Abstract
There is growing public concern regarding assay sensitivity to HBsAg mutants in clinical diagnosis and vaccine escape. The aim of this study is to introduce a new HBsAg mutant strain. The serum samples were those of patient X at the age of 3 months and 3 years respectively, and of her mother immediately before parturition, which were used to amplify the HBsAg-coding DNA fragments by PCR. The HBsAg DNA sequences were translated into their corresponding amino acid sequences and then aligned in pubmed with nucleotide blast. The sequencing data of S coding regions shows that patient X has been infected by a new HBV variant with an A to C substitution at nt431, resulting in an Asp(GAC)to Ala(GCC) substitution at aa144 of major protein; CC to AA substitution at nt359 and nt360, resulting in an Pro(CCC) to Gln(CAA) substitution at aa120 of pre “a” epitope; A to G substitution at nt491, resulting in an Glu(GAG) to Gly(GGG) substitution at aa164 of post “a” epitope. Three new mutations (S171F, S174N and Q181R) at the antigenic epitopes of HBV presented by HLA class I molecules are found. The HBV mutant strain causes vaccine escape and occult infection.
Abbreviations:
- WBC, white blood cell count
- RBC, red blood cell count
- Hb, hemoglobin
- Plt, platelet count
- CRP, C-reactive protein
- TP, total protein
- Alb, albumin
- T-Bil, total bilirubin
- AST, aspartate aminotransferase
- ALT, alanine aminotransferase
- ALP, alkaline phosphatase
- γGTP, γ-glutamyl transferase
- LDH, lactate dehydrogenase
- UA, uric acid
- AchE, acetylcholin esterase
- TG, triglycerides
- HBsAg, hepatitis B surface antigen
- Anti-HBs, antibodies to HBsAg
- Anti-HBc, antibodies to hepatitis B core antigen
- HCV, hepatitis C virus
- anti-HA, antibody to hepatitis A
- EBV, Epstein-Barr virus
- VCA, viral capsid antigen
- EBNA, Epstein-Barr nuclear antigen
- CMV, cytomegalovirus
- EIA, enzyme immunoassay
Introduction
Hepatitis B virus (HBV) is an etiological agent of acute and chronic liver disease, including fatal fulminant hepatitis, cirrhosis and hepatocellular carcinoma, which is one of the most common human cancers and causes of death worldwide.Citation1 It has been estimated that more than 2 billion of the global population have been infected with HBV. Of these, approximately 360 million people are chronically infected, and an estimated 500,000 to 700,000 people die from complications of HBV infection each year worldwide.Citation2 Hepatitis B vaccination program has been implemented for decades and has obtained the remarkable achievements in reducing the incidence of HBV infection.Citation3,4 However, HBV has not gone away and always stay in a certain infection rate . The reason is very worthy of our thinking. In the article we introduce a new HBsAg mutant strain that genetic mutations occur in the area within and outside the `a' determinant region and the CTL epitope of HBsAg to clarify part of the possible mechanisms.
Case Report
Patient X, female, was born to a hepatitis B carriers’ mother. The patient had been immunized with HBV vaccine on a conventional 0, 1, 6 schedule: an injection of HBV vaccine was given at the time of birth, at 1 month and at 6 months of age. The serum samples used were those of patient X at the age of 3 months and 3 years respectively, and of her mother immediately before parturition.
Blood tests revealed negative results for HBsAg and positive results for HBeAg, anti-HBc and Pre-S1 in patient X’ sera at both the age of 3 months and 3 years. However, patient X’ HBV DNA is positive (6.2 × 10Citation6 ge/ml). Her mother's blood test results revealed positive for HBsAg, anti-HBe and anti-HBc and negative for HBeAg and anti-HBs. The serum samples of her mother were taken immediately before parturition. A systematic blood sample of patient X analyzed at the age of 3 years revealed normal level liver enzymes (ALT: 38 U/L [upper normal limit <50], AST: 42 U/L [upper normal limit <55], ALP: 120 U/L [<136], γGTP: 11 U/L [<50] and T-Bil: 5.8 μmol/L [<19]) associated with normal level CRP: 2 mg/L [<8] with no leukocytosis. The detailed data was shown in . No history of hepatitis A, HCV, CMV and EBV infection were found in this patient as well. The clinical features of Patient X is characterized by poor drug effect, illness bounce after the drug was stopped, e antigen turns negative difficult.
