Abstract
Over the past 2 years there has been a radical change in standard clinical practice with respect to vitamin D. As a result of a growing body of knowledgeable physicians are assessing the vitamin D nutritional status of their patients and prescribing aggressive repletion regimens of a vitamin D supplement. The present paper summarizes some basic information about this essential nutrient and reviews some of the more recent data implicating vitamin D deficiency in disease etiology with an emphasis on cardiovascular disease and cancer. Finally a rational approach to the dosing of vitamin D in different patient populations is provided.
Introduction
Over the past 5 years there has been a marked increase in the number of high-dose vitamin D prescriptions in the United States. A spike in prescriptions for a particular drug is normally observed following the publication of a seminal clinical study whose compelling results command attention and dictate changes in standard clinical practice. This review explores the data behind this prescribing trend.
Vitamin D has a long and interesting history that is closely linked to that of the childhood bone disease rickets. Although the existence of vitamin D had been suspected since the mid-17th century, it was not actually discovered until 1920 and its chemical structure was not elucidated until 1932 Citation1Citation2Citation3.
In the decades that followed its discovery, an overwhelming body of clinical and laboratory evidence established its critical role in the maintenance of calcium balance and skeletal health. Thus, vitamin D is associated first and foremost with these functions. However, a quick survey of the current literature reveals that vitamin D is at the center of an endocrine system that regulates cellular proliferation and differentiation in addition to a wide range of other cellular processes, extending the role of vitamin D beyond the skeleton to include the immune, cardiovascular, and neuroendocrine systems. Such a survey would also indicate that vitamin D deficiency as well as genetic variation in its receptors may play a significant role in the etiology of a variety of chronic disorders including mycobacterial infections, diabetes, cardiovascular diseases, cancer (e.g. colorectal), and autoimmune diseases such as systemic lupus erythematosus (SLE), multiple sclerosis, rheumatic arthritis, and psoriasis. Vitamin D is now a highly active field of research. Over 2,300 papers on the subject were published in the first 9 months of 2010.
Following a summary of a few essential facts about vitamin D, the review will focus on its role in disease etiology, and the experts’ opinions concerning the optimal vitamin D levels and daily doses for different patient populations.
Physiology of vitamin D
Vitamin D belongs to the quartet of fat soluble vitamins (A, D, E, and K). This accounts for its distribution primarily in adipose tissue and its very slow turnover rate. Structurally, it is a secosteroid with a ring structure similar to cholesterol except for a broken C–C bond in the B ring (a and b).
Fig. 1. (a) Basic chemical structure of a steroid. When UVB rays strike 7-hydrocholesterol in the epidermis the C9–C10 bond in the B ring breaks forming an intermediate compound called pre-D3 that isomerizes to D3. (b) The structures of calciferol (D2) and cholecalciferol (D3). The structural differences between the two compounds are limited to the side chain; D2 has one additional methyl group and a double bond.
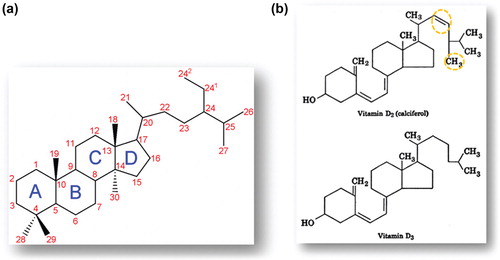
There are two main forms of vitamin D: the first is vitamin D2, which is also referred to as ergocalciferol or calciferol. It is produced by the irradiation of yeast or plant ergosterol. The second and more important is vitamin D3 (cholecalciferol), which is derived from the photoconversion of 7-hydrocholesterol in the skin upon exposure to sunlight or artificial ultraviolet radiation (wave length range 285–315 nm, known as UVB). Significant amounts of vitamin D3 can also be obtained from fish liver oil and oily fish in general and very small amounts from other animal products. Supplemented milk sold in the United States contains approximately 100 international units (IUs) per cup. Vitamin D3 is produced commercially starting with lanolin (wool fat) as the raw material. Of course both D2 and D3 are available in pill form. In the United States, vitamin D3 is widely available as over-the-counter (OTC) products in tablet or capsule form (200–5,000 IUs each) or oral liquid form. Vitamin D2 is available by prescription in the form of capsules containing 50,000 IUs each. Vitamin D2 is biologically weaker than D3, possessing only about 30% of vitamin D3 activity.
