Abstract
Sclerosing lipogranuloma (SLG) of the male external genitalia is a rare benign condition presenting as subcutaneous masses. The underlying pathological process is a granulomatous reaction of fatty tissue in this area. The cause of this is unclear but hypothesis stems around the pathogenesis of exogenous lipid degeneration from injection of foreign bodies such as paraffin for penile augmentation. However, endogenous lipid degeneration from other various causes such as infection, trauma, and allergic mechanisms has also been reported. We present the case of a 40-year-old man with primary SLG of the external genitalia. Literature review on the treatment strategies are addressed and discussed.
Introduction
Sclerosing lipogranuloma (SLG) is a granulomatous inflammation with marked sclerosing response to the fatty tissue Citation1. It may occur in any part of the body but is frequently reported in the male external genitalia Citation2. This is due to foreign material which is oil based, injected into the penis and scortum to achieve penile augmentation and enhance sexual performance. As these exogenous materials result in lipid degeneration, a primary process of spontaneous endogenous lipid degeneration is also recognised as another cause of SLG. This is due to infective process, trauma, extremes of temperature or allergic mechanisms. Endogenous causes are mainly reported in the East-Asian countries where patients deny injecting foreign substance into the external genitalia. Management strategy of this disease varies and is not influenced by the causative factor. Here we present a young man with primary SLG of the external genitalia. A literature review on its causes and treatment options available is presented.
Case report
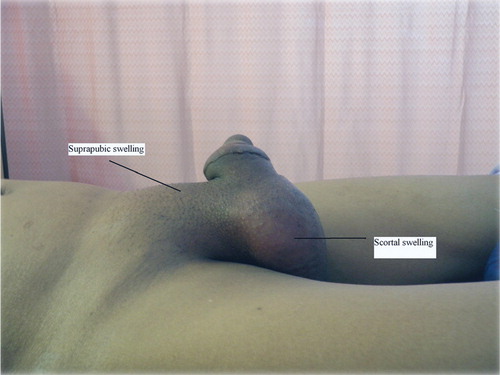
A 40-year-old man presented with bilateral scrotal, penile, and suprapubic swelling, which was intermittently tender and had progressively enlarged over 4-month period. He denied injecting foreign material into his external genitalia. There was no trauma to the groin and no symptoms of urinary tract infection. Past history revealed an episode of penile discharge 2 years ago which grew Klebsiella species treated with antibiotics. On examination, the penis and scrotum were swollen and tense. The swelling extended to the suprapubic region. There was bilateral inguinal lymphadenopathy. The testes were not palpable due to the scrotal oedema. There were multiple non-tender, irregular masses on the penile shaft dorsally without pus discharge per meatus ().
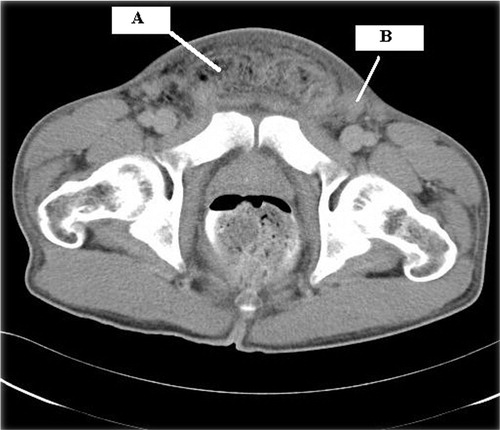
His white cell counts were 11.8×109 and erythrocyte sedimentation rate (ESR) was 79 mm/h. Urine full examination and microscopic examination (FEME) was normal. Ultrasonography showed thickened scrotum due to oedema, minimal hydrocele with normal testes. Blood screen for sexually transmitted diseases were negative. Serology test for tuberculosis, fungal, cytomegalovirus, and filariasis from blood and tissue cytology were negative. Computer tomography of abdomen and pelvis showed bilateral scrotal enlargement with presence of a fat component within, extending superiorly to anterior abdominal wall (). Initial fine needle aspiration of enlarged lymph node yield a mixed population of lymphoid cells, predominantly of small lymphocytes, suggestive of a reactive process. As this diagnosis was inadequate, an excision of lymph node was performed.
Fig. 2. Computer tomography appearance of suprapubic lipogranuloma. A – suprapubic fatty accumulation. B – left inguinal lymph node involvement.
