Abstract
Research has commonly examined eating disorders (EDs) predominantly in female groups. However, males are a large minority of people with EDs. In view of this, the present paper aimed to investigate and review the experience of treatment and recovery for males with an ED. We carried out a systematic search for qualitative articles focusing on the experiences of treatment and found only four papers which met inclusion criteria. Key themes identified across studies were 1) delays in seeking treatment, 2) clinical features distinctive to males such as drive for muscularity, 3) feminine and other aspects of treatment services, and 4) lack of consensus in views about relevance of sex in treatment. More studies are needed to explore male pathways through treatment and both impediments, but also facilitators, of successful engagement in and response to treatment.
Males represent a substantive minority of people with an eating disorder (ED) particularly with binge eating disorder (Citation1, Citation2), and ED behaviors such as purging and severe dieting may be increasing at a faster rate in males than in females (Citation3). However, the perception of EDs as a predominately female problem likely contributes to the relative neglect of males in research studies and also deficits in understanding these disorders in males (Citation4), including less community sympathy in young men and women (Citation5).
Research is limited and sometimes conflicting regarding similarities and differences in etiology and clinical presentation of EDs in males compared to females. There is sparse evidence regarding genetic predisposition. Strober et al. (Citation6) have reported a similar familial aggregation in males, compared to females with anorexia nervosa, which does not support a differing genetic risk, at least for males with anorexia nervosa. Homosexuality may be a risk factor for disordered eating in men (Citation7, Citation8), but findings are complex and not consistent (Citation9). Meyer et al. (Citation10) have suggested that femininity traits act as specific risk factors for EDs in homosexual men and women, whereas masculinity in homosexual subjects of both sexes acts as a protective factor. A meta-analysis (Citation11) of studies in males found masculinity to be negatively associated with eating pathology and body dissatisfaction and femininity to be negatively related to muscle dissatisfaction in heterosexual but not in homosexual men.
With regards to clinical features, Nunez-Navarro et al. (Citation12) found a different pattern of ED behaviors (a higher frequency of vomiting episodes but less laxative abuse), less thinness preoccupation, and lower levels of general psychopathology as well as harm avoidance, reward dependence, and cooperativeness in 60 male and 60 female ED patients and compared to healthy controls. A review of more recent publications (Citation13) also supports males having lower levels of clinical symptoms, in addition to consistently higher body weight and overweight prior to and during the ED, but males did not differ from females in frequency of ED behaviors.
A recent study of 334 males’ experiences of treatment of their ED in a residential center found that whilst there were many similarities with treatment for females, there were distinctive aspects of the program that were important for males. These included addressing excessive exercise, body image concerns with muscularity, sexuality, and sexual identity. Weltzin et al. also emphasized the importance of ‘male-only’ group therapy and approaches in the program in allowing the expression of appropriate emotions that may thereby be ‘identified as strength rather than weakness’ (Citation14).
In contrast to these quantitative studies, Bezance and Holliday (Citation15) identified 11 qualitative studies of adolescents’ experiences that included only one paper with a male participant (Citation16). In this paper, the young man reported feeling unsupported as a male by some of the young women with anorexia nervosa on the unit he had been referred to. He attributed this to his desire to be more muscular, whereas they wanted to be thinner. Lamb et al. (Citation17) also carried out a systematic search for qualitative articles focusing on the experiences of eight exemplar groups with exceptional problems in access to care, including adolescents with EDs. As in Bezance and Holliday, they identified no papers with a representative sample of males, and only the same solitary paper with one male participant (Citation16). We have identified a qualitative study (Citation18) where 2 of the 17 participants recovered from bulimia nervosa were male, one of whom described that through becoming involved in self-help groups he was able to give up living according to expectations of perfection and needing to compare himself to other people.
Like other areas of ED research, qualitative studies of treatment experiences have thus focused largely on females, and to our knowledge, no systematic review of such studies in males with EDs has been published. Therefore our aims were to conduct such a systematic review with critical appraisal of studies, and if possible, a synthesis of themes from included papers. The review focused on treatment experiences in papers published since 1980. This was in order to reflect contemporary treatment experience as during this time there have been significant developments particularly in treatment of bulimia nervosa and binge ED (Citation19).