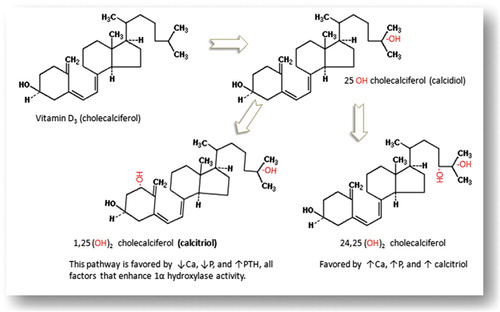
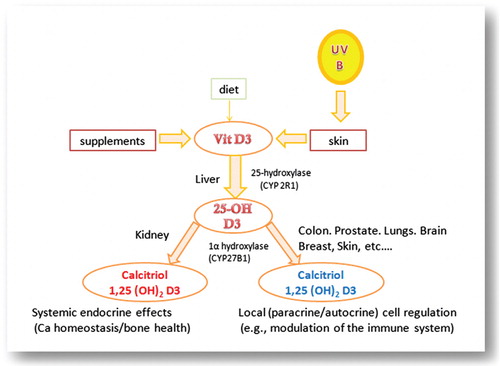
In the body, the two forms (D2 and D3) follow similar metabolic pathways. However, our focus in this review will be primarily on D3 since it constitutes the predominant input and the naturally occurring form in humans. In the liver, cholecalciferol (D3) is hydroxylated in position 25 to form 25-hydroxy-cholecalciferol [25(OH)D3] (also called calcidiol, ). This reaction is catalyzed by 25-hyroxylases that are cytochrome P450 enzymes located in the endoplasmic reticulum such as the microsomal CYP2R1 and the mitochondria CYP27A1. Calcidiol [25(OH)D3] represents the storage form and the major circulating metabolite of vitamin D3. Its level in the plasma is used clinically to assess a patient's vitamin D nutritional status. In the circulation, vitamin D and its various metabolites travel aboard a specific carrier protein known as a vitamin D-binding protein (DBP). At physiological concentrations, vitamin D2, vitamin D3, and calcidiol have virtually no intrinsic biological activity. In the kidney, a second hydroxyl group is added to the calcidiol molecule in position 1 to form 1α,25-dihydroxycholecalciferol [1,25(OH)2D3], often referred to as calcitriol. In the kidney, this reaction is catalyzed by 1α hydroxylase, a cytochrome P450 enzyme (CYP27B1). Calcitriol is the active, hormonal form of vitamin D3 whose serum level normally ranges between 15 and 75 pg/mL. Calcitriol is available by prescription in oral and injectable forms for patients with advanced kidney disease. Some calcidiol is hydroxylated in position 24 (instead of position 1) to form 24,25-dihydroxy-cholecalciferol [24,25(OH)2D3], which is also biologically active (). Other products include 25,26(OH)2D3 and 25(OH)D3 23-26 lactone.
Mutation of the gene coding for the 1α hydroxylase (CYP27B1) results in the rare disease of vitamin D pseudodeficiency, which is characterized by an undetectable level of circulating calcitriol, hypocalcemia, hyperparathyroidism, and rickets Citation4. Production of calcitriol and its circulating level depend on several factors, the most important of which is the activity of 1α-hydroxylase (CYP27B1) in the proximal tubule cells of the kidney. The activity of this enzyme is enhanced by low calcitriol levels, high parathyroid hormone (PTH), hypocalcemia, and hyperphosphatemia. However, in addition to the 1α-hydroxylase activity, a key determinant of calcitriol production rate is the circulating concentration of its immediate precursor, calcidiol [25(OH)D3], which depends on vitamin D3 inputs (skin exposure to UVB radiation and/or oral intake of D3). Calcitriol production is inhibited by the fibroblast growth factor 23 (FGF23) in association with α-Klotho as a cofactor; α-Klotho is a protein that appears to be a key player in a complex regulatory system of calcium and phosphate homeostasis Citation5.
Both calcidiol and calcitriol are ultimately inactivated through an oxidative pathway involving CYP24A1, which has been shown in experimental animals to play a critical role in the prevention of vitamin D toxicity Citation6. The end product of calcitriol oxidation (via CYP24A1) is calcitroic acid that is eliminated in the urine.
