Abstract
Background
Over time, Residency Match dynamics fluctuate with some specialties experiencing increases in medical student popularity. Academic departments with limited resources must devise methods for coping with increased demand for their specialty. Students perceive traditional programs on Match mechanics as inadequate. Subsequently, faculty are confronted with demands for more personal attention from more students.
Objectives
We developed a strategy for providing specialty-specific residency match advising to large numbers of students.
Methods
The ‘speed-advising’ session (SAS) was developed to address the common questions and concerns that medical students pose during the Match process and to provide advisees with a breadth of faculty perspectives. Two SASs were offered over a 2-week period. After the sessions, students and faculty were surveyed regarding their experience.
Results
Twenty-six students pursued our specialty in the 2015 Match (26 of 234, 11.1%). Twenty-three (89%) participated in the SAS. Seventy-four percent of students (17 of 23) and all faculty completed the post-session survey. Students found the SAS to be informative, helpful and an efficient use of time. Common discussion topics included: career goals, to which programs and how many to apply, and how academic record impacts their likelihood of matching in our specialty. Students would have preferred more time with each faculty; however, most (77%) conceded that their questions were adequately answered. Faculty-favored speed advising over traditional advising (86%), primarily due to estimated time savings of 7.3 h per faculty member.
Conclusions
In preparing students for the Match, specialty-specific speed advising offers an efficient supplement to traditional advising.
The transition from medical school to residency is a challenging and anxiety-provoking process for medical students. In a very short period of time, students are required to evaluate the strength of their candidacy and select both a specialty that matches their professional interests and a residency program that will most benefit their career. Medical schools provide guidance and support to students throughout medical school (Citation1). However, as students begin to identify their specialty choice, they seek direct guidance and support from physicians in their specialty of interest.
Large-group advising meetings are commonly used to provide general and logistic information to medical students about the National Residency Match Program (NRMP) Match process and how to use the Electronic Residency Application Service (ERAS®). These types of informational meetings are most effectively delivered at the third year of medical school when students are beginning the specialty selection process and preparing their applications. Once their choice is made, however, students prefer to meet individually with faculty from their chosen specialty to seek advice and establish relationships.
Fourth-year students feel the need to know more details about the career path they have chosen. They seek advice about the logistics of applying for their specialty of interest. Specifically, they want to know how to: formulate their application, write their personal statement and prepare for interviews (Citation2). Additionally, they seek feedback on their academic record and guidance on which programs they should apply for, whether they should do away-electives, and how many applications they should generate. Furthermore, medical students seek advice from various faculty based on familiarity, educational role or status, and the faculty members own personal background.
Although literature on advising medical students regarding career or specialty selection is prevalent (Citation1, Citation3) little has been published about career advising for medical students, once their specialty choice has been established (Citation2). Effective post career–identification counseling of students during the Residency Match process requires knowledge of specialty-specific nuances such as: information about the competitiveness of specific training programs of interest, the strength of the student's application, and whether there is a match between the two (Citation4–Citation8). Therefore, medical educators from the specialty of choice play a larger role in helping medical students navigate the application and interview process.
The numbers of students interested in any given specialty fluctuate from year-to-year, and when interest is high, there are increases in demand for faculty time to meet and advise medical students specifically about their specialty. Students will often request meetings with more than one faculty member to compare and contrast the advice they receive. There is also a perception that they need to meet with residency program faculty, particularly if they are interested in matching at their home institution.
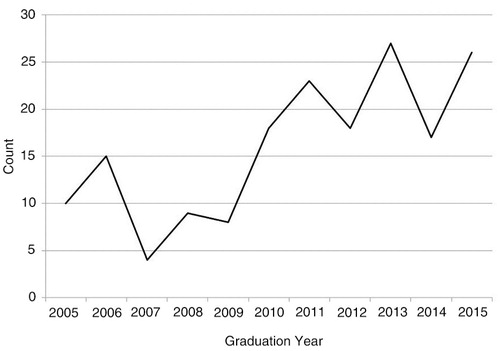
Over the past several years, our department has experienced a substantial increase in interest of our specialty and in our residency program (see ). This increase has resulted in increased demands for faculty time to meet and advise medical students.
Fig. 1. Number of medical school graduates matching in emergency medicine by graduation year at The Ohio State University College of Medicine.
The goal of this project was to devise an effective and efficient alternative for advising medical students who had already selected emergency medicine as their specialty choice. After consideration of the needs of these medical students, we designed and implemented ‘speed-advising’ sessions (SASs) for students pursuing residency in emergency medicine.
Methods
We recruited all fourth-year medical students who expressed interest in our specialty, emergency medicine to participate in the SAS. We also recruited the emergency medicine faculty whose appointments aligned with administrative roles in medical student or residency programs within the EM department. Faculty were asked to participate on a voluntary basis.
