Abstract
A male patient with Stage IV melanoma was treated with ipilimumab resulting in a long-lasting partial response according to RECIST criteria. However, twenty months after ipilimumab treatment, routine follow-up CT scan revealed new splenic lesions initially interpreted as indicative of progressive disease. Nevertheless, a biopsy was performed and histologic evaluation showed that the lesions did not contain malignant cells but rather constituted non-caseating epithelioid cell granulomas consistent with sarcoidosis. As the patient was asymptomatic no treatment was initiated and over the following months the splenic lesions slowly disappeared and to date the patient remains in remission.
Ipilimumab is now widely used in the treatment of melanoma patients. Our case-report illustrates that physicians should consider the possibility of ipilimumab induced visceral sarcoidosis-like reactions, mimicking metastatic lesions, developing even many months after ipilimumab treatment. Thus, biopsy of such suspicious lesions is advisable to avoid misinterpretation as disease progression and unnecessary resumption of cancer therapy.
Background
Ipilimumab (Yervoy; Bristol-Myers Squibb) is a fully humanized, monoclonal antibody directed against cytotoxic T-lymphocyte associated protein 4 (CTLA-4) and approved for the clinical treatment of metastatic melanoma. It was the first drug to show improved survival of patients with metastatic melanoma in a Phase III trialCitation1 and recent data have shown that treatment with ipilimumab can foster long-term survival.Citation2 Blockade of CTLA-4 is thought to elicit an antitumor immune response by overcoming CTLA-4 mediated T-lymphocyte suppression. Side effects of ipilimumab treatment are mainly due to autoimmune reactions. Thus, numerous immune-related adverse reactions have been reported in connection with ipilimumab treatment including colitis, hepatitis, hypophysitis, uveitis, dermatitis, pancreatitis, neuropathy and vitiligo. The past few years a small number of cases of ipilimumab-induced sarcoidosis-like reactions in lung and mediastinum have been reported.Citation3–8 Here we report a case of late sarcoidosis-like granulomatosis of the spleen in a patient previously treated with ipilimumab for metastatic melanoma.
Sarcoidosis is a multi-systemic inflammatory disease of unknown etiology characterized by the accumulation of T lymphocytes, mononuclear phagocytes, and non-caseating granulomas occurring in affected organs.Citation9 The disease predominantly involves the lungs and mediastinum, but can involve virtually any organ system in the body. The physiopathology of sarcoidosis remains unclear but the presence of granulomatous inflammation is thought to result from an exaggerated cell-mediated immune response to one or more unidentified antigens in a genetically predisposed hosts. The disorder is characterized by a T helper type 1 response that is mediated primarily by the release of interleukin-2 (IL-2) and interferon γ (IFNγ). The immune reaction leads to the formation of granulomas composed of epithelioid and giant cells surrounded by a ring of fibroblasts, and CD4+ and CD8+ T lymphocytes.Citation10 There are no morphologic features of the granulomas that are specific for sarcoidosis, therefore these lesions lack definitive diagnostic hallmarks, and non-caseating granulomas may also be seen in patients with infectious disease (e.g., tuberculosis, brucellosis, histoplasmosis), environmental exposures (e.g., beryllium), autoimmune disorders (e.g., Wegener's granulomatosis), and neoplasms.Citation11
Case Report
A 44-year old man was diagnosed in 1999 with a melanoma on the left shoulder, (Breslow thickness 1.5 mm, Clarks level 4) for which he underwent local resection. Shortly prior to this, the patient had undergone radical right upper and middle lobectomy due to a carcinoid lung tumor (histologically confirmed) and was subsequently infected with hepatitis B during hospitalization. Otherwise he had no previous medical history. In 2009, the patient relapsed with multiple melanoma metastases in several organ systems including the right kidney, lungs, mediastinal and retroperitoneal lymph nodes, brain, osteolytic bone metastases and multiple intramuscular and subcutaneous metastases. The diagnosis was confirmed histopathologically in a biopsy from the right kidney. The patient received stereotactic radiation therapy for a brain metastasis in the right frontal hemisphere and in the left cerebellar hemisphere and subsequently started treatment with temozolomide 150 mg/m2 in May 2009. Due to substantial regression of the disease shortly after treatment initiation, temozolomide dose was increased to 200 mg/m2 and a complete remission of peripheral lesions was obtained after 12 months of temozolomide therapy. At that time magnetic resonance imaging (MRI) of the brain unfortunately revealed a new brain metastasis in the previously irradiated field. The patient received repeated stereotactic radiation and continued temozolomide therapy for another 5 months until progression with new metastases in the right lung and mediastinum as shown by computed tomography (CT) as well as suspected progression of the known brain metastases shown by MRI ().
