Abstract
Introduction: Inadequate nutritional support after mechanical circulatory device placement is known to increase postoperative infections and to decrease survival. The extracorporeal membrane oxygenation (ECMO) patients with complicated postoperative recovery may require long-term nutritional support using percutaneous endoscopic gastrostomy (PEG) tube feeding. In this study, the feasibility of PEG procedure on patients on ECMO was evaluated.
Methods: Between November 2010 and July 2012, 43 patients were placed on venoarterial or venovenous ECMO for cardiogenic shock or severe respiratory failure. All of the long-term ECMO patients were supported with tube feeding. Four patients underwent PEG tube placement for long-term nutritional support while they were on ECMO. Procedure management consisted of cessation of anticoagulation 12 hours before and 12 hours after procedure. Anticoagulation was continued while on ECMO. Data were retrospectively analyzed to investigate complications related to the PEG placement.
Results: The studied patients consisted of two males and two females with a mean age of 55.5±7.9 years. The interval of ECMO to PEG placement was a mean 16.8±4.2 days. The mean total length of ECMO support for these patients was 22.7±5.6 days. PEG was successfully performed in the operating room or bedside in all patients. There were no ECMO-device-related issues during or after the PEG procedure. There were no postoperative short-term or long-term PEG-related complications, such as, acute gastric bleeding or dislodgement of the PEG tube.
Conclusions: PEG placement for ECMO patients can be done without increasing the risk of device or intra-abdominal organ injury with carefully coordinated efforts from both the intensive care team and surgical services.
Introduction
Inadequate nutritional support after mechanical circulatory device placement is known to increase postoperative infections and mortality. Patients in this intensive care setting are hypercatabolic, which makes an emphasis on nutrition crucial. An enteral route is preferred over parenteral to maintain gastrointestinal integrity and to prevent morbidity directly related to parenteral support, such as parenteral nutrition-associated liver disease, and infection Citation1 Citation2. Most hospital protocols call for the placement of nasogastric tubes (NGTs) to provide enteral access for nutritional support in patients with these devices. NGTs have been linked to interruption of the lower esophageal sphincter, which can lead to aspiration pneumonia, gastrointestinal bleeding, and esophagitis Citation3. In patients requiring ventilator assistance, higher rates of ventilator-associated pneumonia were found among patients with NGTs vs. percutaneous endoscopic gastrostomy (PEG) tubes Citation4. In addition, repeated removal and re-insertion of the NGT may inflict nasopharyngeal trauma, which may occasionally require nasopharyngeal packing by otolaryngology specialty service. This leads to interruption of crucial nutritional support and leads to an increased risk of developing infection, which may further contribute other organ failure. Compared to NGTs, PEG tube placement provides consistent nutritional support with less risk of the above-mentioned complications and low risk of procedure-related complications Citation5 Citation6.
In the past, there have been concerns about intra-operative and postoperative gastrointestinal bleeding with PEG placement in patients on constant anticoagulation for life support devices, such as extracorporeal membrane oxygenation (ECMO). Titrating an ECMO patient off of anticoagulation for PEG placement raised concerns for clotting and dysfunction of the ECMO device. The ECMO patients with complicated postoperative recovery may require long-term nutritional support using tube feedings. Placement of a PEG in the ECMO patient requires knowledge of the anticoagulation management. In our institution, ECMO anticoagulation protocol was established Citation7. Using this protocol, PEG placement was performed in selected ECMO patients who required long-term nutritional support. Current study was performed to assess the feasibility of PEG procedure on the patient on ECMO.
Methods
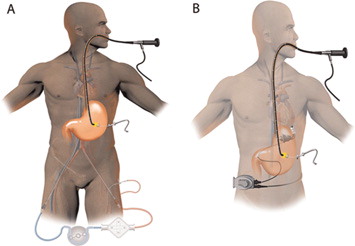
Between November 2010 and July 2012, 43 patients underwent peripherally cannulated venoarterial or venovenous ECMO placement for cardiogenic shock or severe respiratory failure in our institution with the end goal of bridge to recovery, bridge to ventricular assist device, or bridge to decision. Among them, 18 patients required 10 days or more of ECMO support. All of the long-term ECMO patients were supported with tube feeding. Four patients underwent PEG tube placement for long-term nutritional support while they were on ECMO. Tube feeding was held 6–8 hours prior to procedure. Other procedure management consisted of cessation of anticoagulation 12 hours before and 12 hours after the procedure. Procedure was performed either in the intensive care unit or in the operating room, depending on the previous history of abdominal surgery. An intensivist, who was primarily taking care of the patient, was present during the procedure. If the patients were considered to be ventricular assist device candidates, the left mid abdomen would be the preferred area for PEG because the upper left quadrant would be occupied by the device and the drive line. The location of the PEG stoma was discussed with the cardiac surgeon, the abdominal surgeon, and the intensivist (). During the PEG procedure, one dose of short-acting muscular relaxant and intravenous sedatives was administered. The procedure was done in standard fashion. Anticoagulation was restarted 12 hours after the procedure and continued while on ECMO, aiming partial thrombin time (PTT) of 45–55 sec. Tube feed via PEG tube was restarted 6 hours after procedure. Data were retrospectively analyzed to investigate complications related to the PEG placement. This study was approved by the internal review board.
Fig. 1. Illustration shows typical percutaneous gastrostomy (PEG) procedure on the patient on venoarterial: extracorporeal membrane oxygenation (ECMO) on left (A), and PEG procedure on the patient with HeartMate II left ventricular assist device (LVAD) on right (B). Prior PEG procedure, an intensivists draw line for the anticipate LVAD placement, which should not overlap to the PEG stoma.
