Abstract
The majority of patients with acute myeloid leukemia (AML) reach complete remission after high-dose chemotherapy. Still, half of these patients experience a relapse due to presence of minimal residual disease (MRD). Here we discuss the poor prognostic role of class II-associated invariant chain peptide (CLIP) expression on residual leukemic cells.
Presence of aberrant markers on leukemic cells, termed the leukemia associated phenotype, facilitates follow-up and early detection of minimal residual disease (MRD) to predict relapse of AML.Citation1 A frequency of >0.1% residual leukemic cells is associated with a very high relapse risk (hazard ratio 2.97), while absence or a very low frequency of residual cells (<0.1%) is a good prognostic feature. This high predictive value of MRD analysis recently resulted in the initiation of a multicenter clinical trial in which presence or absence of MRD combined with an intermediate or good cytogenetic risk-profile is directive for proceeding to allogeneic or autologous stem cell transplantation (SCT), respectively (www.hovon.nl). However, presence of MRD is not exclusively predictive for a relapse. The central role of tumor immune surveillance in the development of AMLCitation2,3 may explain why some MRD-positive patients do not experience a relapse, and other patients with a low frequency of MRD do experience an early relapse. Various immune escape mechanisms have been reported. For instance, enhanced expression of co-inhibitory molecules such as PD-L1 on leukemic cells impairs recognition by cytotoxic CD8+ T cells. Interestingly, antibodies against co-inhibitory receptor CTLA-4 show promising results as immunotherapeutic agents in solid tumors.Citation4 For AML, the first multicenter clinical trial with CTLA-4 blocking agent Ipilimumab has been started (clinicaltrial.gov: NCT01757639).
Unlike most other solid tumors, the majority of leukemias are positive for HLA-DR. Their potential to activate CD4+ T helper cells is directly linked to the expression of the class II-associated invariant chain peptide (CLIP). CLIP is a small self-peptide and cleavage product of the invariant chain (i.e. CD74) that resides in the HLA-II antigen binding groove. For efficient HLA-II antigen presentation, CLIP is exchanged for an antigenic peptide after which the HLA-II/peptide complex is transported to the plasma membrane. We have previously shown that leukemic cells expressing CLIP are poorly recognized by CD4+ T helper cells.Citation5 Alternatively, we revealed that CLIP can also be presented by HLA class I, implicating that insufficient recognition by cytotoxic CD8+ T cells might play a role as well.Citation6 Probably, genes regulating the antigen presentation pathway are impaired in leukemic cells, leading to increased expression of CLIP.
Irrespective of its regulation and function, CLIP expression on de novo leukemic cells is a predictor of poor clinical outcome in AML.Citation5 In our recent study, we assessed whether CLIP on residual leukemic cells could add to the prognostic value of MRD frequency for relapse risk.Citation7 The current cut-off for MRD positivity is 0.1%. However, for MRD-negative acute leukemias, up to 40% of patients experience a relapse, most likely due to outgrowth of low frequent residual cells.Citation1 In a cohort of 50 AML patients, we analyzed CLIP expression on residual leukemic cells during follow-up using multiparameter flow cytometry. In 32 patients, 0.01-0.1% of residual cells were detected and considered as MRDlow. For these cases, we found that high expression of CLIP (>35%) on residual leukemic cells (16/32 patients) was predictive for a shortened relapse-free survival. In total, 10/12 cases experiencing a relapse were CLIP positive (specificity 83%) and 14/20 cases who remained in remission were negative for CLIP (sensitivity 70%).
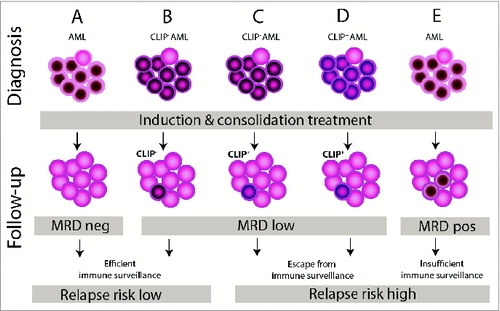
In this paper, we demonstrate that CLIP is a predictive marker on residual leukemic cells for relapse risk in AML, especially in patients considered as MRDlow (). Also other markers might be of importance to determine which AML patient is at high risk for developing a relapse. Especially those markers that give the leukemic cell a functional benefit in escaping immune surveillance, such as PD-L1, but also IDO,Citation8 may be of high importance in predicting AML relapse. In our view, extensive phenotypic evaluation of functional immune markers on residual leukemic cells will result in better prediction which AML patients are likely to benefit from additional treatment options for relapse prevention. It will also provide the basis for development of targeted and personalized immunotherapies in AML. This is directly related to the clinical potential of defining the immune contexture for solid tumors, as recently described.Citation9
Figure 1. Proposed model for the role of CLIP on residual leukemic cells in relapse of AML. When no MRD cells are detected during follow-up of AML, there is a low probability for a relapse (A). In the situation of a low MRD percentage (<0.1%) with CLIP-negative residual leukemic cells during follow-up, the immune system is able to effectively target these cells, thereby preventing a relapse (B). For CLIP-positive residual cells, either CLIP-negative leukemic cells may gain CLIP expression during follow-up (C) or CLIP-positive leukemic cells preferentially resist high-dose chemotherapy and subsequent consolidation therapy (e.g. allogeneic stem cell transplantation; (D) resulting in escape from immune surveillance and a high relapse risk. When the frequency of MRD cells is higher than 0.1%, the immune system lacks the capacity to eliminate such high number of outgrowing residual leukemic cells (E). AML, acute myeloid leukemia; CLIP, class II-associated invariant chain peptide; MRD, minimal residual disease.
