Abstract
Background
Physicians’ tolerance of uncertainty (TU) is a trait potentially associated with desirable outcomes, and emerging evidence suggests it may change over time. Past studies of TU, however, have been cross-sectional and have not measured tolerance of the different, specific types of uncertainty that physicians confront. We addressed these limitations in a longitudinal exploratory study of medical students.
Methods
At the end of medical school (Doctor of Medicine degree) Years 1 and 4, a cohort of 26 students at a US medical school completed measures assessing tolerance of different types of uncertainty: 1) complexity (uncertainty arising from features of information that make it difficult to comprehend); 2) risk (uncertainty arising from the indeterminacy of future outcomes); and 3) ambiguity (uncertainty arising from limitations in the reliability, credibility, or adequacy of information). Change in uncertainty-specific TU was assessed using paired t-tests.
Results
Between Years 1 and 4, there was a significant decrease in tolerance of ambiguity (t=3.22, p=0.004), but no change in students’ tolerance of complexity or risk.
Conclusions
Tolerance of ambiguity – but not other types of uncertainty – decreases during medical school, suggesting that TU is a multidimensional, partially mutable state. Future studies should measure tolerance of different uncertainties and examine how TU might be improved.
Physicians’ tolerance of uncertainty (TU) has become a matter of growing interest among medical educators. Emerging research suggests that TU varies among medical trainees and physicians and that greater TU is associated with various outcomes including greater comfort dealing with grief, loss, and death; reduced fear of medical error and malpractice, and reduced propensity to order diagnostic tests (Citation1, Citation2). The desirability of such outcomes raises the question of whether TU is a fixed – as opposed to a mutable – characteristic that ‘can be taught and nurtured’ (Citation1). Past studies of TU among medical trainees, however, have yielded conflicting answers to this question. Some have shown a positive relationship between TU and higher levels of medical education (Citation3–Citation5), suggesting that TU changes over time, while other studies have shown no relationship (Citation6, Citation7).
These studies, however, have been limited by their cross-sectional design as well as important conceptual and measurement problems. Most studies have not distinguished between the specific types of uncertainty that physicians confront – and that constitute the putative objects of their tolerance – but instead have treated uncertainty as a monolithic phenomenon (Citation1). Past studies have correspondingly employed various measures of TU that focus on physicians’ responses to uncertainty in general, for example, emotional ‘stress from uncertainty’, ‘reluctance to disclose uncertainty to patients’ (Citation8, Citation9), and ‘preference for highly structured training environs’ (Citation5).
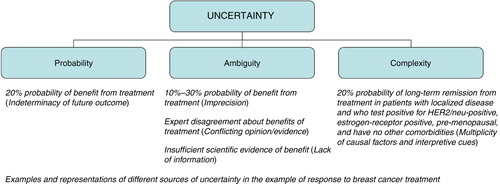
Yet uncertainty represents a multidimensional phenomenon consisting of the conscious awareness of ignorance arising from distinct sources: probability, ambiguity, and complexity () (Citation10). Probability, or ‘risk’, refers to the indeterminacy of future outcomes; ambiguity – a construct from the decision theory literature – refers to limitations in the reliability, credibility, or adequacy of information (Citation11); whereas complexity refers to features of information that make it difficult to comprehend. Behavioral research has shown that uncertainties arising from these different sources have unique effects and are associated with varying levels of tolerance among individuals (Citation10, Citation12–Citation15).
Fig. 1. Sources of uncertainty in health care. Adapted from Han et al. (Citation10).
