Abstract
Background: Despite the prevalence of medical interpreting in the clinical environment, few medical professionals receive training in best practices when using an interpreter. We designed and implemented an educational workshop on using interpreters as part of the cultural competency curriculum for second year medical students (MSIIs) at David Geffen School of Medicine at UCLA. The purpose of this study is two-fold: first, to evaluate the effectiveness of the workshop and second, if deficiencies are found, to investigate whether the deficiencies affected the quality of the patient encounter when using an interpreter.
Methods: A total of 152 MSIIs completed the 3-hour workshop and a 1-station objective-structured clinical examination, 8 weeks later to assess skills. Descriptive statistics and independent sample t-tests were used to assess workshop effectiveness.
Results: Based on a passing score of 70%, 39.4% of the class failed. Two skills seemed particularly problematic: assuring confidentiality (missed by 50%) and positioning the interpreter (missed by 70%). While addressing confidentiality did not have a significant impact on standardized patient satisfaction, interpreter position did.
Conclusion: Instructing the interpreter to sit behind the patient helps sustain eye contact between clinician and patient, while assuring confidentiality is a tenet of quality clinical encounters. Teaching students and faculty to emphasize both is warranted to improve cross-language clinical encounters.
Introduction
According to 2000 US Census data, 47 million people aged 5 and over speak a language other than English at home. Of those 47 million, nearly 50% indicate that they speak English less than ‘very well’ Citation1 and are often identified as Limited English Proficiency (LEP). These individuals may experience difficulties speaking, reading, writing, or understanding the English language that prevents them from participating fully in society Citation2. The LEP patient population is increasing in the USA, particularly in urban areas, such as Los Angeles County, where almost 2.5 million residents (48.3%) aged 5 and older speak English less than ‘very well Citation3.’ Despite the growing need for interpreter services, few clinicians ever receive training in the effective use of interpreters.
To ensure the health of LEP patients, Title VI of the Civil Rights Act of 1964 requires all federally funded healthcare organizations to provide LEP patients with interpretation services by bilingual staff or professionally trained interpreters Citation4. When caring for an LEP patient, lack of a common shared language between patient and healthcare provider can jeopardize the effectiveness of a clinical encounter, regardless of the provider's medical knowledge, use of cutting edge technology, or overall clinical competence Citation5Citation6. Studies indicate that use of professionally trained interpreter services is associated, in general, with better health outcomes, whereas LEP patients who do not receive trained interpreter services have increased medical tests, greater test cost, and an increased risk of hospitalization Citation7. Use of interpreter services helps preserve the integrity of the LEP patient–physician encounter.
Given these legal and ethical grounds for using interpreter services when interviewing an LEP patient, how an interpreter affects the patient encounter is of high concern for healthcare providers. Many have noted that any interaction with an interpreter increases the chance of a breech in patient confidentiality Citation8. Also troubling is the potential adverse effect of an interpreter on the ‘patient-centeredness’ of a clinic visit. Rivadeneyra et al. Citation9 found that physicians elicit fewer patient concerns when using an interpreter to communicate with LEP patients than when communicating directly with English-speaking patients. In addition, interpreters may affect patient satisfaction with the clinical encounter. In a study involving Spanish-speaking patients seen in a public hospital emergency department, Baker et al. Citation10 found that patients who used an interpreter or felt they needed an interpreter though none was provided rated their provider as significantly less friendly and less respectful, and indicated less comfort with the provider.
In a 2003 study, Flores et al. Citation11 found that only a quarter of US teaching hospitals offered training in working with interpreters, and the majority that did offer a course treated it as optional. In medical education, many have emphasized the need for training medical students and residents in the use of interpreter services as part of a standard cultural competency curriculum Citation12Citation13Citation14Citation15. Despite this recent emphasis, few examples of such training exist in the literature Citation16.