Table 1. Laboratory date of patient X at the age of 3 years
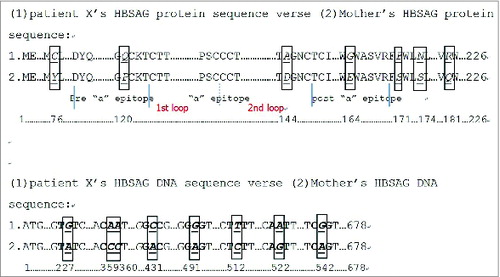
The HBsAg-coding 1.2-kb fragments were amplified by PCR from the serum samples of patient X, who had failed to achieve protection from vaccination. The sequencing data of the S coding region shows that she has been infected by a new HBV variants with an A to C substitution at nt431, resulting in an Asp(GAC) to Ala(GCC) substitution at aa144 of major protein; CC to AA substitution at nt359 and nt360, resulting in an Pro(CCC) to Gln(CAA) substitution at aa120 of pre “a” epitope; A to G substitution at nt491, resulting in an Glu(GAG) to Gly(GGG) substitution at aa164 of post “a” epitope; C to T substitution at nt512, G to A substitution at nt522, A to G substitution at nt542, A to G substitution at nt227, resulting in an Ser(TCT) to Phe(TTT) substitution at aa171, an Ser(AGT) to Asn(AAT) substitution at aa174, an Gln(CAG) to Arg(CGG) substitution at aa181, an Tyr(TAT) to Cys(TGT) substitution at aa76, respectively. The detailed data was shown in .
Figure 1. The nucleotides sequence (nt) and amino acid (aa) sequence of S gene from patient X and her mother.The nucleotides sequence and amino acid sequences of S gene from patient X at the age of 3 months and 3 years are the same. All aa122 and aa160 among them are Lys(K), the characteristic amino acids for subtype adw.Citation22
Discussion
There is no difference in the sequences of HBV variants throughout the complete S region from the blood samples of patient X collected at her 3 months and 3 years of age respectively. This indicates that this variant is stable in maintaining persistent replication in the chronic patient. Comparing with the nucleotides sequence of S coding region of HBV DNA from the mother of patient X collected immediately before parturition, patient X shows distinctly differences in nt227, nt359, nt360, nt431, nt491, nt512, nt522 and nt542. Thus, patient X and her mother appear to be infected by 2 different HBV strains. Patient X turns out to be infected by a new mutant of HBV, mainly characterized by the immune escape.
The major HBsAg is the small molecule HBsAg with 226 amino acid residues. It has 2 moderately hydrophilic regions, one at residues 30 to 79 which is internal, and another at residues 99 to 168 which is exposed on the surface of the HBsAg particle. The second region, rich in cysteines and prolines, is considered as encompassing the immunogenic epitopes determining the serotypes of various HBV strains. Among them, the ‘a’ determinant is common to all HBV strains and is presumed to be important for the protective immune response to HBV. The domain between aa124 to aa147 is the critical region for neutralizing immunogenicity of the “a” determinant. Through the analysis of the sequence, we found patient X was infected by a new HBV variants with an A to C substitution at nt431, resulting in an Asp (GAC) to Ala (GCC) substitution at aa144 of the “a” determinant. Asp is an electropositive hydrophilic amino acid, but Ala is a neutral and hydrophobic one. The exchange between Asp and Ala should lead to a drastic change in the conformation of the “a” determinant, and in antigenicity as well. We believe this is one of the reasons why HBsAg cannot be detected by detection method based on the antibody. As Tyr (TAT) to Cys (TGT) substitution at aa76 is not exposed on the surface of the HBsAg particle, so this mutation on the new immune escape mutant of HBV will not affect antigenicity of HBsAg.
The region between aa100 and aa160 is termed as the major hydrophilic region (MHR). This comprises amino acids (aa) 99–160 that encompass the group-specific “a” determinant. The region between aa118 and aa123 was identified as a hot spot for insertion by investigators. The importance of an Pro(CCC) to Gln(CAA) substitution at aa120 of pre “a” epitope is that the mutations, situated closely adjacent to the ‘a’ determinant, could change the entire immunodominant region structure and therefore weaken the antigenicity even though no mutations were found within this ‘aa124-aa147’ region. In order to demonstrate the influence of adjacent residues on the ‘a’ determinant conformation, Scientists have done a lot of research. Mutation at the position of aa120 have been found to impair the performance of HBsAg tests, either alone or combination with other substitutions and the reported mutation phenotype at the position of aa120 is P120G/S/L.Citation5-8 It is the first time to our knowledge that the mutation that Pro (CCC) to Gln (CAA) substitution at aa120 has been reported.