However, most past studies of TU have not distinguished these uncertainties, and indeed have used the terms ‘uncertainty’ and ‘ambiguity’ interchangeably (Citation1). Only two studies have attempted to explicitly measure tolerance of different types of uncertainty among medical practitioners or trainees (Citation4, Citation6) (Citation8). One study measured practicing primary care physicians’ tolerance of both general uncertainty (using the Tolerance for Ambiguity (TFA) (Citation6) and Physician Reaction to Uncertainty (PRU) (Citation8) scales, both of which arguably measure tolerance of complexity) and of risk (using the Pearson Risk Attitude (PRA) scale (Citation16)) and found that both tolerance of general uncertainty (measured only by the PRU scale) and risk predicted physician resource use (Citation17). Another study assessed both primary care physicians’ tolerance of general uncertainty (using the PRU) and risk (using the PRA) and found that each predicted use of different literature-searching strategies (Citation18). These studies, however, did not measure tolerance of ambiguity (as defined in decision theory terms) and no study has assessed tolerance of different uncertainties among trainees.
This lack of conceptual and measurement specificity may account for the historically inconsistent findings regarding the development of TU among medical trainees, and the overarching objective of the current research was to explore this possibility. We undertook an exploratory study designed to longitudinally measure medical students’ specific tolerance of risk, ambiguity, and complexity. Our goal was to obtain proof-of-principle evidence on whether students’ tolerance of different types of uncertainty change over time, justifying a multidimensional approach to measuring – and potentially intervening upon – this attribute.
Methods
Study population and design
The study population consisted of the ‘Maine Track’ (MT) cohort (Class of 2014) of Tufts University School of Medicine: approximately 36/200 students in each class who are interested in rural health care and receive most clinical training at Maine rather than Boston hospitals. Survey measures, described below, were administered to MT students at the end of both Year 1 (2011) and Year 4 (2014) of medical school.
Measures
Three uncertainty-specific TU measures were completed by the cohort (). Tolerance for Ambiguity (TFA) is a seven-item measure designed to assess tolerance of general uncertainty in life, although its items focus primarily on uncertainty arising from complexity (Citation6). The scale has acceptable reliability (α=0.75), and higher tolerance of ambiguity has been shown to predict medical students’ specialty choice and physician interest in ordering a genetic test of unknown clinical utility (Citation6).
Table 1 Uncertainty tolerance measures used in the current studya
The Pearson Risk Attitude (PRA) scale is a six-item measure of TU arising from probability or risk. The PRA scale has acceptable reliability (α=0.71), and lower risk tolerance among emergency room physicians has been shown to be associated with higher rates of admission for patients with acute chest pain (Citation16).
The Ambiguity Aversion in Medicine (AA-Med) scale is a six-item measure of aversion to ambiguity (Citation19), conceptualized specifically in decision theory terms, as uncertainty regarding the reliability, credibility, or adequacy of risk information. The scale has acceptable reliability (α=0.73), and higher ambiguity aversion has been shown to predict lower interest among laypersons in a hypothetical ambiguous cancer screening test, and pessimistic appraisals of the benefits and harms of cancer screening interventions (Citation19–Citation21). Originally designed for laypersons, the scale was adapted for the current study by omitting a single item, ‘Conflicting expert opinions about a medical test or treatment would lower my trust in the experts’.
Data analyses
Descriptive analyses were conducted and Cronbach's alpha was calculated to evaluate measure reliability at both time points. Associations between TU measures were evaluated using Pearson's correlations, and change in TU assessed by each measure was evaluated using paired (matched) t-tests. As a nonparametric sensitivity analysis given the study's small sample size, change in TU was also evaluated using the Wilcoxon signed ranks test.
Results
Thirty-two students completed the Year 1 measures, and 26 (79%) completed the Year 4 measures. The cohort was 50% male, 92% Caucasian, with a mean age of 24 years at Year 1, mean Medical College Admissions Test score of 32.03 and mean college grade point average of 3.54.
Scores on the PRA, TFA, and AA-Med scales were normally distributed. There was a significant correlation between Year 1 and Year 4 scores for the PRA, but not for the TFA and AA-Med scales (). There were moderate-sized correlations between Year 4 PRA and TFA scale scores and between Year 1 TFA and AA-Med scale scores, but no other significant correlations, suggesting the scales measure distinct constructs. Scale reliability was acceptable (α≥0.70) for all scales but were relatively low for the AA-Med scale administered during Year 4 (α=0.59) ().