In the review of our own pre-doctoral education structure, the curriculum development team discovered that instruction on working with interpreters was lacking where it was needed most, that is, prior to the start of clinical rotations. Recognizing this need, course directors for our longitudinal Doctoring curriculum, a special feature of the UCLA School of Medicine curriculum, developed a ‘Working with Interpreters’ Workshop, incorporating it into the second-year medical student curriculum. Doctoring first, second, third, and fourth (which take place over the entire four-year curriculum) are year-long case-based learning courses that focus on the development of professional behaviors, clinical skills, and a biopsychosocial perspective on patient care and lifelong learning. Goals of the Doctoring curriculum are to provide a broad foundation for clinical medicine that is not discipline specific. Topics covered include doctor–patient communication, clinical decision making, ethics, health economics, and epidemiology. Each year of the Doctoring curriculum has its own distinct focus while reinforcing certain topics from the previous year. The year two Doctoring curriculum specifically aims to provide students with an understanding of the health needs of different communities and to develop skills and knowledge about patient-centered approaches to clinical care. These charges are also part of the larger theme of the cultural competency curriculum embedded throughout the four-year curriculum. Doctoring course directors felt that instruction on working with interpreters would fit well with the overall themes of the year two Doctoring course and also afford the opportunity to provide all students with a standardized foundation in the use of interpreters prior to dispersing across southern California to the various UCLA clinical rotation sites.
In 2005, working with the curriculum development team, course directors implemented a 3-hour interpreter-use training workshop entitled ‘Working with Interpreters’ following guidelines proposed by Ethan Wiener and Maria Rivera in their paper ‘Bridging language barriers: how to work with an Interpreter Citation17.’ This second-year medical student workshop provided a step-by-step guidance to best practices in working with an interpreter. While the Wiener and Rivera article outlined for healthcare providers the importance of medical interpreting by a qualified interpreter, most importantly for the workshop, the authors identified specific behaviors for physicians when using a medical interpreter, from pre-interview arrangements with the interpreter to proper positioning and medical interview techniques during the interview (summarized in ).
Fig. 1. Summary of guidelines proposed by Wiener and Rivera Citation17.
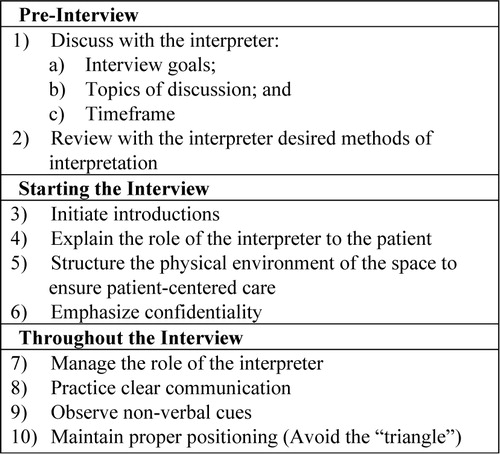
At the time, the Wiener and Rivera paper was unique in its discussion of the physical placement of the interpreter, or the seating arrangement, in a medical encounter, thereby addressing both the verbal and physical aspects of incorporating an interpreter into the medical interview.
Following a general overview of the importance of using qualified interpreters, Wiener and Rivera offer a step-by-step guide for medical professionals on using an interpreter during a patient interview. They emphasize the importance of structure, both of the interview itself and of the physical clinical environment. They also stress the importance of confidentiality and the need to discuss this first with the interpreter separately and then with the patient during the interview. In terms of the interview, Wiener and Rivera identify several strategies for properly structuring the interview and organizing the physical space. Wiener and Rivera go into great detail concerning the negative effects of the ‘triangle approach’ in medical interpreting, suggesting that the healthcare provider should avoid positioning the three interview participants – the patient, the physician, and the interpreter – in a triangle. Rather, the authors posit that the interpreter should be positioned to the side and slightly behind the patient in order to ensure maximum eye contact with the patient and preserve the integrity of the patient–physician encounter. The authors also list several pitfalls to medical interpreting and suggest language to avoid during an interview with an LEP patient and an interpreter.