Methods
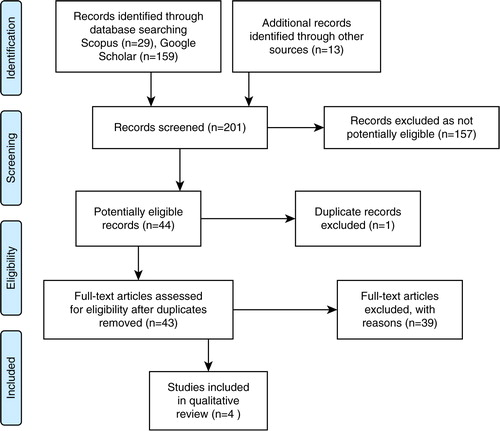
A systematic search of the literature was conducted using the following databases: Scopus (PubMed) and Google Scholar (for grey literature). The keywords in SCOPUS search were: (men or males) and (EDs or anorexia or bulimia) and (qualitative research) and (treatment experience) and PUBYEAR > 1979, and in Google Scholar were: (men or males) and (EDs or anorexia or bulimia) and (qualitative research) and (treatment experience) since 2010.
Studies identified were then individually evaluated and selected if they met the following inclusion criteria: peer reviewed article; published post-1980; participants had an ED according to current diagnostic schemes (DSM or ICD (Citation20, Citation21)); and the study addressed recovery or treatment experiences, included a majority of males and distinguished male-only data, and used a qualitative study methodology. Studies were excluded if they were not published in English and were not a study of treatment experience.
Included studies were assessed for quality by both authors based on the RATS (Citation22) and Critical Appraisal Skills Programme (CASP) criteria (Citation23) namely: 1) relevance, where the research question was explicit and linked to the existing knowledge base, 2) methods were described and justified, 3) there was transparency in regards to selection, recruitment, data collection, role of researchers/investigators, and ethics, and 4) there was rigor of analysis and reporting.
In synthesizing the evidence from relevant included papers we followed the method described in Shaw (Citation24), that is, both authors read and reread the papers separately, together constructed a table of themes as reported in the primary paper (first-order constructs), together translated studies by compiling second order constructs and a comparison of concepts from studies into one another, and then presented findings as a series of themes supported by quotes from the original papers.
Results
The search resulted in 201 papers of which 43 were potentially eligible and were read in full. Four (Citation25–(Citation28)) were determined to be eligible (). Studies (Citation4, Citation14) (Citation17, Citation18) (Citation29–Citation61)) were excluded because they were all or predominantly female participants (n=20); participants did not have a diagnosis of ED and/or it was not a study of treatment experience (n=11); and the study did not use qualitative methods (n=8). Details of potentially eligible excluded studies are found in .
Table 1. Excluded studies identified in the literature search
The four studies included in the review are described in . All had less than 10 male participants and one included participants who were representatives of health care organizations and health care professionals, and used a written survey, not interviews, to collect data (Citation25). All but one was of adults and in the fourth study the age group was unclear (Citation28). In one (Citation25) study the, methods were not reported in detail and the quality was therefore unclear. Only two studies had a primary focus of males’ experiences of treatment (Citation26, Citation27). Themes related to treatment experiences as reported in the four included papers are summarized in .