Upstream (between 164 and 215) of MHR region of native and or recombinant surfance proteins has different binding capcities to antibodies.Citation9-11 Hence, the classical definition of the ‘a' immunodominant region may need to be extended to require adjacent amino acids supporting its conformation. The amino acid sequence of the polymerase between aa163 and aa210 is the region that can confer resistance to some polymerase inhibitors, when mutated.Citation12 We found an Glu(GAG) to Gly(GGG) substitution at aa164 of post “a” epitope of HBV on patient X and this may has important clinical significance.
The hepatitis B virus is not directly cytopathic for the infected hepatocyte, and it is generally presumed that viral clearance and liver cell injury during viral hepatitis are due to a CTL response to HBV encoded Ag presented by HLA class I molecules.Citation13,14 Schirmbeck et al. found that in H-2b mice even small changes in amino acid residues within 2 different CTL epitopes that mimic natural variants of adw2, ayr and adr, completely eliminated the immunogenicity of each epitope.Citation13 A majority of mutations of up- and downstream of MHR in different studies were found to be potentially responsible for vaccine breakthrough and HBsAg undetectability which unpredictably were found to be located within the known CTL epitopes of surface protein.Citation15,16 Mutations that abrogate recognition of a viral epitope by class I-restricted CTL contribute to viral persistence in a subset of patients with chronic HBV infection who express a narrow repertoire of anti-HBV CTL responses. Thus, viral mutations in CTL epitopes were able to evade cellular immunity and contribute to persistency.Citation17-19 The aa 171–179 Citation20,21 and aa175–184 Citation22,23 is the antigenic epitopes of HBV presented by HLA class I molecules. In this region, we found 3 new mutations (S171F, S174N and Q181R) on HBV which infected patient X. Studies from our laboratory have revealed there is a higher frequency of mutations at the position of the HLA-restricted CTL epitope of the surface gene in patients with chronic hepatitis B, suggesting that these mutations might contribute to chronic infections. In the process of clinical treatment, these variations have significantly affected patient X’ clinical treatment effect and disease outcome which is characterized by poor drug effect, illness bounce after the drug was stopped, e antigen turns negative difficultly.
In conclusion, the mutations of the new HBsAg variant that Asp (GAC) to Ala (GCC) substitution at aa144 of the “a” determinan and Pro (CCC) to Gln (CAA) substitution at aa120 causes false negative tests of HBsAg and vaccine escape; 3 new mutations (S171F, S174N and Q181R) on HBV from the pantient X induce CTL dysfunction contributing to chronic infections.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
References
- Lee WM. Hepatitis B virus infection. N Engl J Med 1997; 337:1733-45; PMID:9392700
- Shouval D. Hepatitis B vaccines. J Hepatol 2003; 39 Suppl 1:S70-76; PMID:14708681
- Boccalini S, Pellegrino E, Tiscione E, Pesavento G, Bechini A, Levi M, Rapi S, Mercurio S, Mannelli F, Peruzzi M, et al. Sero-epidemiology of hepatitis b markers in the population of tuscany, central italy, 20 years after the implementation of universal vaccination. Hum Vaccin Immunother 2013; 9:636-41; PMID:23354158; http://dx.doi.org/10.4161/hv.23259
- Liao XY, Zhou ZZ, Wei FB, Qin HN, Ling Y, Li RC, Li YP, Nong Y, Sun KX, Li J, et al. Seroprevalence of hepatitis b and immune response to hepatitis b vaccination in chinese college students mainly from the rural areas of western china and born before hbv vaccination integrated into expanded program of immunization. Hum Vaccin Immunother 2014; 10:224-31; PMID:24018404; http://dx.doi.org/10.4161/hv.26311