With the Wiener and Rivera approach to integrating interpreters into the LEP patient encounter as a general framework, ‘The Working with Interpreters’ Workshop was incorporated into our standard Doctoring curriculum. The aim of this study was first to evaluate the effectiveness of our curricular innovation, the ‘Working with Interpreters’ workshop, in training students to better incorporate an interpreter into a LEP patient encounter as measured by performance on an Objective Structured Clinical Examination (OSCE). Second, this study aims to identify potential student behaviors that can negatively affect the quality of the patient encounter, as measured by standardized patient (SP) assessment of the physician–patient interaction (PPI), when using an interpreter.
Methods
Workshop description
Taught as part of a larger seminar on the clinical decision-making process within the Doctoring course curriculum, the 3-hour ‘Working with Interpreters’ Workshop incorporated several learning objectives, including awareness of our diverse patient population, knowledge of the complex issues involved in caring for an LEP patient, knowledge of the legal and ethical implications of treating immigrant patients, as well as the demonstrated ability to effectively use an interpreter and knowledge of available resources for LEP patients. The Doctoring course directors who designed the Interpreter Workshop created a faculty and student guide that included both a discussion of using interpreters and topical articles. The workshop guide also summarized the Wiener and Rivera suggestions for working with interpreters and included the paper. At the end of the guide, the course directors introduced a helpful, condensed list for students on how to conduct a patient interview using an interpreter, based on a synthesis of these materials.
Prior to the workshop, faculty instructors were asked to review the faculty guide and read all associated paper. A 1-hour faculty development session was held prior to the workshop, in which course directors reviewed the material with the faculty, emphasized the workshop learning objectives, and modeled the specific techniques referenced in the faculty guide. Course directors also reviewed the format of the workshop, which included large and small group activities, with all instructors to ensure a standardized experience for all students. Two faculty instructors, a clinician and a behavioral science professional, were assigned to each group of eight to nine students during a 3-hour session that featured demonstration and active student participation, as outlined in the workshop guide. Students first discussed with instructors how to conduct a patient interview using interpreter services, specifically touching on topics like setting roles and expectations for each participant. Instructors then demonstrated how best to conduct a cross-language interview using an interpreter with the aid of two actors, one playing an SP with LEP who spoke Spanish and the other acting as a standardized interpreter (SI). In this demonstration, students were taught how best to arrange seating, maintain eye contact, and adjust the style and length of their questions as well as approaches to assuring patient confidentiality. Two students with limited Spanish proficiency alternated conducting the interview while the group observed. Both the student interviewer and the instructors could pause the exercise at any time to discuss issues raised in the moment or elicit feedback from the group. Following the interview, students received immediate feedback from faculty instructors.
Measurement
We developed a one-station OSCE involving an SP and an SI to assess students’ competency in using interpreters. An OSCE is designed to simulate real clinical settings using trained actors, known as SPs, as patients with the intention of assessing specific skills expected within those settings. Students are given limited amount of time to complete the examination.
The OSCE case developed for the ‘Working with Interpreters’ Workshop involved an LEP patient presenting with a cough who requires an interpreter in order to communicate with the doctor. Students completed this one-station OSCE 8 weeks after the workshop as part of the Doctoring course final examination. Students had 20 minutes to complete the encounter. During the encounter, the SI displayed behaviors that could diminish the effectiveness of an interpreter in a patient encounter, such as editing, paraphrasing interpretations, and engaging in side conversations. In addition, the SP and the SI were purposefully situated in the room in a triangle, in direct opposition to the positioning standards put forth by Wiener and Rivera that had been taught to the students during the workshop. At the end of the interview, both the SP and the SI independently completed a checklist () assessing history taking and PPI.
Table 1. Combined SI and SP ‘Working with Interpreters’ OSCE checklist
The SP and SI each rated their ‘Overall Satisfaction’ with the encounter using one global item and a 6-point scale. The interaction quality component (PPI) consisted of five SP and SI combined items assessing quality of communication techniques on a 6-point scale. The history-taking component charted techniques used during the interview process and consisted of 12 yes/no items. Five of the history-taking items were specific to the experience of the SP, while the other seven were specific to the experience of the SI. While the items were organized into the SP perspective and SI perspective on the checklist, they can be further divided into three sub-categories for feedback purposes: setting the stage for the interview, managing interview logistics, and maintaining patient centeredness during the interview ().