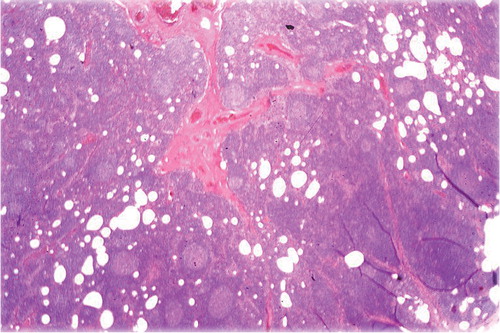
Lymph node excision biopsy revealed lymphoid follicles of various sizes with prominent germinal centre and tangible body macrophages. There was lipo-granulomatous reaction in the sinuses (). He was treated with broad spectrum antibiotics for 8 weeks. He had initially been on intravenous Ciprofloxacin 400 mg bd for 10 days, followed by oral Augmentin (Amoxicillin/Clavulinic Acid) 625 mg bd for 14 days. Later a combination of Doxycycline 100 mg daily and metronidazole 500 mg tds was given for 2 weeks in view of possible sexually transmitted microorganism involvement. Intravenous Ceftriaxone 1 gm daily was added for a total of 10 days. Following a bout of fever, intravenous Meropenem 1 gm tds was commenced for 1 week. Partial resolution of the genitalia and suprapubic swelling with complete resolution of pain was achieved. No surgical excision was required. The bilateral inguinal lymphadenopathy had shown partial resolution prior to discharge but later completely resolved on follow up one month later.
Discussion
Primary SLG of the male genitalia is rare and is believed to result from breakdown of endogenous lipids. This occurs following an allergic pathway induced by heat, extreme cold, infection, and trauma such as bicycle saddle injury and vigorous sexual intercourse. Some authors have reported presence of esonophilia in peripheral blood which supports the hypothesis of an allergic mechanism in these patients Citation3.
Patients experience painful erections and penile deformity and usually have tender subcutaneous nodules from penile base, along its shaft and in the scortum. Primary lesions have also been reported in the testis, presenting as a firm mass and requiring a radical orchidectomy to rule out possibility of malignancy Citation4.
Our patient most likely has a primary cause of this disease as he denied injecting foreign material into the external genitalia. He additionally had a diffuse and tender suprapubic mass which extended to the margins of the inguinal ligament bilaterally that has never been reported thus far. This had made us look for filiriasis as a possible cause as Wuchereria bancrofti is known to cause scrotal and suprapubic swellings and is common in Asian countries Citation5. Recurrent infection with Klebsiella species was ruled out as a possible etiology of primary SLG and bilateral lympphadenopathy based on the normal urine analysis results. This patient had a muscular build and it could be the strenuous muscle exercises resulting in primary lipid degeneration and lipogranuloma formation around his suprapubic and external genitalia region.
However as in most cases, it is almost impossible to pin point the exact cause of primary SLG. Some authors consider most primary cases are actually secondary because patients are not forthcoming about the use of foreign material injections Citation6. Does this matter? It probably does not as treatment strategies vary and not influenced by its underlying cause. Treatment is generally divided in to conservative and surgical approach. Surgical treatment includes partial or total excision of nodules with or without reconstructive skin flaps depending on extent of deformity. Partial excision may result in spontaneous regression or sometimes, quite the opposite, early recurrence which mimics a malignant disease process. This can cause unwanted anxiety among patients and treating surgeons. Péter et al. Citation7 advocated complete excision combined with penoplasty for best outcomes.
Conservative management varies from close observation, symptomatic treatment, antibiotic treatment to oral corticosteroids. Recent reports have shown good response to oral steroids over a 6-week period. Steroids also had resolved the associated eosinophilia seen in primary SLG Citation8. As there are very little data on the use of other drugs in its treatment, systemic steroids thus should be the first-line treatment for primary SLG while surgery is reserved for patients with refractory disease or with recurrences.
Our patient benefited from a prolonged treatment of broad spectrum antibiotics as his main concern of pain over the suprapubic mass and scortum was alleviated. However, he remains under close follow up to detect recurrences for which the oral steroids may be used.
Conflict of interest and funding
The authors have not received any funding or benefits from industry to conduct this study.
References
- Inci GK, Hatice B, Hakan O. Sclerosing lipogranuloma of male genitalia. Eur J Plast Surg. 2004; 27: 249–52.
- Lim HK, Byun JH, Yoon SE, Kim AY, Ha HK. Primary sclerosing lipogranuloma of the rectum: CT findings. Br J Rad. 2006; 79: e190–2.
- Matsuda T, Shichiri Y, Hida S, Okada Y, Takeuchi H, Nakashima Y, et al.. Eosinophilic sclerosing lipogranuloma of the male genitalia not caused by exogenous lipids. J Urol. 1988; 140: 1021–4.
- Vincent SR, Martin BR, Christopher AH, Dhanlaxmi D, Dan XC. Sclerosing lipogranuloma of the testis. Urology. 2002; 60: 515xviii–xix.
- Stefan D, Elke W, Maximilian B, Wolf FW, Wolfgang O. Giant scrotal elephantiasis of inflammatory etiology: a case report. J Med Case Reports. 2007; 1: 23.
- Yuji O, Junichi M, Yoshihiro K, Masataka Y, Takao S, Mutsuo F. Three cases of sclerosing lipogranuloma: an immunohistochemical study. Med Mol Morphol. 2007; 40: 108–11.
- Péter N, Zsolt K, András K, Gergely B, Katalin B, Imre R. Treatment and outcome of vaseline-induced sclerosing lipogranuloma of the penis. Urology. 2008; 71: 1132–7.
- Nathan L, David A, Damien MB. Sclerosing lipogranuloma of the genitalia treated with corticosteroids. Int Urol Neph. 2006; 38: 97–9.