Two 2-h SASs were scheduled and offered 1 week apart during August, 2014. Student advisees were asked to complete a questionnaire in advance of the SAS that detailed their academic record, extracurricular activities, career goals, and residency program preferences. In addition, they were asked to list two or three specific questions that they hoped to have answered during the SAS. Faculty were provided with completed student questionnaires in advance of the SAS.
During the SAS, each student advisee met with up to seven EM education faculty members in succession for8-min intervals. To facilitate quick rotation and minimize time between meetings, we used proximal private offices. At the conclusion of the SASs, students and faculty completed an anonymous survey regarding this advising format.
Both students and faculty were asked whether student's questions were answered, whether there was sufficient time allotted to adequately cover student's questions, and whether they thought the SAS was efficient and informative. Both were also asked about their comfort discussing personal questions during the session, and whether they thought the process was fair and objective. Students were asked whether meeting with multiple faculty members was desirable and faculty were asked whether they prefer this method of advising to traditional methods. Both students and faculty were asked to identify the topics of discussion covered during the SAS. And finally, both students and faculty were asked open-ended questions about what they felt were the strengths and weaknesses of the speed-advising format. Descriptive statistics were tabulated using IBM-SPSS for Windows, Version 22.0 (Citation9). IRB exemption was granted.
Results
Of 26 students pursuing EM, 23 (89%) participated in the SAS. Of the eight faculty participants, six participated in both sessions, and two participated in one session. The post-session survey was completed by 74% of the student participants (17 of 23) and 100% of the faculty (all eight members). Students met with an average of 6.25 faculty and reported that over half were new to them. Faculty also reported no prior interaction with about 60% of the advisees.
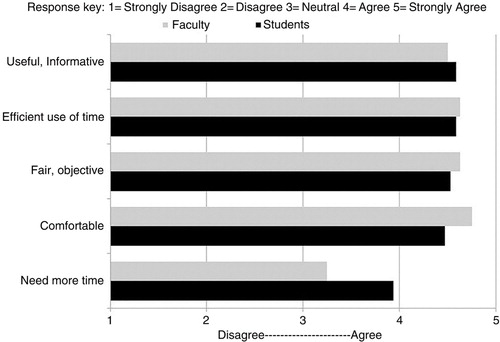
All students and faculty found the SAS to be informative and an efficient use of time (see and ). Almost all faculty and students found the SAS format to be fair and objective (100 and 94%) and were comfortable discussing personal questions (100 and 88%). Students desired longer time intervals with each faculty (71%), but 77% felt their questions were answered adequately. Most faculty members (75%) thought students had all of their questions answered, and few felt the need for longer time intervals with each student (37.5%). Faculty overwhelmingly preferred the speed-advising meeting format to the traditional advising format. Medical students were unanimous in their opinion that meeting multiple faculty in this manner was helpful.
Table 1 Post-program survey responses from 8 faculty members and 17 medical student advisees regarding speed-advising sessions
The most common discussion topics identified by both faculty and students included: to which programs and how many to apply. More than half the faculty said that application blemishes or problems were a common topic, while only one student agreed. Students also reported discussing: likelihood of matching in EM, standardized letters of evaluation, grades, United States Medical Licensing Examination (USMLE) scores, and career goals less frequently than did faculty (). The least common discussion topic identified by both faculty and students was non-clinical or extracurricular activities.
Table 2 Number (and percentage) of question topics that arose during speed-advising sessions as reported by 8 faculty members and 15 medical students
Faculty comments centered around ‘time’ as the best feature of the SAS format. They liked the efficiency and the opportunity to meet more students. Student comments centered around the value of meeting with multiple faculty as the best feature of the SAS format because they valued obtaining a wider range of opinions.
The faculty suggested that to improve the session, each faculty should be assigned specific topics to discuss with every student they met so that redundancy was eliminated. Students suggested that they needed more time with each faculty member. Some felt that meeting with seven faculty members was too many and that more time with fewer faculty would be preferred.
Discussion
Student experience
Students found the SAS to be informative and efficient. They valued advice from multiple faculty and felt their questions were adequately answered, despite a desire for more time with each faculty. Salkowitz maintains that there is both analytic and anecdotal evidence showing the value in trying to explain the attitudes of individuals and groups according to their generational outlook (Citation10). Millennial learners are generally defined as students born from the early 1980s to the early 2000s. This represents the majority of current senior medical students seeking advice about residency training programs. Some characteristics of this generation are the need for speed and innovation and an expectation of others’ investment in their careers (Citation11). The SAS addresses both of these needs for this generation of learners. Further studies may identify what students would consider an optimal time interval with each faculty member (i.e., a few more minutes vs. longer meetings approaching the traditional advising format).