Table 2. History items within subcategories of ‘Working with Interpreters’ checklist
Subjects
A convenience sample of 152 second-year medical students completed the workshop and the one-station OSCE at the end of their Doctoring course in 2005, resulting in 100% participation. This study received UCLA Institutional Review Board (IRB) exempt status.
Analysis
The results were analyzed using SPSS 15.0. Descriptive analyses were conducted to assess workshop effectiveness. The effect of omitted techniques on the quality of the encounter, as determined by the SP, was assessed using independent-sample t-tests.
Results
Workshop effectiveness was evaluated based on a passing score determined by the course directors of 70% or higher of total History Taking items completed and an average of 4 or above on PPI of the combined SP and SI checklist items. Failing either or both components would result in a ‘fail.’ Based on these criteria, 39.4% of the class failed the examination. However, on closer examination of student performance, the results did show some obvious strengths and weaknesses that can aid us in future planning. Students achieved an average score of 0.75 (SD = 0.14) in history taking and an average of 4.6 (SD = 0.67) out of a maximum 6 points in interaction quality (PPI) using items that incorporated both the SP and the SI's perspectives. Based on the anchors of the 6-point scale, a 4.6 average would put a majority of the students in between the categories of ‘Good’ and ‘Very Good.’ Of the three sub-categories, students did best in Management (M=0.87, SD = 0.16), followed by Patient Centeredness (M=0.73, SD = 0.27); they did worst in Setting the Stage (M=0.62, SD = 0.22). Based on those numbers, students did well in managing the encounter while still keeping the interaction patient-centered. They had more trouble with the details of preparing the encounter. A review of the item statistics showed that almost 70% of the class did not arrange the seating according to Wiener and Rivera's guidelines Citation17, in which the interpreter is positioned just slightly behind the patient, and 50% of the class did not address the issue of confidentiality before beginning the interview. Both techniques were discussed and modeled by instructors in the workshop as part of ‘Setting the Stage.’
Quality of the encounter
Though we collected both a measure of ‘Overall Satisfaction’ with the encounter and interaction quality (PPI), the 5-item PPI scale () included perspectives from both the SP and the SI. It also represented a more comprehensive behaviorally-based evaluation of the students’ communication skills than the more general single-item ‘Overall Satisfaction.’ Independent-sample t-tests were performed to explore the individual effect of the seating arrangement and the discussion of confidentiality on the overall quality of interaction as reported by the SP (three of the five PPI items). Students who arranged the seating according to the guidelines scored slightly but significantly higher (M=4.73, SD = 0.71) than those who did not (M=4.48, SD = 0.67), based on SP PPI scores (t=–2.116, df = 150, p<0.05). Although those who addressed confidentiality (M=4.62, SD = 0.69) scored higher than those who did not (M=4.49, SD = 0.68), the difference was not statistically significant.
Discussion
Health care professionals recognize the need for educational interventions that address delivering effective healthcare in cross-language situations. Implementation of ‘The Use of Interpreter’ Workshop afforded us the opportunity to do just that. Although almost 40% of the class failed the examination based on our strict passing standards, we achieved moderate success as students learned to employ various techniques to manage effectively the logistics of an interview involving an interpreter while maintaining patient-centeredness. We also identified two curricular elements not emphasized enough, which fall under the ‘Setting the Stage’ sub-category: (1) properly positioning the patient and the interpreter and (2) establishing issues of confidentiality.