Table 2. Characteristics of included papers
Table 3. Themes related to the experience of ED treatment as reported in the primary papers
Themes resulting from translation across studies are summarized in . The first were several issues that give an understanding of delays and impediments in seeking treatment. Many participants described shame and/or stigma of having an ED as an important impediment to seeking help as in the following quotes (note only Ref. 27, provided identity pseudonyms):
It took over 10 years for me to do it … I think I was just a bit ashamed on the admitting side. [‘Ed’ from (27, p. 179)]
As a bloke I didn't like seeking help because it made me feel weak. [Participant from (28, p. 4)]
… I didn't tell her … it would be seen as a sign of weakness. [‘Ed’ from (27 p. 181)]
May be ‘… very embarrassed’. [Organisational representative from (26, p. 602)]
‘It can feel like an admission of being less than male’ ‘having a female condition’ and consequent self-stigma or there being ‘something further wrong’ ‘weak and incapable’ ‘less than male’. [Participants from (25, p. 432)]
Table 4. Translation of themes related to male's experiences of treatment for an eating disorder across the four primary studies
Males also reported that having an ED and/or having mental illness did not fit sociocultural perceptions of maleness or masculinity:
Mental disorders are not very masculine as illnesses go. [Participant from (28, p.4)]
I felt ‘I'm the only guy in the world this has happened to’. [‘Henry’ from (27, p. 180)]
Stigma in eating disorders being seen as ‘female issues’. [Practitioner from (26, p. 599)]
May perceive they have a female illness. [Organisational representative from (26, p. 602)]
Many males were ambivalent toward the ED, perceiving positive aspects of it which reduced motivation to seek help:
Because I used to be really big … people used to stare at me. So I don't really want to go back to that. [‘Greg’ from (27, p. 182)]
It was a sense of control … it just made me happy. [‘Greg’ from (27, p. 181)]
Part of the thing I really value about being underweight is that it suppresses my sexuality. [‘Frank’ from (27, p. 181)]
… Because I … wasn't fat … people wanted to get to know me. [‘Ed’ from (27, p. 181)]
There was also commonly a deficit of knowledge about EDs both in themselves and in others, and a fear of subsequent rejection through a lack of understanding or health literacy:
I'd been given all this stuff to read … from that point on I was quite keen to get it sorted out. [‘Henry’ from (27, p. 180)]
I have not sought treatment … I never thought I was sick enough … as I was never drastically underweight. [Participant from (26, p. 599)]
I was afraid of another doctor telling me I wasn't eating disordered after I tried so hard to come to terms with it. [Participant from (26, p. 599)]
Lack of recognition that eating disorders affect men. [Practitioner from (26, p. 599)]
The second aspect to emerge was that, whilst there may be clinical features in common with females, there are also distinct features of EDs in men. The first differences were around body image concerns and muscularity:
I'm not very muscular. [Participant from (28, p. 4)]
A man has connotation of big, strong, muscly … I'm a straight guy, but a somewhat feminine straight guy. [Participant from (26, p. 597)]
Appreciation of exploration of multiple definitions of masculinity aided recovery. [Practitioner report of client feedback from (26, p. 599–600)]
… Particularly those who body-build or exercise excessively. [Practitioner from (26, p. 600)]
… issue of Body Dysmorphic Disorder expresses itself through men ‘seeing’ thin … [but] … often being quite large and muscled. [Practitioner from (26, p. 602)]
it's about being fit, it's not about being skinny. [Participant from (25, p.431)]
There were also views that in some way an ED could be more likely in homosexual males compared to heterosexual males:
That's why I think women and gay men are quite similar in eating disorders, and in image …. [‘Anthony’ from (27, p.182)]
The only other clinical feature mentioned was the suppression of sexual function:
Difficulty achieving erection. [Participant from (26, p. 602)]
Several issues related to the lack of appreciation of male issues in services, the female character of services (from community and primary care to specialized services) and how it felt to be a minority in services:
All the books are directed at women. [‘Henry’ from (27, p. 180)]
[As the only male] you become aware of people holding back or you are purposely excluded, or people saying maybe it's best if you're not in this group. [‘Bill’ from (27, p. 183)]
If we had more male friendly health systems more men might talk about eating issues. [Practitioner from (26, p. 601)]
The groups I'd be sitting in on … body image things, they really didn't bear any relation to … the issues that I had … because we're women we're expected to be slim. [‘Bill’ from (27, p. 183)]
In male only groups’ men … might not feel as ashamed or less masculine. [Participant from (Citation25)]
[I] tend to include small talk about cars and speak more pitched at a masculine level. [Practitioner from (26, p. 602)]
[importance of being] … open to differences between men and women's experiences. [Practitioner from (26, p. 603)]
Treatment was perceived as often too short and professionals lacked time to listen:
Had I found it more difficult to put on weight I'd have been there for longer and would have had more therapy which I didn't really get at all. [‘Bill’ from (27, p. 182)]
It was also experienced by one participant as being controlling and a threat to self:
I didn't like being pushed around. [Participant from (25, p. 432)]
A final theme was that there was often a lack of consensus regarding the presence, relevance, or importance of sex issues:
I think this pretty much sex-excluding as a disorder. The reason why you get there are probably slightly different but in the end all roads lead to Rome. [Bill from (27, p. 182)]
I would feel most comfortable being treated by a woman. [Participant from (26, p. 602)]
I am aware it is usually considered that men are more likely to suffer from reverse eating patterns, but this has not been my experience. [Participant from (26, p. 602)]
Keep approach very similar … as for women. [Practitioner from (26, p. 603)]
Discussion
The present research is, to our knowledge, the first systematic review of qualitative studies exploring the treatment experiences of males with EDs. We found only four studies and of these only two focused on treatment experience. The two (Citation26, Citation27), however, had a clearly reported phenomenological qualitative method based on interviews. Studies were also small, only one (Citation25) reported triangulation, and none reported reaching saturation of data. Notwithstanding the limitations of the studies, some themes emerged across between two and four studies. These were most often relevant to an understanding of the barriers to help-seeking with less about processes once treatment engagement had occurred.
