary such as fiberoptic bronchoscopy, upper GI endoscopy, and colonoscopy could not be done due to unfavorable physical condition. The final diagnosis was metastatic signet ring cell adenocarcinoma of unknown primary with chylothorax, chylous ascites, and probably malignant pericardial effusion.
During hospital stay, patient required repeated thoracocentesis and pericardiocentesis. He was started on low cholesterol diet with medium chain triglyceride supplements. To minimize nutritional depletion, intercostal tube was not inserted. In view of poor prognosis the patient and his family opted for treatment at their hometown. He was thus sent home with recommendations to commence treatment with a local palliative care unit.
Discussion
Chyle is described as being white, milky, or opalescent in appearance. This characteristic color is seen in less than one half of patients with chylous effusion Citation1Citation2. Pleural-ascitic fluid triglyceride level of more than 110 mg/dl generally confirm the diagnosis of chylothorax or chylous ascites Citation1Citation7. Chylous pleural effusion (Chylothorax) is usually secondary to disruption of the thoracic duct or derangement of lymphatic flow within the thorax Citation1Citation3Citation4Citation5. Chylous ascites is associated most frequently with malignant conditions such as lymphomas and disseminated carcinomas from primaries in the pancreas, breast, colon, prostate, ovary, testes, and kidney Citation8. In some patients, chylothorax occurs in the setting of chylous ascites, which in turn is related to a primary abdominal process such as nephrotic syndrome, hypothyroidism, cirrhosis of the liver, abdominal operations, and pancreatitis Citation1. In our patient, CT of thorax and abdomen were not contributory.
The treatment of the chylothorax and chylous ascites usually involves the treatment of the underlying cause. Malignant chylous serositis requires specific therapy directed at the primary cause with chemotherapy, radiation, and surgery with supportive therapy Citation8. Treatment of chylous pleural effusions with chest tube thoracotomy and pleurodesis has had limited success regardless of the sclerosing agent used. It also usually requires prolonged drainage, which could lead to nutritional and immune compromises Citation9.
Signet ring cell adenocarcinoma is most common in the stomach followed by the colon Citation11. There is only one report where primary have been found in the lung Citation10. In our patient the primary was unknown. However, in view of poor general condition of the patient invasive procedures like endoscopy or bronchoscopy were not possible.
Chylothorax with chylous ascites associated with pericardial effusion is a rare finding. If the cause is malignancy, it is difficult to treat. There are only few published case reports of chylothorax and chylous ascites occurring together. Among them, one case of chylothorax with chylous ascites due to metastatic carcinoma of lung, one due to constrictive pericarditis, and the rest due to metastatic carcinoma of stomach Citation6Citation9Citation12. We would like to conclude that chylothorax with chylous ascites in background of malignant pericardial effusion is a rare scenario.
Conflict of interest and funding
This work was conducted at Christian Medical College, Vellore, Tamilnadu, India. The authors have not received any funding or benefits from industry to conduct this study.
References
- Doerr CH, Allen MS, Nicholas III FC, Ryu J. Etiology of chylothorax in 203 patients. Mayo Clin Proc. 2005; 80: 867–70.
- Staats BA, Ellefson RD, Budahn LL, Dines DE, Prakash UBS, Offord K. The lipoprotein profile of chylous and nonchylous pleural effusions. Mayo Clin Proc. 1980; 55: 700–4.
- Sassoon CS, Light RW. Chylothorax and pseudochylothorax. Clin Chest Med. 1985; 6: 163–71.
- Sahn SA. The differential diagnosis of pleural effusions (Medical Progress). West J Med. 1982; 137: 99–108.
- Roy PH, Carr DT, Payne WS. The problem of chylothorax. Mayo Clin Proc. 1967; 42: 457–67.
- Guneri S, NazlI C, Kinay O, Kirimli O, Mermut C, Hazan H. Chylous ascites due to constrictive pericarditis. Int J Card Imaging. 2000; 16: 49–54.
- Riza Altiparmak M, Avsar S, Yanik S. Chylous ascites and chylothorax. Neth J Med. 2004; 62: 59–61.
- Raghuraman UV. Chylous ascites, eMedicine specialties, e Medicine, Gastroenterology, liver. ; 2008. Available from: http://www.tripdatabase.com/doc/830069-Chylous-Ascites (Overview) [cited 25 March 2010]..
- Wohlrab JL, Read CA. Chylothorax associated with Noonan syndrome: management with medical thoracoscopic talc pleurodesis. J Bronchol. 2002; 9: 122–4.
- Tanaka F, Fukama S, Sawada K, Seki Y, Ishida I, Kuwahara T. Bilateral chylothoraxand chyloperitoneum associated with signet-ring cell carcinoma of the lung. Nippon Kyobu Geka Gakkai Zasshi. 1981; 29: 1064–9.
- Gold Stein NS, Long A, Kuan SF, Hart J. Colon signet ring cell adenocarcinoma: immunohistochemical characterization and comparison with gastric and typical colon adenocarcinomas. Appl Immunohistochem Mol Morphol. 2000; 8: 183–8.
- Bautz JB, Delaney MD, Mostaghim R, Lodato RF. Chylothorax as presenting manifestation of adenocarcinoma with probable gastric primary. Chest. 1999; 99: 1044–5.