Wiener and Rivera make a strong argument for positioning each party involved in the interview and advise against the ‘triangle approach’ Citation17, in which the interview participants are arranged in a triangle. About two-thirds of the class did not follow the recommended seating arrangement in the OSCE, despite discussion and demonstration of the proper technique during the workshop. Eye contact – as well as other non-verbal cues – is important in establishing rapport. Those who use ‘triangle positioning’ when interviewing may inadvertently break eye contact with the patient or miss vital facial cues, leading to poorer ratings of interaction quality. We suspected that although the guidelines stressed the importance of proper positioning in an LEP encounter, some of our faculty members underestimated the impact of chair arrangement and did not adequately emphasize it in their small group instruction. The faculty guide for the workshop, while including the paper, did not provide detailed descriptions of the methods outlined by Wiener and Rivera in the main body of the guide. Though the paper does include a diagram illustrating proper positioning, the faculty guide does not; perhaps the addition of this diagram to the text of the workshop guide and added emphasis on the importance of physical placement in an LEP interview might assist faculty in better conceptualizing the method in order to better explain to students the proper technique. The finding that students who did not rearrange seating as recommended scored significantly lower in interaction quality provides support for Wiener and Rivera's claim that chair arrangement does make a difference in the quality of the encounter. The SPs reported feeling more supported and respected by students who initiated proper positioning of the interpreter during the interaction. In the future, we hope students and faculty instructors alike place more emphasis on this aspect of the cross-language interview.
Since the establishment of professional medical interpretation services, much effort has been put into the development of uniform codes of ethics Citation8. The importance of addressing issues of confidentiality is also emphasized by The Association of American Medical Colleges in their ‘Guidelines for the Use of Medical Interpreter Services’ Citation18. Although failure to assure confidentiality did not produce a devastating effect on encounter quality, based on SP ratings, it is not clear whether this would be true with actual patients. Alternatively, an LEP patient may consider a healthcare provider's verbal assurance of confidentiality as less important than conveying information, making this less damaging to the overall quality of the interaction. Regardless of the reasoning behind failure to address confidentiality during an LEP patient encounter, it is an essential component that must be addressed when interpreters are involved; failure to do so may result in ethical or legal ramifications.
This was a single-institution case study; baseline data were not ascertained. Although the techniques measured were not case specific, the examination only consisted of one case. Generalization of our findings to other cases can not be established. More cases are needed to achieve an acceptable level of reliability index. The study should be replicated at other institutions in order to confirm and generalize findings.
Conclusion
In summary, implementing a workshop on working with interpreters provided much needed instruction for our students while closing a gap in our pre-clinical curriculum. The effect of this was easily evaluated using SP encounters. This study also illuminated the importance of proper faculty development to the success of the workshop. Many of the errors made by students as evaluated by the SPs and Sis, could be attributed to our instructors’ under emphasis of some of the key learning objectives during the workshop. For instance, the learning objective related to interpreter use, phrased as ‘[developing] skills necessary to use an interpreter (including interpreter accuracy, sensitivity, and confidentiality)’ and ‘Demonstrate effective and efficient communication skills when encountering a LEP patient’ might have been too general for faculty and students. Specifically listing particular skills as emphasized in the Wiener and Rivera paper might improve the overall structure of the session and better direct faculty when instructing students in proper interview techniques while using an interpreter.
Our findings also bolster support for various recommended techniques when using an interpreter, such as the proper positioning of the interpreter. Although there are different approaches toward positioning of the interpreter in practice, our data suggest Wiener and Rivera's guidelines for positioning the interpreter produce higher patient satisfaction with the encounter. In order to generalize these findings to a wider population (i.e., physicians in practice), further studies exploring the impact of proper techniques in working with an interpreter from speaking slowly and avoiding medical jargon to physically arranging the room, are crucial.
Acknowledgements
The authors would like to thank Vicky Mays, PhD, MSPH, and LuAnn Wilkerson, EdD for their editorial assistance reviewing our manuscript and their ongoing support.
Conflict of interest and funding
All authors gratefully acknowledge K07 funding from the National Heart Lung and Blood Institute (NHLBI). This project was supported in part by NHLBI award #K07HL79240-5 ‘Linking Health Disparities Research to Medical Education.’ Part of this research was made possible by a pre-doctoral advanced quantitative methodology training Grant (#R305B080016) awarded to UCLA by the Institute of Education Sciences of the US Department of Education. The views expressed in this paper are those of the authors alone and do no reflect the views/policies of the funding agencies or grantees.
References
- U.S. Census Bureau [Internet]. Language use and English-speaking ability. : 2000; October 2003. WashingtonDC: U.S. Census Bureau. date unknown, p. 11. Available from: http://www.census.gov/prod/2003pubs/c2kbr-29.pdf [cited 27 January 2010].