Although cholecalciferol is referred to as a vitamin, its active metabolite calcitriol fits the definition of a hormone; it is produced by a discrete organ (a gland, the kidney in this case), travels through the circulation to reach specific target tissues, and interacts with specific receptors in the target cells to trigger predictable biological responses. Most of the known actions of calcitriol are mediated via a nuclear transcription factor known as the vitamin D receptor (VDR). In the cell nucleus calcitriol binds to VDR and causes it to bind to the retinoic acid x-receptor (RXR). The calcitriol–VDR–RXR complex binds to certain DNA segments known as the vitamin D response elements (VDREs) to initiate the regulation of specific genes. Calcitriol is involved in the regulation of more than 200 genes, including those controlling insulin synthesis, renal renin production, the proliferation and growth of cardiac and vascular muscle cells, the release of cytokines by the T cells, and the production in macrophages of the antimicrobial peptide cathelicidin.
There are significant individual and ethnic variations in the gene coding for VDR. These genetic variations (polymorphisms) that usually involve a single nucleotide are thought to be largely responsible for the variation in individual response to vitamin D and may be a significant determinant of the risk for different diseases Citation7Citation8Citation9.
In addition to the nuclear VDR, another kind of vitamin D receptor exists that is associated with the plasma membrane rather than the nucleus. This membrane-associated receptor is thought to mediate rapid, non-genomic cellular responses to calcitriol such as insulin secretion, the opening of voltage-gated ion channels in osteoclasts, and the rapid translocation of calcium ions across the wall of the small intestine Citation10Citation11Citation12.
It is well established since the early 1930s that vitamin D deficiency is the primary cause of the bone disease known as rickets in children and osteomalacia in adults. In the 1940s it became mandatory in the United States to fortify milk with vitamin D3, which resulted in a dramatic decline in the incidence of rickets. Consequently, most of the early research focused on the role of vitamin D in regulating calcium balance, skeletal development, and maintenance of bone health. The small intestine, kidneys, parathyroids, and bone have been identified as the effector organs involved in the calcitriol endocrine regulatory system. It is in these target tissues that the presence of the nuclear vitamin D receptor (VDR) was first established. However, over the past 25 years VDR has also been found in over 30 other cell types including the brain, skeletal muscle, heart, smooth muscle, skin, beta cells of the pancreas, and cells of the immune system (macrophages, dendritic cells, and B & T lymphocytes). Researchers have also revealed the extrarenal presence of 1α-hydroxylase (CYP27B1) in many tissues (colon, prostate, dendritic cells, skin, etc.) where locally produced calcitriol appears to serve localized (paracrine) functions () and where its local production does not contribute to the circulating pool of calcitriol except in the case of granulomatous diseases such as sarcoidosis probably due to the absence in macrophages of CYP24A1, which is responsible for the oxidative deactivation of calcitriol Citation4.
Vitamin D and the immune system
Despite the recent expansion in vitamin D research, an immense gap remains in our knowledge of its multiple functions in the variety of cell types where the presence of vitamin D receptors and paracrine production of calcitriol have been established. However, it is now generally accepted that a strong connection between vitamin D and the immune system exists as suggested by several key findings: (a) the presence of VDR in activated human immune cells, (b) the ability of these cells to produce calcitriol, and (c) the ability of calcitriol to inhibit the proliferation of T cells. In addition, it has become increasingly evident in recent years that calcitriol plays a significant role in modulating the function of the immune system. Furthermore, many epidemiological studies strongly suggest that vitamin D deficiency and certain VDR polymorphisms may be linked to immune system related diseases such as multiple sclerosis, SLE, DM type I, alopecia (areata or universalis), and psoriasis Citation13Citation14Citation15Citation16Citation17Citation18.
Upon penetrating the body, the microbe sheds its pathogen-associated molecular patterns (PAMPs), which are quickly recognized by the toll-like receptors (TLRs) on the surface of the immune cells. This recognition triggers a complex cascade of events inside the host immune cell, which leads to the initiation of the innate immune system response. This includes the release of cytokines, enhanced expression of antimicrobial peptides (natural antibiotics) such as cathelicidin, and a surge in the production of reactive oxygen species. Several studies have now demonstrated that injury or the addition of microbial lipopeptides enhances the expression of CYP27B1 (1α-25OH-D3 hydroxylase) and the paracrine production of calcitriol. Also, the expression of cathelicidin in both myeloid and epithelial cells is induced by calcitriol. These observations suggest that this hormone plays a significant role in the host immune response Citation19Citation20Citation21Citation22Citation23Citation24. Further, in the absence of adequate levels of 25(OH)D3 (calcidiol), the paracrine production of calcitriol and the expression of cathelicidin are both markedly reduced.