Table 2 Pearson correlations between different uncertainty tolerance measures
Table 3 Change in uncertainty tolerance scores between medical school years 1 and 4
No temporal differences in either tolerance of complexity (TFA scores) or tolerance of risk (PRA scores) were noted (). However, there were significant differences in ambiguity aversion (AA-Med scores). AA-Med scores were significantly lower at Year 4 than Year 1, indicating a temporal decrease in ambiguity aversion. Nonparametric analyses yielded the same pattern of results, demonstrating a significant temporal difference in AA-Med scores only (Z=2.80, p=0.005).
Discussion
The current study – to our knowledge, the first to explore TU among medical students both longitudinally and using multiple uncertainty-specific measures – demonstrated a significant temporal decrease in students’ aversion to ambiguity but no change in their tolerance of either risk or complexity. These findings are clearly preliminary given the study's small sample size; however, they have important implications.
The overarching implication is that TU is not a monolithic, static trait but a multifaceted, dynamic state (Citation10), and that aversion to – or conversely, tolerance of – ambiguity is a distinguishable TU subtype that is more malleable than tolerance of either complexity or risk. More research is needed to confirm these findings, since our study may have had insufficient power to detect change in all TU subtypes. However, our findings are consistent with past cross-sectional studies (Citation6, Citation7), as well as emerging evidence on the evolution of medical trainees’ beliefs about the nature of knowledge. Medical school is a time in which students are exposed, often for the first time, to the ambiguity pertaining to medical tests and treatments, and this exposure may promote more sophisticated epistemological beliefs and greater tolerance of this ambiguity (Citation4, Citation22). In particular, specific aspects of the medical school curriculum – for example, training in evidence-based medicine and critical appraisal of the medical literature – may heighten students’ awareness of the insufficient and conflicting scientific evidence underlying much of medical practice, and the need to accept these limitations. In contrast, the medical school curriculum per se does not aim to promote tolerance of risk or complexity. These TU subtypes, furthermore, are not specific to medicine and may be more fully developed – and resistant to change – by the time students reach medical school.
More research is needed to test these and alternative explanations of our findings and to address several study limitations. Our study was conducted at a single institution among a small cohort of students whose interest in rural health care may have influenced their baseline level and subsequent development of TU. The study assessed TU at only two time points using only three specific TU measures. Additional longitudinal studies – using larger, multiinstitution samples and multiple measures of TU subtypes – are needed to confirm our findings. Further research is also needed to examine how other unmeasured characteristics, including students’ medical knowledge and skills, might influence TU.
Despite these limitations, our study provides seminal proof-of-principle evidence that tolerance of ambiguity – an important subtype of TU unmeasured in previous studies – changes during medical education. This finding has practical implications for researchers and educators. It raises the need to understand and measure TU in an uncertainty-specific manner. It suggests that tolerance of ambiguity indeed ‘can be taught and nurtured’ (Citation1) and calls for further work to develop deliberative approaches to this task and to assess the outcomes of greater ambiguity tolerance for physicians and patients (Citation1, Citation23). Our study endorses the value of such efforts.
Conflict of interest and funding
The authors have no relevant conflicts of interest to declare. The study was funded by an Innovations in Education Grant Award from Tufts University School of Medicine.
Acknowledgements
The authors thank the Maine Track students of the Class of 2014, Tufts University School of Medicine, for their voluntary participation in the study.
References
- Geller G . Tolerance for ambiguity: an ethics-based criterion for medical student selection. Acad Med. 2013; 88: 581–4.
- Luther VP , Crandall SJ . Commentary: ambiguity and uncertainty: neglected elements of medical education curricula?. Acad Med. 2011; 86: 799–800.
- DeForge BR , Sobal J . Intolerance of ambiguity among family practice residents. Fam Med. 1991; 23: 466–8. [PubMed Abstract].
