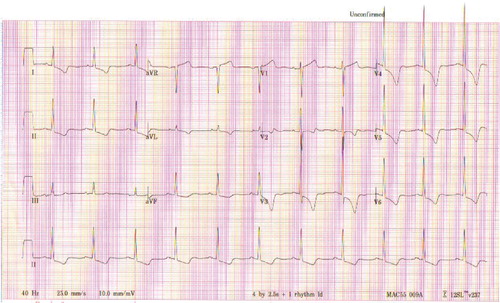
The following 12-lead electrocardiogram (ECG) was obtained from a 69-year-old female who presented to the hospital following an episode of syncope (see ).
Q1: What is the ECG diagnosis?
Q2: Based on the brief clinical history provided with this ECG, what are the likely causes for her syncope?
Q3: Based on the clinical information below, what is the clinical diagnosis?
The lady has a 12–18-month history of a progressive exertional dyspnea with chest tightness. Her heart rate was 68 per minute and blood pressure was 110/85 mmHg with no significant postural changes. The jugular venous pressure was normal at 2 cm above sternal angle and her carotid pulses were of low volume and delayed upstroke. The first heart sound (S1) was normal, however, S2 was soft and single and there was S4 gallop. A grade 3/6 harsh, late-peaking ejection systolic murmur was heard along the left sternal border with some radiation to carotid arteries.
Answers and explanations
A1: The ECG diagnosis: left ventricular hypertrophy (LVH) with strain
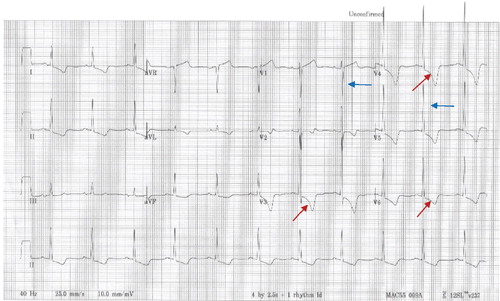
The ECG shows sinus rhythm at 66 beats per minute, normal electrical axis, and left ventricular hypertrophy (LVH) by both voltage (S wave in V1 or V2+R wave in V5 or V6>35 mm) and ST-T segment abnormalities. The diagnosis of LVH can be made with reasonable certainty from the ECG if there is high QRS voltage and associated ST-T changes. Pressure overload causes sustained delayed repolarization of the left ventricle, producing a negative ST segment and T wave in leads with leftward orientation (i.e. V5 and V6); this condition is called left ventricular strain. The mechanism of strain is not clearly understood, but it is related to the increased pressure (pressure-overload) in the left ventricular cavity (see ).
A2: The possible causes for her syncope
Hypertrophic obstructive cardiomyopathy (HOCM), cardiac arrhythmia, and aortic valve stenosis.
The ECG showed that this patient has an underlying left ventricular pressure or volume overload state. The most common pressure overload states that may result in this ECG picture are: systemic hypertension, aortic valve stenosis, and HOCM. Left ventricular volume-overload conditions, such as aortic regurgitation and mitral valve regurgitation may also cause LVH. Cardiac arrhythmias, both ventricular and supraventricular, may lead to syncope however; syncope due to transient ischemic attack is extremely rare. In order to determine the cause of this patient's syncope, more clinical information is required.
A3: Severe (critical) aortic valve stenosis
Now, we can say with certainty that this patient's syncope was due to severe (critical) aortic valve stenosis. Further evaluation with a transthoracic echocardiogram revealed a critical aortic valve stenosis (an aortic valve area of 0.45 cm2). The diagnosis was predicted based on the following clinical information: Symptoms: syncope, exertional dyspnea, and exertional angina. Remember!! ‘Aortic stenosis is a “SAD story”: S=syncope; A=angina; D=dyspnea.’
Signs: The carotid pulse has low volume and delayed upstroke (i.e. ‘pulsus parvus et tadus “in Latin”’); a harsh, late-peaking ejection systolic murmur; soft and single second heart sound (S2).
Conclusion
The diagnosis of LVH can be made with reasonable certainty from the ECG if you find high QRS voltage and associated ST-T changes. Because high voltage in chest and limb leads is often seen in normal children and young adults, especially athletes, the diagnosis of LVH should not be made based on these findings alone.
The recognition of LVH is clinically important for two reasons:
Diagnostically, LVH is a clue to the presence of a potentially life-threatening pressure or volume-overload state (hypertension, aortic stenosis, hypertrophic cardiomyopathy, aortic regurgitation, and mitral regurgitation).
Prognostically, patients with LVH from any cause are at increased risk for major cardiovascular complications, including congestive heart failure and serious atrial, or ventricular arrhythmias.