A recent study by Krutzik et al. has clearly demonstrated the absolute need for IL-15, which is produced by the innate immune cells upon the activation of TLR2/1; IL-15 is essential for the induction of CYP27B1 and the conversion of calcidiol to calcitriol, leading to VDR activation and the expression of cathelicidin Citation25. In addition, the antimicrobial activity of cathelicidin against intracellular pathogens such as mycobacterium tuberculosis has been demonstrated. This may explain the salubrious effect of sun exposure on tuberculosis patients.
The overall effect of calcitriol on the adaptive immune system is suppressive; it suppresses antibody production by inhibiting the differentiation of B cells into the immunoglobulin producing plasma cells. With respect to the T cells, the actions of calcitriol are more complex. By affecting the secretion of various cytokines, calcitriol promotes the functions of Th2 and Treg (previously known as suppressor T cells) and inhibits the development and function of Th1 and Th17 Citation25.
These effects may form the basis for the connection between vitamin D deficiency and autoimmune diseases. The inhibition of Th1 by calcitriol leads to decreased production of both INF-γ and IL-2; this in turn results in the suppression of macrophage activation and antigen presentation and prevents further proliferation and recruitment of T cells. Vitamin D deficiency is now believed to be linked to Th1-mediated autoimmune diseases such as multiple sclerosis Citation26.
Epidemiology of vitamin D deficiency
Vitamin D deficiency is now recognized as a pandemic particularly in the northern hemisphere where winters are severe and sun exposure is minimal. Vitamin D is lipophilic and distributes preferentially into the adipose tissue with a half-life of approximately 2 months. As mentioned above, the biomarker of vitamin D status is the level of circulating calcidiol [25(OH)D], which due to its lipophilic nature distributes into the adipose tissue and represents the storage form of vitamin D with a half-life of 15 days. Vitamin D deficiency is defined as a calcidiol level <20 ng/mL, insufficiency as a level of 21–29 ng/mL, and sufficiency as a level >30 ng/mL (1 ng/mL=2.5 nmol/L). In current medical practice, these reference ranges are gradually shifting upward as vitamin D deficiency is increasingly being implicated in the etiology of an expanding list of diseases. Obvious vitamin D toxicity manifested as hypercalcemia and ectopic calcification does not occur until the calcidiol level is well above 150 ng/mL. However, the long-term safety of sustained high levels (>50 ng/mL) is yet to be determined since the trend of prescribing vitamin D mega-doses has become widespread only recently. Therefore any benefit of vitamin D intake has to be balanced against the risk of known short-term and potential long-term toxicities Citation27, Citation28.
The Third National Health and Nutrition Examination Survey (NHANES III) has revealed that a large segment of the American population have low vitamin D levels, a fact that has been confirmed in many other studies. The phenomenon of vitamin D deficiency has also been found in many other parts of the world including North Africa and the Middle East where social customs dictate minimal skin exposure. The reasons for vitamin deficiency are multiple and include indoor life style, high latitude, dark skin, insufficient skin area exposed to UVB, obesity (expanded volume of distribution), aging (reduced capacity for photosynthesis), severe liver disease, and chronic kidney disease (CKD).
In addition to bone diseases in both children and adults, vitamin D deficiency has been linked to a wide variety of chronic conditions including diabetes mellitus type II, hypertension, colorectal cancer, infectious diseases, and autoimmune diseases such as SLE and diabetes mellitus type I. However, in most of these conditions a causal relationship and the pathophysiological mechanisms involved have not yet been established.
Vitamin D and cardiovascular disease (CVD)
Calcitriol plays a significant role in the regulation of many genes including those involved in the regulation of renal renin production and the proliferation and growth of cardiac and vascular muscle cells. Also, calcitriol has an anti-inflammatory effect manifested in the downregulation of C-reactive protein and other proinflammatory markers. Thus it is not surprising that vitamin D deficiency has a negative impact on cardiovascular health. Several observational studies point to a strong association between vitamin D deficiency and cardiovascular mortality adding a potential novel CVD risk factor. In a retrospective study focusing on racial differences between black and white Americans, Fiscella and colleagues evaluated data from nearly 15,000 participants in the NHANES III (1988–1994) and cause-specific mortality through 2001 using the National Death Index. Black participants with calcidiol levels in the lowest quartile (mean=13.9 ng/L=34.8 nmol/L) had a 40% greater risk of death due to coronary heart disease, heart failure, or stroke compared with those whose levels were in the three higher quartiles (means: 21.6, 28.4, and 41.6 ng/mL). With respect to race, the study found that blacks have a nearly 40% greater risk of CVD related mortality than whites, but this difference was reduced to 14% when the two groups were matched with respect to the calcidiol level Citation29. Several other studies have also shown vitamin D deficiency to be associated with a higher risk for metabolic syndrome, hypertension, and adverse cardiovascular events Citation29Citation30Citation31. Revved up renin–angiotensin–aldosterone system, insulin resistance, and secondary hyperthyroidism are thought to mediate at least some of the cardiovascular effects of vitamin D deficiency. In 2008, Lee and colleagues reviewed this topic in greater detail for the Journal of the American College of Cardiology Citation32.