As in studies of women with EDs, stigma and shame were noted barriers to help-seeking. Poor ED health literacy or understanding of the nature and treatment of EDs in males with the ED as well as health professionals, and a positive regard for features of an ED that help control weight, have also been reported in studies of women with EDs (Citation62–(Citation64)). Such barriers are, however, likely compounded in males through the perception of EDs as a feminine problem and by implication males with an ED are less masculine (Citation65) and there is less sympathy and understanding of health care need from males toward people with ED (Citation5).
Homosexuality did emerge in the synthesis as a theme, somewhat negating epidemiologic evidence (Citation9). However, as other studies suggest (Citation10), the relationships of homosexuality in males to ED features such as body dissatisfaction may be indirect or moderated by other psychological constructs such as degrees of femininity/masculinity. Research in males has pointed to the different body image concerns they may have, and some have argued for muscle dysmorphic disorder to be a variant of an ED in males (Citation66). This view was supported by the finding of body image concerns around muscularity across three studies. Few other clinical features of males with EDs were described in the present study. In particular, there was an absence of themes around differing ED behaviors and obesity or weight disorder. The single report of sexual dysfunction is a reminder that males also have endocrine effects of EDs, the impact of which adds to poor quality of life of males with EDs (Citation2).
Some males, as has been reported in studies of females, perceived their treatment experience as being unsupportive with professionals lacking time and the experience being a threat to self and a sense of control (Citation63, Citation64). The males in this review also drew attention to a lack of care providers’ appreciation of male issues. This supports the view of Weltzin et al. (Citation14) that tailored services should to be provided for males for optimal outcomes. However, others in this review saw much in common for males with EDs with females and were positive about treatment from female practitioners. There seemed to be a lack of consensus with regards to the need for male-only services. Although this was found in only two of the studies, these were the two studies that focused on exploring treatment issues (Citation26, Citation27).
The strengths of this review were the broad inclusion criteria of all forms of an ED and the use of two reviewers in trial identification and data extraction. Limitations were the search of only one academic database; however, SCOPUS is broad based and includes PubMed papers as well as those from the social sciences. We decided to focus on post-1980 studies in order to provide a contemporary context for understanding the treatment experience of males, but this did mean we are unable to discuss how their experience may have changed over a longer time period. In addition, our review cannot comment on experiences of children or younger adolescents as no study addressed these groups. Finally, we did not contact authors to clarify methodologies where information was lacking in the published report and we included qualitative studies with disparate methodologies.
Conclusions
The present review identified only four small qualitative studies of males who have had treatment for an ED. The findings support studies in females which have investigated the delays and barriers to treatment seeking, such as stigma and poor health literacy. The findings also support studies which have argued for an appreciation of different body image concerns, i.e. a drive for muscularity being present in males, and heightened stigma of an ED in males as EDs are perceived a ‘female’ problem. Larger studies focusing on treatment experiences are needed to explore and expand on the issues of the similarities and differences in clinical features and thereby treatment needs, the role and nature of male-only services versus mixed-sex services, and what features of services may better engage and motivate males in therapy. Studies are also needed to explore the treatment experience across ED diagnostic groups.