- U.S. Department of Health & Human Services [Internet]. Limited English proficiency (LEP). WashingtonDC: U.S. Department of Health & Human Services. [date unknown]; [about 2 screens]. Available from: http://www.hhs.gov/ocr/civilrights/resources/specialtopics/lep/ [cited 24 February 2010].
- U.S. Census Bureau. 2006–2008 American community survey 3-year estimates data set [Internet]. , Los Angeles County, CA selected social characteristics in the USA: 2006–2008. WashingtonDC: U.S. Census Bureau. [date unknown]; [about 6 screens]. Available from: http://factfinder.census.gov/servlet/ADPTable?_bm = y&-geo_id = 05000US06037&-qr_name = ACS_2008_3YR_G00_DP3YR2&-ds_name = ACS_2008_3YR_G00_&-_lang = en&-redoLog = false&-_sse = on [cited 19 January 2010].
- Office of Minority Health [Internet]. National standards for culturally and linguistically appropriate services in health care final report. ; 2000. WashingtonDC: U.S. Department of Health and Human Services. [modified 18 April 2008], p. 139. Available from: http://www.omhrc.gov/assets/pdf/checked/finalreport.pdf [cited 27 January 2010].
- Roter DL, Hall JA. Studies of doctor–patient interaction. Annu Rev Public Health. 1989; 10: 163–80.
- Institute of Medicine, Board on Health Sciences Policy., Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. In: Smedley BD, Stith AY, Nelson AR Unequal treatment: confronting racial and ethnic disparities in health care. WashingtonDC: The National Academies Press, 2003, p. 79.
- Flores G. The impact of medical interpreter services on the quality of health care: a systematic review. Med Care Res Rev. 2005; 62: 255–99.
- Dysart-Gale D. Communication models, professionalization, and the work of medical interpreters. Health Commun. 2005; 17: 91–103.
- Rivadeneyra R, Elderkin-Thompson V, Silver RC, Waitzkin H. Patient centeredness in medical encounters requiring an interpreter. Am J Med. 2000; 108: 470–4.
- Baker DW, Hayes R, Fortier JP. Interpreter use and satisfaction with interpersonal aspects of care for Spanish-speaking patients. Med Care. 1998; 36: 1461–70.
- Flores G, Laws MB, Mayo SJ, Zuckerman B, Abreu M, Medina L, et al.. Errors in medical interpretation and their potential clinical consequences in pediatric encounters. Pediatrics. 2003; 111: 6–14.
- Washington DL, Bowles J, Saha S, Horowitz CF, Moody-Ayers S, Brown AF, et al.. Transforming clinical practice to eliminate racial-ethnic disparities in healthcare. J Gen Intern Med. 2008; 23: 685–91.
- Betancourt JR. Cross-cultural medical education: conceptual approaches and frameworks for evaluation. Acad Med. 2003; 78: 560–9.
- Lie D, Boker J, Dow E, Murata P, Encinas J, Gutierrez D, et al.. Attributes of effective community preceptors for pre-clerkship medical students. Med Teach. 2009; 31: 251–9.
- Karliner LS, Perez-Stable EJ, Gildengorin G. The language divide: the importance of training in the use of interpreters for outpatient practice. J Gen Intern Med. 2004; 19: 175–83.
- Lie D, Boker J, Bereknyei S, Ahearn S, Fesko C, Lenahan P. Validating measures of third year medical students’ use of interpreters by standardized patients and faculty observers. J Gen Intern Med. 2007; 22: 336–40.
- Wiener ES, Rivera MI. Bridging language barriers: how to work with an interpreter. Clin Pediatr Emerg Med. 2004; 5: 93–101.
- American Association of Medical Colleges [Internet]. Guidelines for use of medical interpreter services. WashingtonDC: American Association of Medical Colleges, c1995–2010, p. 2. Available from: http://www.aamc.org/students/medstudents/interpreter_guide.pdf [cited 13 October 2009].