Vitamin D and cancer
One of the earliest hints of a possible association between vitamin D deficiency and cancer is the observation that both vitamin D deficiency and the incidence of certain cancers vary by latitude. This is thought to be related to the north–south sunshine gradient and is sometimes referred to as the geographic or ecological factor.
In an epidemiological study involving 111 countries, a strong positive association between latitude and the incidence rates of lung cancer was found. At the same time there was an inverse relationship between lung cancer rates and the effective exposure to UVB rays. Having accounted for other factors such as cigarette smoking, the authors concluded that low levels of UVB irradiance are independently associated with higher incidence rates of lung cancer Citation32. Retrospective analysis of more than 60 observational studies in the United States suggests that inadequate vitamin D levels may be associated with a higher incidence of cancer in general Citation33Citation34Citation35Citation36Citation37.
In a follow-up study lasting 18 years and involving nearly 15,000 men who participated in the United States Physicians’ Health Study it was concluded that men whose calcidiol levels were below the median concentration of 25 ng/mL in the winter and 32 ng/mL in the summer had a significantly greater risk of prostate cancer than those whose levels were above the median (odd ratio=2.1 with 95% confidence interval 1.2–3.4). When the low calcidiol level was associated with the less functional VDR FokI ff genotype (as opposed to FokI FF) the risk was greater and the cancer more aggressive Citation34. There have also been numerous other retrospective analysis and nested studies suggesting a potential for cancer prevention by maintaining adequate circulating vitamin D levels. Data from the Women's Health Initiative point to the possibility that chronic vitamin D deficiency [calcidiol levels <23 ng/L (58 nmol/L)] may be associated with increased incidence of malignancy Citation35.
In a prospective study involving 1,179 patients with an average baseline calcidiol level of 28 ng/mL, Lappe et al. compared the effects of daily intake of calcium (about 1,500 mg), calcium plus vitamin D3 (1,100 IUs), or placebo over a period of 4 years. Supplementation resulted in raising the serum calcidiol level above 38 ng/mL. After excluding patients who were diagnosed with tumors within the first year of study, the Ca plus D3 group had a significantly lower incidence of malignancies than the other two groups Citation38.
This wealth of information prompted the International Agency for Research on Cancer (IARC) to charge a number of expert panels with the task of conducting in-depth reviews of available data related to Vitamin D and cancer. The groups conducted various types of studies including meta-analyses, prospective, and nested and published their initial reports in 2008. The Cohort Consortium Vitamin D Pooling Project (VDPP) pooled data from patient populations (cohorts) with a considerable degree of diversity in terms of race and geography and spanning a period of over 30 years. One conclusion of these studies is that adequate vitamin D (calcidiol) levels provide significant reduction in the risk for colorectal cancer. Data from prospective studies demonstrated a statistically significant decrease in the risk of colorectal cancer per 1 ng/mL increase in serum calcidiol level (RR=0.984, 95% CI: 0.976, 0.991). However, for both breast and prostate cancers, meta-analyses of pooled data were inconclusive Citation37. Meta-analysis of the prospective breast cancer studies yielded mixed results and the observed risk reductions were not statistically significant (RR=0.994, 95% CI: 0.964, 1.024). For prostate cancer, solid evidence is still lacking for an association with the vitamin D nutritional status.
The picture for pancreatic cancer is even more complicated. Laboratory studies suggest that vitamin D plays a significant role in both function and dysfunction of the pancreas. Pancreatic cells possess VDR and express CYP27B1 (calcidiol 1α-hydroxylase). Calcitriol appears to be involved in the regulation of insulin synthesis, release, and function. Vitamin D metabolites and synthetic analogs inhibit pancreatic cell line growth and promote apoptosis of pancreatic cancer cells in vitro. Furthermore, over the past 7 years, several ecological studies have suggested an inverse relationship between UVB exposure (and presumably vitamin D status) and the incidence of pancreatic cancer Citation38Citation39Citation40Citation41Citation42. In light of this background the results of recent studies were totally unexpected.