Most strikingly, SAS broadened the students’ advising network by interacting with many new faculty members (students met with an average of 3.7 unfamiliar faculty). Many institutions use single advisor systems, employing either the program director or the clerkship director in this role (Citation6). This can, however, create an inherent internal conflict of the program director in the process of advising. A study by Miller in 2004 demonstrated less confidence in the student when the advisor sat on the residency selection committee (Citation7). If a dual advisor system is instead employed (program director and medical student advisor), studies have shown low levels of congruity of opinions between these two groups (Citation8). Broadening and diversifying the pool of advisors might help to address both of these issues.
Faculty experience
Faculty advisors overwhelmingly preferred SAS to traditional advisor meetings. Programs have become larger over the past decades, placing more responsibility of managing higher volumes of students on program directors. This is compounded by students seeking the opinions of multiple faculty, including assistant or associate program directors, medical student or clerkship directors, core education faculty, advisors, etc. Faculty identified significant time savings that are multiplied depending on the number of students requesting individual advising meetings. By our estimates the SAS required 253 min (11 min per student including 3-min pre-session form review and the 8-min meeting) vs. traditional advising which would have required 690 min (30 min per student). Several faculty suggested that each faculty advisor should be assigned certain topics from those delineated in in order to ensure comprehensive coverage and avoidance of redundancy.
Limitations
This study took place in a single department in a single academic center with limited sample size. Furthermore, the effect of SAS on long-term outcomes over time has yet to be evaluated. All students who participated in the SAS during this match cycle, however, successfully matched to a residency position in our specialty, emergency medicine or emergency medicine–internal medicine program.
Conclusions
Although optimal structure and time allotment should continue to be explored, speed-advising sessions allow students to have efficient interaction with multiple advisors while addressing individual concerns about matching in residency. This is a novel advising approach that we believe should be generalizable to other medical specialties and institutions.
Authors' contributions
Jillian McGrath originated the concept of the project and administered the speed-advising session. Jillian McGrath, David Way, Sarah Greenberger, Daniel Bachman, Diane Gorgas, and Nicholas Kman conducted literature reviews, formulated the evaluation instruments, prepared the faculty, and assembled the medical student profiles for the speed-advising sessions. David Way and Jason Bischof provided statistics support, data analysis, interpretation, and data management. All authors contributed to the drafting of the manuscript, critical revisions of the article, and approved the final manuscript for publication.
Disclaimer
The study was reviewed and determined to be exempt by our Human Subjects Institutional Review Board.
Conflict of interest and funding
The authors declare that they have no competing interests or financial disclosures. The authors report no external funding source for this study.
Acknowledgements
The authors would like to acknowledge Daniel R. Martin, MD, Maxwell Hill, MD, and the medical students from The Ohio State University College of Medicine for their participation in the speed-advising sessions and support of this project.
References
- Navarro AM, Taylor AD, Pokorny AP. Three innovative curricula for addressing medical students’ career development. Acad Med. 2011; 86: 72–6. [PubMed Abstract].
- Englander R, Carraccio C, Zalneraitis E, Sarkin R, Morgenstern B. Guiding medical students through the match: perspectives from recent graduates. Pediatrics. 2003; 112: 502–5. [PubMed Abstract].
- Sweeney KR, Fritz RA, Rodgers SM. Careers in medicine at Vanderbilt University School of Medicine: an innovative approach to specialty exploration and selection. Acad Med. 2012; 87: 942–8. [PubMed Abstract].
- Aagaard EM, Julian K, Dedier J, Soloman I, Tillisch J, Pérez-Stable EJ. Factors affecting medical students’ selection of an internal medicine residency program. J Natl Med Assoc. 2005; 97: 1264–70. [PubMed Abstract] [PubMed CentralFull Text].
- DeSantis M, Marco CA. Emergency medicine residency selection: factors influencing candidate decisions. Acad Emerg Med. 2005; 12: 559–61. [PubMed Abstract].
- Rogers RL, Wald DA, Lin M, Zun LS, Christopher T, Manthey DE. Expectations of an emergency medicine clerkship director. Acad Emerg Med. 2011; 18: 513–18. [PubMed Abstract].
- Miller JB, Koehn NN, Schaad DC, Crittenden RA, Oriol NE. The departmental advisor's effect on medical students’ confidence when the advisor evaluates or recruits for their own program during the match. Teach Learn Med. 2004; 16: 290–5. [PubMed Abstract].
- Crossman SH, Gary JS, Flores SK, Bradner MK, Sabo RT. Residency faculty opinions about medical student advising: a national survey. Fam Med. 2015; 47: 134–7. [PubMed Abstract].
- IBM Corp. Released 2013. IBM – SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM.
- Salkowitz R. Generation blend: managing across the technology age gap. 2008; Hoboken, NJ: Wiley.
- McNeill RJJr. Adapting Teaching to the Millennial Generation: a case study of a Blended/Hybrid course. 28 July 2011. International CHRIE Conference-Refereed Track, Paper 3. [cited 26 March 2015] Available from: (Archived by WebCite® at http://www.webcitation.org/6fK6tVoVJ).