Conflict of interest and funding
The authors have no conflicts to declare and the study is unfunded.
References
- Hudson JI, Hiripi E, Pope HG Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007; 61: 348–58.
- Mitchison D, Mond J, Slewa-Younan S, Hay P. Sex differences in health related quality of life impairment associated with eating disorder behaviors: a general population study. Int J Eat Disord. 2013; 46: 375–80.
- Mitchison D, Hay P, Slewa-Younan S, Mond J. The changing demographic profile of eating disorder behaviors in the community. BMC Public Health. 2014; 14: 943.
- Striegel RH, Bedrosian R, Wang C, Schwartz S. Why men should be included in research in binge eating: results from a comparison of psychosocial impairment in men and women. Int J Eat Disord. 2012; 45: 233–40.
- Mond JM, Arrighi A. Gender differences in perceptions of the severity and prevalence of eating disorders. Early Interv Psychiatry. 2011; 5: 41–49.
- Strober M, Freeman R, Lampert C, Diamond J, Kaye W. Males with anorexia nervosa: a controlled study of eating disorders in first-degree relatives. Int J Eat Disord. 2001; 29: 263–9.
- Russell CJ, Keel PK. Homosexuality as a specific risk factor for eating disorders in men. Int J Eat Disord. 2002; 31: 300–6.
- Matthews-Ewald MR, Zullig KJ, Ward RM. Sexual orientation and disordered eating behaviors among self-identified male and female college students. Eat Behav. 2014; 15: 441–4.
- Mitchison DM, Hay PJ. The epidemiology of eating disorders: genetic, environmental, and societal factors. Clin Epidemiol. 2014; 6: 89–97.
- Meyer C, Blissett J, Oldfield C. Sexual orientation and eating psychopathology: the role of masculinity and femininity. Int J Eat Disord. 2001; 29: 314–18.
- Blashill AJ. Gender roles, eating pathology, and body dissatisfaction in men: a meta-analysis. Body Image. 2011; 8: 1–11.
- Nunez-Navarro A, Aguera Z, Krug I, Murcia SM, Sanchez I, Araguz N. Do men with eating disorders differ from women in clinics, psychopathology and personality?. Eur Eat Disorders Rev. 2012; 20: 23–31.
- Raevuori A, Keski-Rahkonen A, Hoek WA. A review of eating disorders in males. Curr Opin Psychiatry. 2014; 27: 426–30.
- Weltzin TE, Carlson TC, Fitzpatrick ME, Kennington B, Bean P, Jefferies C. Treatment issues and outcomes for males with eating disorders. Eat Disord. 2012; 20: 444–59.
- Bezance J, Holliday J. Adolescents with anorexia nervosa have their say: a review of qualitative studies on treatment and recovery from anorexia nervosa. Eur Eat Disorders Rev. 2013; 21 : 352–60.
- Tierney S. The individual within a condition: a qualitative study of young people's reflections on being treated for anorexia nervosa. J Am Psychiatr Nurses Assoc. 2008; 13: 368.
- Lamb J, Bower P, Rogers A, Dowrick C, Gask L. Access to mental health in primary care: a qualitative meta-synthesis of the evidence from the experience of people from ‘hard to reach’ groups. Health. 2012; 16: 76–104.
- Nakamura H. Overcoming bulimia nervosa: a qualitative study of recovery in Japan. Proceedings. 2012; 17: 101–09.
- Agras WS. Agras WS. Introduction and overview. The Oxford handbook of eating disorders. 2010; New York, NY: Oxford University Press. 1–6.
- APA. Diagnostic and statistical manual of mental disorders. 2013; Washington, DC: American Psychiatric Publishing. fifth Ed.
- WHO. International statistical classification of diseases and related health problems 10th revision. 1992; Geneva: World Health Organization.
- Clark JP. Godlee F, Jefferson T. How to peer review a qualitative manuscript. Peer review in health sciences. 2003; London: BMJ Books. 219–35. Second Ed.
- CASP. Qualitative research checklist. Critical Appraisal Skills Program. 2013. Downloaded 21 July 2014. http://www.casp-uk.net/ [cited 21 July 2014]..
