Patients with Kidney transplants are known to be at increased risk of non-tuberculous mycobacterial infections (Citation1–Citation3). This can take the form of skin infection, lung infection and more seriously disseminated disease. The increased risk is related to the reduced cellular immunity due to immune suppressant drugs. Very little is known about the risk of Kidney transplantation in patients who are already known to have Non-tuberculous mycobacterial infection.
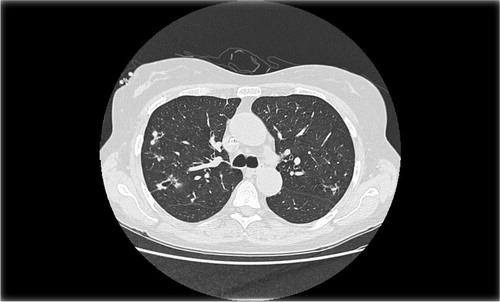
A 55-year-old female known with CKD5 on haemodialysis secondary to Anti-Glomerular Basement Membrane (anti-GBM) disease was referred to the chest clinic because of an incidental finding of a small cavitation lesion at the right upper lung zone. At the time, she had no symptoms related to her chest although she did have history of chest infection in the past. Computerised Tomography (CT) scan demonstrated scattered bronchocentric nodules in the upper lobes with some areas of cavitation (). Bronchoscopic bronchial lavage was smear positive for acid fast bacilli and culture grew Mycobacterium avium complex (MAC).
A diagnosis of pulmonary infection with MAC was made, and she was started on a treatment regimen of a combination of clarithromycin 500 mg twice daily, rifampicin 600 mg once daily, and ethambutol 1,300 mg three times a week to be taken in the evening preceding the dialysis day. This was based on 55 kg dry weight. We planned to give her a course of 2 years. However, she was very keen to proceed with live donor renal transplant. Consultation of the literature did not give any clinical guidance to manage such a situation. After consultation with international experts in the UK and US, we decided to monitor her response to treatment, and if her condition was controlled, we decided to proceed with transplantation after 9 months of therapy. During the following 9 months of treatment, her chest remained stable and she had no respiratory symptoms, and she remained very keen to proceed with the renal transplant after detailed discussions about risk benefit. A repeat CT chest showed improvement in some pulmonary opacities while others remained unchanged. There was no evidence of new lesions.
Based on stability of her condition and reassuring CT scan, she proceeded with live donor renal transplant. Immune suppression was given with tacrolimus 5 mg am and 6 mg pm and mycophenolate 540 mg bd while MAC infection treatment was continued on the same regimen.
She remained under monitoring and follow-up both clinically and radiologically (chest X rays) at the Mycobacterial Infections Clinic. Her chest remained stable and asymptomatic, she reported no sputum production, and so culture for mycobacteria was not repeated. She completed a 2 years course of treatment following which we continued to monitor her with no sign of relapse.
Conclusion
We believe that this is the first case of renal transplant in a patient already known with MAC pulmonary infection controlled with treatment. The timing of transplant was difficult. She was very keen to progress with the transplant as early as possible. Obviously it was not possible to progress with transplant until we were confident that her disease was well controlled on treatment. Six to nine months of effective treatment seemed reasonable but was not based on concrete evidence. We felt it is important to share this experience with colleagues interested in this field.
Patient consent
The patient kindly consented for her case to be published anonymously.
Mycobacterial Infections Clinic
Department of Respiratory Medicine
Salford Royal NHS Foundation Trust
Salford, UK
Kay Lavery
Mycobacterial Infections Clinic
Department of Respiratory Medicine
Salford Royal NHS Foundation Trust
Salford, UK
Magde Gornasa
Mycobacterial Infections Clinic
Department of Respiratory Medicine
Salford Royal NHS Foundation Trust
Salford, UK
Tina Wilding
Mycobacterial Infections Clinic
Department of Respiratory Medicine
Salford Royal NHS Foundation Trust
Salford, UK
Anna Walsham
Department of Radiology
Salford Royal NHS Foundation Trust
Salford, UK
Edmond O'Riordan
Department of Renal Medicine
Salford Royal NHS Foundation Trust
Salford, UK
References
- Longworth SA, Vinnard C, Lee I, Sims KD, Barton TD, Blumberg EA. Risk factors for nontuberculous mycobacterial infections in solid organ transplant recipients: a case-control study. Transpl Infect Dis. 2014; 16: 76–83.
- Haas S, Scully B, Cohen D, Radhakrishnan J. Mycobacterium avium complex infection in kidney transplant patients. Transpl Infect Dis. 2005; 7: 75–9.
- Piersimoni C. Nontuberculous mycobacteria infection in solid organ transplant recipients. Eur J Clin Microbiol Infect Dis. 2012; 31: 397–403.