Figure 1. Sarcoidoisis-like lesions occurring in melanoma cancer patient following ipilumumab therapy. Horizontal sections of the brain with melanoma metastatic tumor imaged by magnetic resonance imaging (MRI) and horizontal sections of thorax and abdomen by computed tomography (CT); red arrows indicate isolated sarcoidosis-like granulomas; yellow arrows indicate metastases in the right lung and mediastinum; green arrows indicate residual metastatic burden. Longitudinal imaging: (A) November 2010, pre-ipilimumab; (B) March 2011, after 4 courses of ipilimumab; (C) April 2011, 6 weeks after Ipilimumab; (D) August 2011, 5 months after ipilimumab; (E) November 2012, 20 months after ipilimumab and (F) December 2013, 2 y and 10 months after ipilimumab.
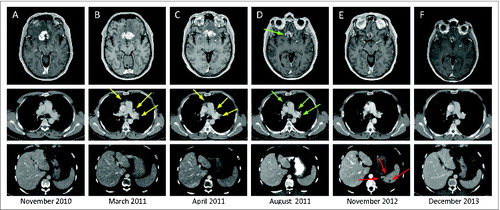
Consequently, in December 2010 the patient started treatment with ipilimumab 3 mg/kg, every 3 weeks. He tolerated all 4 courses of ipilimumab well, however, evaluation CT scans in March 2011 showed progressive disease (, yellow arrows) which was confirmed in April 2011, with new mediastinal lymph node enlargement and a new lung metastasis (, yellow arrows) whereas brain metastases were stable. Progression was presumed and the patient was referred to experimental treatment. However, this treatment was never initiated because novel imaging evaluation showed minor regression of both mediastinal lymph nodes and brain metastases and therefore an approach of watchful waiting was decided (, green arrows). In the following months the mediastinal lymph nodes regressed further and the brain metastases remained stable (imaging not shown).
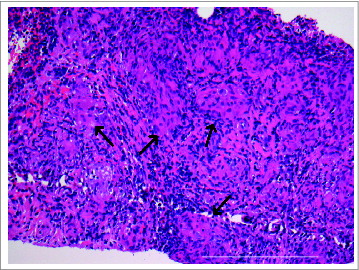
In November 2012, 20 month after ipilimumab therapy was completed, CT scan revealed multiple small (less than 1 cm in diameter), hypodense splenic nodules indicative of metastatic disease (, red arrows). There was no associated splenomegaly. The previously enlarged lymph nodes in the mediastinum were no longer measurable according to RECIST and the lesions in the brain remained stable. There were no other new lesions. Retrospectively a few small lesions in the spleen could be found on CT scans dating 6 month back, slowly increasing in size and number. Because metastases were suspected ultrasound-guided core biopsy was performed to ensure diagnosis and histologic examination showed non-caseating epithelioid cell granulomas consistent with sarcoidosis (). Immunohistochemistry showed negative reaction for the melanoma markers S-100 and melan-A, and no malignant cells were detected (data not shown). The patient had no symptoms and no treatment was administered. During the next 6 months the lesions in the spleen slowly disappeared and the latest evaluation scans in December 2013 showed complete regression of the splenic lesions () and otherwise stable disease with the cerebellar metastasis being the only visible lesion.
Figure 2. Development of splenic sarcoidosis-like lesions in melanoma patient with durable response to ipilimumab. Ultrasound guided biopsy and histological examination of the hypodense lesions in the spleen of ipilimumab treated melanoma patient showing several non-caseating epithelioid cell granulomas (black arrows) consistent with sarcoidosis (hematoxylin-eosin stain; original magnification × 20, scale bar 500 μm).
Discussion
The development of sarcoidosis in melanoma patients in general is rare, as it has been reported in only 0.6% (7/1199) of melanoma patients in a large retrospective study.Citation12 Involvement of the spleen is common in patients with sarcoidosis, but isolated splenic sarcoidosis itself is infrequent.Citation13,14 Splenic sarcoidosis is usually asymptomatic and typically manifests as homogeneous splenomegaly; however, it may present as multiple low-attenuation nodular lesions which can easily be mistaken for metastases and infections, such as tuberculosis.Citation15 The diagnosis requires needle biopsy and the exclusion of other granulomatous diseases.
To our knowledge, this is the first report of a melanoma patient developing isolated sarcoidosis-like granulomas in the spleen after treatment with ipilimumab. Six cases of ipilimumab-induced sarcoidosis-like reactions in melanoma patients have previously been reported.Citation3-8 Three patients received ipilimumab 3 mg/kg and 3 patients received ipilimumab 10 mg/kg. In all cases the lungs and mediastinum was affected and in addition 3 of the patients presented with cutaneous lesions with histopathologic features resembling sarcoidosis.Citation3,7,8 Three patients with symptoms from the respiratory system received corticosteroid treatment and in all patients the sarcoidosis-like reactions disappeared after a few months, regardless of whether or not the patient underwent treatment. This is also the first reported case of late development of sarcoidosis-like reaction more than 1½ year after last ipilimumab dose. In contrast, previously reported cases occurred during or within a few months after treatment with ipilimumab.