A nested study of Finnish male smokers (part of the α-tocopherol, β-carotene, ATBC Study) revealed that higher calcidiol levels are associated with a nearly threefold rise in the incidence of pancreatic cancer Citation43. Also, a prospective study suggests that individuals with consistently high calcidiol levels are at a significantly higher risk for pancreatic cancer relative to those with adequate or low levels. However, there was no concentration-response relationship Citation44.
Further, a pooled nested case-control study of patients from eight cohorts within the Cohort Consortium VDPP of Rarer Cancers evaluated whether prediagnostic serum calcidiol levels were associated with the development of pancreatic cancer. During a median follow-up period of 6.5 years, 952 cases of pancreatic adenocarcinoma cases occurred among participants. The control group consisted of 1,333 participants matched within each cohort for age, sex, race, and so on. Overall, after adjusting for other risk factors (smoking, obesity, and diabetes), a circulating calcidiol level greater than 40 ng/mL (100 nmol/L) was associated with a statistically significant twofold increase in the risk for pancreatic cancer Citation45.
Daily vitamin D intake
At present, there are no established guidelines for dosing vitamin D in the various patient populations (infants, children, adolescents, young adults, seniors, pregnant, lactating, or menopausal women) that take into account clinical information acquired in recent years as well as the factors that determine effective UVB exposure (latitude, season, clothing and skin area exposure, skin pigmentation) and other risk factors for vitamin D deficiency such as obesity, old age, smoking, liver and chronic kidney disease, and certain drugs (steroids, barbiturates, and anticonvulsants). However, an evaluation of recently published literature suggests that the currently recommended daily allowances are probably too low and that higher doses are required to achieve the best outcomes at least in terms of bone health and colorectal cancer. Until revised, optimal vitamin D intakes are defined and due to the multiplicity and complexity of the factors that determine net vitamin D input, it appears reasonable based on available data to aim for a serum calcidiol level between 30 and 40 ng/mL (75–100 nmol/L) and modify the daily vitamin D supplement as necessary to achieve this level. Once reached, this level may be maintained in adults with a daily vitamin D3 dose of 1,000–2,000 IUs Citation46.
Adolescents (10–17 years) and seniors (≥65 years) may require higher doses (≥2,000 IUs/day). For children in the first year of life, there are data suggesting significant benefits from a daily vitamin D3 dose of 2,000 IUs. A Finnish study of over 10,000 children found that a daily dose of 2,000 IUs in the first 12 months of life reduced the risk of type I diabetes by 78% in the following 31 years of life Citation47Citation48Citation49.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
References
- History of Vitamin D. Available from: http://vitamind.ucr.edu/history.html [cited 1 October 2010].
- Unveiling the Enigma of Vitamin D. Available from: http://www.beyonddiscovery.org/content/view.txt.asp?a=414 [cited 1 October 2010].
- Holick MF. Vitamin D deficiency. N Engl J Med. 2007; 357: 266–81.
- Daniel D. Bikle . Endotext website. Chapter 3 – Vitamin D: Production, metabolism, and mechanisms of action. Available from: http://www.endotext.org/parathyroid/parathyroid3/parathyroid3.htm [cited 1 October 2010].
- Nabeshima Y. Discovery of alpha-Klotho unveiled new insights into calcium and phosphate homeostasis. Proc Jpn Acad Ser B Phys Biol Sci. 2009; 85: 125–41.
- Masuda S, Byford V, Arabian A, Sakai Y, Demay MB, St-Arnaud R, et al.. Altered pharmacokinetics of 1,25-dihydroxyvitamin D3 and 25-hydroxy vitamin D3 in the blood and tissues of the 25-hydroxyvitamin D-24-hydroxylase (CYP24A1) null mouse. Endocrinology. 2005; 146: 825–34.
- Köstner K, Denzer N, Müller CS, Klein R, Tilgen W, Reichrath J. The relevance of vitamin D receptor (VDR) gene polymorphisms for cancer: a review of the literature. Anticancer Res. 2009; 29: 3511–36.
- Bid HK, Mishra DK, Mittal RD. Vitamin-D receptor (VDR) gene (Fok-I, Taq-I & Apa-I) polymorphisms in healthy individuals from North Indian population. Asian Pac J Cancer Prev. 2005; 6: 147–52.