- Shaw RL. Harper D, Thompson AR. Identifying and synthesising qualitative literature. Qualitative research in mental health and psychotherapy: a guide for students and practitioners. 2012; John Wiley. 9–22.
- De Beer ZD, Wren B. Fox JRE, Goss KP. Wiley series in clinical psychology: eating and its disorders. Somerset. 2012; NJ: John Wiley. 427–41.
- Dearden A, Mulgrew KE. Service provision for men with eating issues in Australia: an analysis of organisations’ practitioners’ and men’ experiences. Aust Soc Work. 2013; 66: 590–606.
- Robinson KJ, Mountford VA, Sperlinger DJ. Being men with eating disorders: perspectives of male eating disorder service users. J Health Psychol. 2012; 18: 176–86.
- Drummond MJN. Men, body image, and eating disorders. Int J Mens Health. 2002; 1: 89–103.
- Aardoom JJ, Alexandra ED, Spinhoven P, Van Furth EF. Treating eating disorders over the internet: a systematic review and future research directions. Int J Eat Disord. 2013; 46: 539–52.
- Adams G, Turner H, Bucks R. The experience of body dissatisfaction in men. Body Image. 2005; 2 : 271–83.
- Algars M, Alanko K, Santtilla P, Sandnabba NK. Disordered eating and gender identity disorder: a qualitative study. Eat Disord. 2012; 20 : 300–11.
- Bjork T, Wallin K, Pettersen G. Male experiences of life after recovery from an eating disorder. Eat Disord. 2012; 20: 460–68.
- Clement S, Schauman O, Graham T, Maggioni F, Lacko SE, Bezborodovs N. What is the impact of mental health-related stigma on help seeking? A systematic review of quantitative and qualitative studies. Psychol Med. 2014; 26 : 1–17.
- Cossrow NHF, Jeffery RW, McGuire MT. Understanding weight stigmatization: a focus group study. J Nutr Educ. 2001; 33: 208–214.
- Couchman G, McMahon G, Kelly A, Ponsford J. A new kind of normal: qualitative accounts of multifamily group therapy for acquired brain injury. Neuropsychol Rehab. 2014; 24 (6): 809–32.
- Dinos S, Stevens S, Serfaty M, Weich S, King M. Stigma: the feelings and experiences of 46 people with mental illness: qualitative study. Br J Psychiatry. 2004; 184: 176–81.
- Graham G, Walton M. Investigating the use of CD-Rom CBT for bulimia nervosa and binge eating disorder in an NHS adult outpatient eating disorder services. Behav Cogn Psychother. 2011; 39: 443–56.
- Green C. Gender differences in treating adolescents with eating disorders. Master of Social Work Clinical Research Papers, Paper 186. 2013. http://sophia.stkate.edu/msw_papers/186..
- Hargreaves DA, Tiggemann M. ‘Body image is for girls’ a qualitative study of boys body image. J Health Psychol. 2006; 11: 567–76.
- Hay PJ, Cho K. A qualitative exploration on the process of recovery from personal written accounts of people with anorexia nervosa. Women Health. 2013; 53: 730–40.
- Higginson S, Mansell W. What is the mechanism of psychological change? A qualitative analysis of 6 individuals who experienced personal change and recovery. Psychol Psychothe Theor Res Pract. 2008; 81 : 309–28.
- Juarascio A, Shaw J, Forman E, Timko CA, Herbert J, Butryn M. Acceptance and commitment therapy as a novel treatment for eating disorders: an initial test of efficacy and mediation. Behav Modif. 2013; 37: 459–89.
- Karlsson GP, Nevonen L. Anorexia nervosa: treatment expectations: a qualitative study. J Multidiscp Health Care. 2012; 5: 169–77.
- Lawrence D. Irish male anorexia: prevalence, presentation and treatment, an investigation. Thesis Dublin Business School online 2011. http://hdl.handle.net/10788/197 [cited 21 July 2014].
- Linville D, Brown T. Eating disorders and social support: perspectives of recovered individuals. Eat Disord. 2012; 20: 216–31.