Because ipilimumab is now widely used as standard therapy for metastatic melanoma it is important for clinicians to be aware of the fact that sarcoidosis-like reaction could be induced at several different organ sites including the spleen and that these lesions can very easily be mistaken for melanoma metastases. Conventional FDG-PET and CT cannot distinguish between metastatic lesions and granulomatosis. Thus, confirmatory biopsy of new suspected malignant radiographic findings, for example, in the spleen of ipilimumab treated patients, is essential in order to avert incorrect diagnosis of disease progression and subsequent unnecessary initiation of the next line of therapy.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
References
- Hodi F, O’Day S, McDermott D, Weber R, Sosman J, Haanen J, Gonzalez R, Roberts C, Schadendorf D, Hassel J, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med 2010; 363:711-23; PMID:20525992; http://dx.doi.org/10.1056/NEJMoa1003466
- Prieto PA, Yang JC, Sherry RM, Hughes MS, Kammula US, White DE, Levy CL, Rosenberg SA, Phan GQ. CTLA-4 blockade with ipilimumab: long-term follow-up of 177 patients with metastatic melanoma. Clin Cancer Res 2012; 18:2039-47; PMID:22271879; http://dx.doi.org/10.1158/1078-0432.CCR-11-1823
- Eckert A, Schoeffler A, Dalle S, Phan A, Kiakouama L, Thomas L. Anti-CTLA4 monoclonal antibody induced sarcoidosis in a metastatic melanoma patient. Dermatology 2009; 218:69-70; PMID:18832811; http://dx.doi.org/10.1159/000161122
- Berthod G, Lazor R, Letovanec I, Romano E, Noirez L, Stalder J, Speiser D, Peters S, Michielin O. Pulmonary sarcoid-like granulomatosis induced by ipilimumab. J Clin Oncol 2012; 30:10-3; PMID:22547608; http://dx.doi.org/10.1200/JCO.2011.39.3298
- Vogel W, Guislain A, Kvistborg P, Schumacher T, Haanen J, Blank C. Ipilimumab-induced sarcoidosis in a patient with metastatic melanoma undergoing complete remission. J Clin Oncol 2012; 30:7-10; PMID:22124098; http://dx.doi.org/10.1200/JCO.2011.37.9693
- Wilgenhof S, Morlion V, Seghers AC, Du Four S, Vanderlinden E, Hanon S, Vandenbroucke F, Everaert H, Neyns B. Sarcoidosis in a patient with metastatic melanoma sequentially treated with anti-CTLA-4 monoclonal antibody and selective BRAF inhibitor. Anticancer Res 2012; 32:1355-9; PMID:22493370
- Reule RB, North JP. Cutaneous and pulmonary sarcoidosis-like reaction associated with ipilimumab. J Am Acad Dermatol 2013; 69:e272-3; PMID:24124863; http://dx.doi.org/10.1016/j.jaad.2013.07.028
- Tissot C, Carsin A, Freymond N, Pacheco Y, Devouassoux G. Sarcoidosis complicating anti-cytotoxic T-lymphocyte-associated antigen-4 monoclonal antibody biotherapy. Eur Respir J 2013; 41:246-7; PMID:23277525; http://dx.doi.org/10.1183/090319-36.00107912
- Baughman RP, Lower EE, du Bois RM. Sarcoidosis. Lancet 2003; 361:1111-8; PMID:12672326; http://dx.doi.org/10.1016/S0140-6736(03)12888-7
- Iannuzzi M, Fontana J. Sarcoidosis: clinical presentation, immunopathogenesis, and therapeutics. Jama 2011; 305:391-9; PMID:21266686; http://dx.doi.org/10.1001/jama.2011.10
- Rosen Y. Pathology of sarcoidosis. Semin Respir Crit Care Med 2007; 28:36-52; PMID:17330191; http://dx.doi.org/10.1055/s-2007-970332
- Seve P, Schott AM, Pavic M, Broussolle C, Gilis L, Thomas L. Sarcoidosis and melanoma: a referral center study of 1,199 cases. Dermatology 2009; 219:25-31; PMID:19365109; http://dx.doi.org/10.1159/000213245
- Zia H, Zemon H, Brody F. Laparoscopic splenectomy for isolated sarcoidosis of the spleen. J Laparoendosc Adv Surg Tech 2005; 15:160-2; PMID:15898908; http://dx.doi.org/10.1089/lap.2005.15.160
- Chen M-Y, Cai J-T, Du Q, Wang L-J. Sarcoidosis of spleen presenting with solitary thrombopenia. Eur J Intern Med 2009; 20:e12; PMID:19237065; http://dx.doi.org/10.1016/j.ejim.2007.09.022
- Mohan A, Sood R, Shariff N, Gulati MS, Gupta SD, Dutta AK. Sarcoidosis manifesting as massive splenomegaly: a rare occurrence. Am J Med Sci 2004; 328:170-2; PMID:15367876; http://dx.doi.org/10.1097/00000441-200409000-00007