- Hancock J , Roberts M , Monrouxe L , Mattick K . Medical student and junior doctors’ tolerance of ambiguity: development of a new scale. Adv Health Sci Educ Theor Pract. 2015; 20: 113–30.
- Merrill JM , Laux LF , Lorimor R , Thornby JI , Vallbona C . Uncertainties and ambiguities: measuring how medical students cope. Med Educ. 1994; 28: 316–22.
- Geller G , Faden RR , Levine DM . Tolerance for ambiguity among medical students: implications for their selection, training and practice. Soc Sci Med. 1990; 31: 619–24.
- Weissenstein A , Ligges S , Brouwer B , Marschall B , Friederichs H . Measuring the ambiguity tolerance of medical students: a cross-sectional study from the first to sixth academic years. BMC Fam Pract. 2014; 15: 6.
- Gerrity MS , DeVellis RF , Earp JA . Physicians’ reactions to uncertainty in patient care. A new measure and new insights. Med Care. 1990; 28: 724–36. [PubMed Abstract].
- Gerrity MS , White KP , DeVellis RF , Dittus RS . Physicians’ reactions to uncertainty: refining the constructs and scales. Motiv Emot. 1995; 19: 175–91.
- Han PK , Klein WM , Arora NK . Varieties of uncertainty in health care: a conceptual taxonomy. Med Decis Making. 2011; 31: 828–38.
- Ellsberg D . Risk, ambiguity, and the savage axioms. Q J Econ. 1961; 75: 643–69.
- Camerer C , Weber M . Recent developments in modeling preferences: uncertainty and ambiguity. J Risk Uncertainty. 1992; 5: 325–70.
- Weber EU , Blais A-R , Betz NE . A domain-specific risk-attitude scale: measuring risk perceptions and risk behaviors. J Behav Decis Making. 2002; 15: 263–90.
- Hamilton JG , Hutson SP , Moser RP , Kobrin SC , Frohnmayer AE , Alter BP , etal. Sources of uncertainty and their association with medical decision making: exploring mechanisms in fanconi anemia. Ann Behav Med. 2013; 46: 204–16.
- Sonsino D , Mandelbaum M . On preference for flexibility and complexity aversion: experimental evidence. Theor Decis. 2001; 51: 197–216.
- Pearson SD , Goldman L , Orav EJ , Guadagnoli E , Garcia TB , Johnson PA , etal. Triage decisions for emergency department patients with chest pain: do physicians’ risk attitudes make the difference?. J Gen Intern Med. 1995; 10: 557–64.
- Allison JJ , Kiefe CI , Cook EF , Gerrity MS , Orav EJ , Centor R . The association of physician attitudes about uncertainty and risk taking with resource use in a Medicare HMO. Med Decis Making. 1998; 18: 320–9.
- McKibbon KA , Fridsma DB , Crowley RS . How primary care physicians’ attitudes toward risk and uncertainty affect their use of electronic information resources. J Med Libr Assoc. 2007; 95: 138–46, e49–50.
- Han PK , Reeve BB , Moser RP , Klein WM . Aversion to ambiguity regarding medical tests and treatments: measurement, prevalence, and relationship to sociodemographic factors. J Health Commun. 2009; 14: 556–72.
- Han PK , Williams AE , Haskins A , Gutheil C , Lucas FL , Klein WM , etal. Individual differences in aversion to ambiguity regarding medical tests and treatments: association with cancer screening cognitions. Cancer Epidemiol Biomarkers Prev. 2014; 23: 2916–23.
- Yeh VM , Schnur JB , Margolies L , Montgomery GH . Dense breast tissue notification: impact on women's perceived risk, anxiety, and intentions for future breast cancer screening. J Am Coll Radiol. 2015; 12: 261–6.
- Knight LV , Mattick K . ‘When I first came here, I thought medicine was black and white’: making sense of medical students’ ways of knowing. Soc Sci Med. 2006; 63: 1084–96.
- Hancock J , Mattick K . Increasing students’ tolerance of ambiguity: the need for caution. Acad Med. 2012; 87: 834; author reply 835.