- Larcombe LA, Orr PH, Lodge AM, Brown JS, Dembinski IJ, Milligan LC, et al.. Functional gene polymorphisms in Canadian aboriginal populations with high rates of tuberculosis. J Infect Dis. 2008; 198: 1175–9.
- Fleet JC. Vitamin D receptors: not just in the nucleus anymore. Nutr Rev. 1999; 57: 60–3.
- Nemere I, Schwartz Z, Pedrozo H, Sylvia VL, Dean DD, Boyan BD. Identification of a membrane receptor for 1,25-dihydroxyvitamin D3 which mediates rapid activation of protein kinase C. J Bone Miner Res. 1998; 13: 1353–9.
- Khanal R, Nemere I. Membrane receptors for vitamin D metabolites. Crit Rev Eukaryot Gene Expr. 2007; 17: 31–47.
- Smolders J, Damoiseaux J, Menheere P, Hupperts R. Vitamin D as an immune modulator in multiple sclerosis, a review. J Neuroimmunol. 2008; 194: 7–17.
- Ascherio A, Munger KL, Simon KC. Vitamin D and multiple sclerosis. Lancet Neurol. 2010; 9: 599–612.
- Ben-Zvi I, Aranow C, Mackay M, Stanevsky A, Kamen DL, Marinescu LM, et al.. The impact of vitamin D on dendritic cell function in patients with systemic lupus erythematosus. PLoS One. 2010; 5: e9193.
- Takiishi T, Gysemans C, Bouillon R, Mathieu C. Vitamin D and diabetes. Endocrinol Metab Clin North Am. 2010; 39: 419–46.
- Marjamäki L, Niinistö S, Kenward MG, Uusitalo L, Uusitalo U, Ovaskainen ML, et al.. Maternal intake of vitamin D during pregnancy and risk of advanced beta cell autoimmunity and type 1 diabetes in offspring. Diabetologia. 2010; 53: 1599–607.
- Miller J, Gallo RL. Vitamin D and innate immunity. Dermatol Ther. 2010; 23: 13–22.
- Medzhitov R. Recognition of microorganisms and activation of the immune response. Nature. 2007; 449: 819–26.
- Kindt TJ, Goldsby RA, Osborne BA. Innate immunity. Chapter 3 in Kuby Immunology6th ed. W.H. Freeman & Company. NY, 2007
- Bartley J. Vitamin D, innate immunity and upper respiratory tract infection. J Laryngol Otol. 2010; 13: 1–5.
- Gombart AF. The vitamin D-antimicrobial peptide pathway and its role in protection against infection. Future Microbiol. 2009; 4: 1151–65.
- Wang TT, Nestel FP, Bourdeau V, Nagai Y, Wang Q, Liao J, et al.. Cutting edge: 1,25-dihydroxyvitamin D3 is a direct inducer of antimicrobial peptide gene expression. J Immunol. 2004; 173: 2909–12.
- Schauber J, Dorschner RA, Coda AB, Buchau AS, Liu PT, Kiken D, et al.. Injury enhances TLR2 function and antimicrobial peptide expression through a vitamin D-dependent mechanism. J Clin Invest. 2007; 117: 803–11.
- Krutzik SR, Hewison M, Liu PT, Robles JA, Stenger S, Adams JS, et al.. IL-15 links TLR2/1-induced macrophage differentiation to the vitamin D-dependent antimicrobial pathway. J Immunol. 2008; 181: 7115–20.
- Daniel C, Sartory NA, Zahn N, Radeke HH, Stein JM. Immune modulatory treatment of trinitrobenzene sulfonic acid colitis with calcitriol is associated with a change of a T helper (Th) 1/Th17 to a Th2 and regulatory T cell profile. J Pharmacol Exp Ther. 2008; 324: 23–33.
- Correale J, Ysrraelit MC, Gaitán MI. Immunomodulatory effects of vitamin D in multiple sclerosis. Brain. 2009; 132: 1146–60.
- Jones G. Pharmacokinetics of vitamin D toxicity. Am J Clin Nutr. 2008; 88: 582S–586S.
- Fiscella K, Franks P. Vitamin D, race, and cardiovascular mortality: findings from a national US sample. Ann Fam Med. 2010; 8: 11–8.
- Ginde AA, Scragg R, Schwartz RS, Camargo CA Jr. Prospective study of serum 25-hydroxyvitamin D level, cardiovascular disease mortality, and all-cause mortality in older U.S. adults. J Am Geriatr Soc. 2009; 57: 1595–603.