- Long S, Wallis D, Leung N, Meyer C. ‘All eyes are on you’: anorexia nervosa patient perspective of in-patient mealtimes. J Health Psychol. 2011; 17: 419–28.
- Malson H, Finn M, Treasure J, Clarke S, Anderson G. Constructing ‘The Eating Disordered Patient'1: a discourse analysis of accounts of treatment experiences. J Community Appl Soc Psychol. 2004; 14: 473–89.
- Malson H, Bailey L, Clarke S, Treasure J, Anderson G, Kohn M. Un/imaginable future selves: a discourse analysis of in patients’ talk about recovery from an eating disorder. Eur Eat Disord Rev. 2011; 19: 25–36.
- Morgan JF, Arcelus J. Body image in gay and straight men: a qualitative study. Eur Eat Disord Rev. 2009; 17: 435–43.
- Pettersen G, Rosenvinge JH, Wynn R. Eating disorders and psychoeducation – patient's experiences of healing processes. Scand J Caring Sci. 2011; 25: 12–18.
- Pretorius N, Rowlands L, Ringwood S, Schmidt U. Young people's perceptions of and reasons for assessing web based cognitive behaviourial intervention for Bulimia Nervosa. Eur Eat Disord Rev. 2010; 18: 197–206.
- Rahkonen AK, Tozzi F. The process of recovery in eating disorder sufferer's own words: an internet based study. Int J Eat Disord. 2005; 37: S80–6.
- Rance NM, Clarke V, Moller NP. ‘If I see somebody … I'll immediately scope them out’: anorexia nervosa clients perceptions of their therapists body. Eat Disord. 2013; 22: 111–20.
- Reid M, Burr J, Williams S, Hammersley R. Eating disorders patients’ views on their disorders and on an outpatient service: a qualitative study. J Health Psychol. 2008; 13: 956–60.
- Rosenvinge JH, Klusmeier AK. Treatment for eating disorders from a patient satisfaction perspective: a Norwegian replication of a British study. Eur Eat Disord Rev. 2000; 8: 293–300.
- Sabel AL, Rosen E, Mehler PS. Severe anorexia nervosa in males: clinical presentations and medical treatment. Eat Disord. 2014; 2: 209–20.
- Stice E, Martie CN, Durant S. Risk factors for onset of eating disorders: evidence of multiple risk pathways from an 8-year old prospective study. Behav Res Ther. 2011; 49: 622–27.
- Timulak L, Buckroyd J, Klimas J, Creaner M, Wellsted D, Bunn F. Helpful and unhelpful aspects of eating disorders treatment involving psychological therapy. 2013; London: British Association of Counselling and Psychotherapy.
- Trepal HC, Boie I, Kress VE. A relational cultural approach to working with clients with eating disorder. J Couns Dev. 2012; 90: 346–56.
- Vromans LP, Schweitzer RD. Narrative therapy for adults with major depressive disorder: improved symptom and interpersonal outcomes. Psychother Res. 2010; 21: 4–15.
- Warren CS, Schafer KJ, Crowley MEJ, Olivardia R. Treatment providers with a personal history of eating pathology: a qualitative examination of common experiences. Eat Disord. 2013; 21: 295–309.
- Hepworth N, Paxton S. Pathways to helpseeking in bulimia nervosa and binge eating problems: a concept mapping approach. Int J Eat Disord. 2007; 40: 493–504.
- Evans EJ, Hay PJ, Mond JM, Paxton SJ, Quirk F, Rodgers B. Barriers to help-seeking in young women with eating disorders: a qualitative exploration in a longitudinal community survey. Eat Disord. 2011; 19: 270–85.
- Rich E. Anorexic dis(connection): managing anorexia as an illness and an identity. Sociol Health Illn. 2006; 28: 284–305.
- Griffiths S, Mond JM, Murray SB, Touyz S. Young peoples’ stigmatizing attitudes and beliefs about anorexia nervosa and muscle dysmorphia. Int J Eat Disord. 2014; 47: 189–95.
- Murray SB, Rieger E, Karlov L, Touyz SW. An investigation of the transdiagnostic model of eating disorders in the context of muscle dysmorphia. Eur Eat Disorders Rev. 2013; 21: 160–4.