Strategies that counteract the immunosuppressive effects such as CLIP downmodulation are preferably combined with systemic immune activators, by means of e.g. dendritic cell-based vaccinations and adoptive T cell transfer. CLIP downmodulation may be achieved by using drug compounds such as HDAC and PKC inhibitors. Currently, also novel genes are being identified that regulate the HLA-II pathway and may be targeted by new drug compounds to downmodulate CLIP for improving antigen presentation efficiency.Citation10
Additional immunotherapeutic treatment should be ideally started before residual leukemic cells gain proliferative activity and escape from immune surveillance. The delicate balance between optimal recovery of the immune system after chemotherapy and the risk of relapse can be elucidated by regular follow-up for MRD. For patients with <0.1% MRD, who are considered MRDlow, additional analysis of e.g. CLIP on residual leukemic cells may further differentiate between high risk patients to find an optimal time point for consolidation immunotherapy. Finally, detection of low frequent CLIP-positive leukemic cells during follow-up may be an extra argument for proceeding to an allogeneic SCT.
In conclusion, evaluation of CLIP on residual leukemic cells as part of the standard protocols for monitoring MRD will help to predict relapse occurrence in AML. Detailed flow cytometric assessment of CLIP and additional markers contributing to immune surveillance of residual leukemic cells may not only serve as diagnostic tool, but also offer critical information for the design and timing of immunotherapeutic strategies during AML follow-up.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
References
- Terwijn M, van Putten WL, Kelder A, van der Velden VH, Brooimans RA, Pabst T, Maertens J, Boeckx N, de Greef GE, Valk PJM, et al. High prognostic impact of flow cytometric minimal residual disease detection in acute myeloid leukemia: data from the HOVON/SAKK AML 42A study. J Clin Oncol 2013; 31:3889-97; PMID: 24062400; http://dx.doi.org/10.1200/JCO.2012.45.9628
- Zitvogel L, Tesniere A, Kroemer G. Cancer despite immunosurveillance: immunoselection and immunosubversion. Nat RevImmunol 2006; 6:715-727; PMID: 16977338; http://dx.doi.org/10.1038/nri1936
- Teague RM and Kline J. Immune evasion in acute myeloid leukemia: current concepts and future directions. J Immunother Cancer 2013; 1; PMID: 24353898; http://dx.doi.org/10.1186/2051-1426-1-13
- Hodi FS, O’Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, Gonzalez R, Robert C, Schadendorf D, Hassel JC, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med 2010; 363:711-23; PMID: 20525992; http://dx.doi.org/10.1056/NEJMoa1003466
- van Luijn MM, van den Ancker W, Chamuleau ME, Zevenbergen A, Westers TM, Ossenkoppele GJ, van Ham SM, van de Loosdrecht AA. Absence of class II-associated invariant chain peptide on leukemic blasts of patients promotes activation of autologous leukemia-reactive CD4+ T cells. Cancer Res 2011; 71:2507-17; PMID: 21310823; http://dx.doi.org/10.1158/0008-5472.CAN-10-3689
- van Luijn MM, van de Loosdrecht AA, Lampen MH, van Veelen PA, Zevenbergen A, Kester MG, de Ru AH, Ossenkoppele GJ, van Hall T, van Ham SM. Promiscuous binding of invariant chain-derived CLIP peptide to distinct HLA-I molecules revealed in leukemic cells. PLoS One 2012; 7:e34649; PMID: 22563374; http://dx.doi.org/10.1371/journal.pone.0034649
- van den Ancker W, van Luijn MM, Chamuleau ME, Kelder A, Feller N, Terwijn M, Zevenbergen A, Schuurhuis GJ, Ham SM, Westers TM, et al. High class II-associated invariant chain peptide expression on residual leukemic cells is associated with increased relapse risk in acute myeloid leukemia. Leuk Res 2014; 38:691-93; PMID: 24731748; http://dx.doi.org/10.1016/j.leukres.2014.03.014
- Chamuleau ME, van de Loosdrecht AA, Hess CJ, Janssen JJ, Zevenbergen A, Delwel R, Valk PJM, Löwenberg B, Ossenkoppele GJ. High INDO (indoleamine 2,3-dioxygenase) mRNA level in blasts of acute myeloid leukemic patients predicts poor clinical outcome. Haematologica 2008; 93:1894-98; PMID: 19050070; http://dx.doi.org/10.3324/haematol.13113
- Angell H, Galon J. From the immune contexture to the Immunoscore: the role of prognostic and predictive immune markers in cancer. Curr Opin Immunol. 2013; 25:261-267; PMID: 23579076; http://dx.doi.org/10.1016/j.coi.2013.03.004
- van Kasteren SI, Overkleeft H, Ovaa H, Neefjes J. Chemical biology of antigen presentation by MHC molecules. Curr Opin Immunol 2014; 26:21-31; PMID: 24556397; http://dx.doi.org/10.1016/j.coi.2013.10.005