- Giovannucci E, Liu Y, Hollis BW, Rimm EB. 25-hydroxyvitamin D and risk of myocardial infarction in men: a prospective study. Arch Intern Med. 2008; 168: 1174–80.
- Lee JH, O'Keefe JH, Bell D, Hensrud DD, Holick MF. Vitamin D deficiency: an important, common, and easily treatable cardiovascular risk factor?. J Am Coll Cardiol. 2008; 52: 1949–56.
- Byers T. Anticancer vitamins du jour – The ABCED's so far. Am J Epidemiol. 2010; 172: 1–3.
- Mohr SB, Garland CF, Gorham ED, Grant WB. Could ultraviolet B irradiance and vitamin D be associated with lower incidence rates of lung cancer?. J Epidemiol Community Health. 2008; 62: 69–74.
- Garland CF, Garland FC, Gorham ED, Lipkin M, Newmark H, Mohr SB, et al.. The role of vitamin D in cancer prevention. Am J Public Health. 2006; 96: 252–61.
- Li H, Stampfer MJ, Hollis JB, Mucci LA, Gaziano JM, Hunter D, et al.. A prospective study of plasma vitamin D metabolites, vitamin D receptor polymorphisms, and prostate cancer. PLoS Med. 2007; 4: e103.
- Wactawski-Wende J, Kotchen JM, Anderson GL, Assaf AR, Brunner RL, O'Sullivan MJ, et al.. For Women's Health Initiative Investigators. Calcium plus vitamin D supplementation and the risk of colorectal cancer. N Engl J Med. 2006; 354: 684–96.
- Lappe JM, Travers-Gustafson D, Davies KM, Recker RR, Heaney RP. Vitamin D and calcium supplementation reduces cancer risk: results of a randomized trial. Am J Clin Nutr. 2007; 85: 1586–91.
- International Agency for Research on Cancer. (2008). Vitamin D and cancer. IARC Working Group Reports. Vol. 5. LyonFrance: International Agency for Research on Cancer. Available from: http://www.iarc.fr/en/publications/pdfs-online/wrk/wrk5/Report_VitD.pdf [cited 27 November 2010]..
- Boscoe FP, Schymura MJ. Solar ultraviolet-B exposure and cancer incidence and mortality in the United States, 1993–2002. BMC Cancer. 2006; 6: 264. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1665523/?tool=pubmed [cited 27 November 2010].
- Grant WB. An ecologic study of cancer mortality rates in Spain with respect to indices of solar UVB irradiance and smoking. Int J Cancer. 2007; 120: 1123–8.
- Tuohimaa P, Pukkala E, Scélo G, Olsen JH, Brewster DH, Hemminki K, et al.. Does solar exposure, as indicated by the non-melanoma skin cancers, protect from solid cancers: vitamin D as a possible explanation. Eur J Cancer. 2007; 43: 1701–12.
- Stolzenberg-Solomon RZ, Vieth R, Azad A, Pietinen P, Taylor PR, Virtamo J, et al.. A prospective nested case-control study of vitamin D status and pancreatic cancer risk in male smokers. Cancer Res. 2006; 66: 10213–9.
- Stolzenberg-Solomon RZ, Hayes RB, Horst RL, Anderson KE, Hollis BW, Silverman DT. Serum vitamin D and risk of pancreatic cancer in the prostate, lung, colorectal, and ovarian screening trial. Cancer Res. 2009; 69: 1439–47.
- Stolzenberg-Solomon RZ, Jacobs EJ, Arslan AA, Qi D, Patel AV, Helzlsouer KJ, et al.. Circulating 25-hydroxyvitamin D levels and risk of pancreatic cancer: cohort consortium vitamin D pooling project of rarer cancers. Am J Epidemiol. 2010; 172: 81–93.
- Bischoff-Ferrari HA, Giovannucci E, Willett WC, Dietrich T, Dawson-Hughes B. Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. Am J Clin Nutr. 2006; 84: 18–28.
- Hyppönen E, Läärä E, Reunanen A, Järvelin MR, Virtanen SM. Intake of vitamin D and risk of type 1 diabetes: a birth-cohort study. Lancet. 2001; 358: 1500–3.
- Heaney RP. The vitamin D requirement in health and disease. J Steroid Biochem Mol Biol. 2005; 97: 13–9.
- Brekke HK, Ludvigsson J. Vitamin D supplementation and diabetes-related autoimmunity in the ABIS study. Pediatr Diabetes. 2007; 8: 11–4.