Results
The studied patients consisted of two males and two females with mean age of 55.5±7.9 years Table 1. The mean interval of ECMO to PEG placement was 16.8±4.2 days. The mean total length of ECMO support for these patients was 22.7±5.6 days. All of the patients were on tube feedings of some sort prior to PEG. One patient had nasopharyngeal trauma from the transesophageal echocardiography (TEE) requiring multiple transfusions despite of lowering the anticoagulation goal. PEG was successfully performed in the operating room or bedside in all patients. There were no ECMO device issues related to the PEG procedure. No additional membranous oxygenator exchanges were required after temporally stopping anticoagulation for the PEG procedure. There were no postoperative short-term or long-term PEG-related complications, such as, acute gastric bleeding or dislodgement of the PEG tube. The prealbumin level improved appropriately after PEG.
Table 1. Patients demographics
Discussion
Once bleeding complication occurs in ECMO patients, medical management becomes a difficult, although not impossible, task. Anticoagulation can be held short period of time to control hemostasis; however, it is not possible to completely stop anticoagulation while on ECMO due to the risk of device clotting. This directly causes hemodynamic and respiratory compromise.
All four patients were on ECMO for more than 5 days and required a steady, reliable source of nutritional support. Parenteral nutrition remains an option but not preferred over enteral nutrition. With parenteral nutrition comes an increased risk of access site infection and subsequent bacteremia and sepsis. In addition, some patients on long-term parenteral nutrition may develop parenteral nutrition-associated liver disease Citation2. Early initiation of enteral support remains the goal. There has been some concern over early initiation of enteral nutritional support in patients on ECMO. Three studies explored initiation of enteral support within the first 24–48 hours. Two studies showed tolerance of early enteral feeding while on ECMO with no adverse effects directly attributable to enteral feeding Citation8 Citation9.
In most settings, nutrition by NGT is standard, as long as NGT access is established and maintained. One of the many problems that arise in ECMO patients is the need for repeated TEE to assess cardiac function. During TEE, the NGT is removed to optimize imaging and is reinserted after. Nasopharyngeal trauma could occur after multiple blind instrumentations. Each of the four patients in this study had some degree of the nasopharyngeal trauma from the multiple instrumentations; the team solved this problem with the use of PEG. Even though PEG requires surgical intervention, it is a relatively low-risk procedure, as long as surgical site bleeding is kept under control Citation1. From our experience, the most frequent sites of bleeding for ECMO patients are surgical sites, including cannulation sites and recent surgical sites Citation7. Anticoagulation regimens were designed, as described above, to allow for PEG placement without excessive risk of bleeding and/or clotting in the ECMO device. Zero out of four patients suffered from PEG-procedure-related complications.
All PEG procedures for the ECMO patients were performed at the bedside with ECMO intensivists in the room. Strict anticoagulation management allowed PEG procedure to perform without complications and allowed ECMO to continue to run safely.
Conclusions
PEG placement for ECMO patients can be done without increasing the risk of device or intra-abdominal organ injury with carefully coordinated efforts from both the intensive care team and surgical services.
Conflict of interest and funding
There is no conflict of interest in the present study for any of the authors.
References
- McClave SA, Martindale RG, Vanek WV, McCarthy M, Roberts P, Taylor B. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (ASPEN). JPEN J Parenter Enteral Nutr. 2009; 33: 277–316. 10.1177/0148607109335234.
- Xu ZW, Li YS. Pathogenesis and treatment of parenteral nutrition-associated liver disease. Hepatobiliary Pancreat Dis Int. 2012; 11(6): 586–93. 10.1016/S1499-3872(12)60229-X.
- Newton M, Burnham WR, Kamm MA. Morbidity, mortality, and risk factors for esophagitis in hospital inpatients. J Clin Gastroenterol. 2000; 30: 264–9. 10.1097/00004836-200004000-00012.
- Kostadima E, Kaditis AG, Alexopoulos EI, Zakynthinos E, Sfyras D. Early gastrostomy reduces the rate of ventilator-associated pneumonia in stroke or head injury patients. Eur Respir J. 2005; 26: 106–11. 10.1183/09031936.05.00096104.
- Park RH, Allison MC, Lang J, Spence E, Morris AJ, Danesh BJ. Randomized comparison of percutaneous endoscopic gastrostomy and nasogastric tube feeding in patients with persisting neurological dysphagia. BMJ. 1992; 304(6839): 1406.10.1136/bmj.304.6839.1406.
- Payne KM, King TM, Eisenach JB. The technique of percutaneous endoscopic gastrostomy. A safe and cost-effective alternative to operative gastrostomy. J Crit Illn. 1991; 6: 611–9.
- Lamb K, Cowan S, Evans N, Pitcher H, Moritz T, Lazar M, Successful management of bleeding complications in patients supported with extracorporeal membrane oxygenation with primary respiratory failure. Perfusion. 2012. [Epub ahead of print].
- Scott LK, Boudreaux K, Thaljeh F, Grier LR, Conrad SA. Early enteral feeding in adults receiving venovenous extracorporeal membrane oxygenation. JPEN J Parenter Enteral Nutr. 2004; 28: 295–300. 10.1177/0148607104028005295.
- Lukas G, Davies AR, Hilton AK, Pellegrino VA, Scheinkestel CD, Ridley E. Nutritional support in adult patients receiving extracorporeal membrane oxygenation. Crit Care Resusc. 2010; 12: 230–4.