- Avellon A, Echevarria JM, Weber B, Weik M, Schobel U, Willems WR, Gerlich WH. European collaborative evaluation of the Enzygnost HBsAg 6.0 assay: performance on hepatitis B virus surface antigen variants. J Med Virol 2011; 83:95-100; PMID:21108344; http://dx.doi.org/10.1002/jmv.21943
- Jeantet D, Chemin I, Mandrand B, Tran A, Zoulim F, Merle P, Trepo C, Kay A. Cloning and expression of surface antigens from occult chronic hepatitis B virus infections and their recognition by commercial detection assays. J Med Virol 2004; 73:508-15; PMID:15221893; http://dx.doi.org/10.1002/jmv.20119
- Tian Y, Xu Y, Zhang Z, Meng Z, Qin L, Lu M, Yang D. The amino Acid residues at positions 120 to 123 are crucial for the antigenicity of hepatitis B surface antigen. J Clin Microbiol 2007; 45:2971-8; PMID:17609325; http://dx.doi.org/10.1128/JCM.00508-07
- Weber B, Van der Taelem-Brule N, Berger A, Simon F, Geudin M, Ritter J. Evaluation of a new automated assay for hepatitis B surface antigen (HBsAg) detection VIDAS HBsAg Ultra. J Virol Methods 2006; 135:109-17; PMID:16567005; http://dx.doi.org/10.1016/j.jviromet.2006.02.009
- Datta S, Chatterjee S, Veer V, Chakravarty R. Molecular biology of the hepatitis B virus for clinicians. J Clin Exp Hepatol 2012; 2:353-65; http://dx.doi.org/10.1016/j.jceh.2012.10.003
- Ireland JH, O'Donnell B, Basuni AA, Kean JD, Wallace LA, Lau GK, Carman WF. Reactivity of 13 in vitro expressed hepatitis B surface antigen variants in 7 commercial diagnostic assays. Hepatology 2000; 31:1176-82; PMID:10796895; http://dx.doi.org/10.1053/he.2000.6407
- Mühlbacher A, Weber B, Bürgisser P, Eiras A, Cabrera J, Louisirirotchanakul S, Tiller FW, Kim HS, v Helden J, Bossi V, et al. Multicenter study of a new fully automated HBsAg screening assay with enhanced sensitivity for the detection of HBV mutants. Med Microbiol Immunol 2008; 197:55-64; PMID:17899185; http://dx.doi.org/10.1007/s00430-007-0059-9
- Scheiblauer H, El-Nageh M, Diaz S, Nick S, Zeichhardt H, Grunert HP, Prince A. Performance evaluation of 70 hepatitis B virus (HBV) surface antigen (HBsAg) assays from around the world by a geographically diverse panel with an array of HBV genotypes and HBsAg subtypes. Vox Sang 2010; 98:403-14; PMID:20412171; http://dx.doi.org/10.1111/j.1423-0410.2009.01272.x
- Jung MC, Diepolder HM, Pape GR. T cell recognition of hepatitis B and C viral antigens. Eur J Clin Invest 1994; 24:641-50; PMID:7531642; http://dx.doi.org/10.1111/j.1365-2362.1994.tb01055.x
- Schirmbeck R, Dikopoulos N, Kwissa M, Leithäuser F, Lamberth K, Buus S, Melber K, Reimann J. Breaking tolerance in hepatitis B surface antigen (HBsAg) transgenic mice by vaccination with cross-reactive, natural HBsAg variants. Eur J Immunol 2003; 33:3342-52; PMID:14635042; http://dx.doi.org/10.1002/eji.200324403
- Bertoletti A, Costanzo A, Chisari FV, Levrero M, Artini M, Sette A, Penna A, Giuberti T, Fiaccadori F, Ferrari C. Cytotoxic T lymphocyte response to a wild type hepatitis B virus epitope in patients chronically infected by variant viruses carrying substitutions within the epitope. J Exp Med 1994; 180:933-43; PMID:7520476; http://dx.doi.org/10.1084/jem.180.3.933
- Khedive A, Norouzi M, Ramezani F, Karimzadeh H, Alavian SM, Malekzadeh R, Montazeri G, Nejatizadeh A, Ziaee M, Abedi F, et al. Hepatitis B virus surface protein mutations clustered mainly in CTL immune epitopes in chronic carriers: results of an Iranian nationwide study. J Viral Hepat 2013; 20:494-501; PMID:23730843; http://dx.doi.org/10.1111/jvh.12045
- Bertoletti A, Sette A, Chisari FV, Penna A, Levrero M, De Carli M, Fiaccadori F, Ferrari C. Natural variants of cytotoxic epitopes are T-cell receptor antagonists for antiviral cytotoxic T cells. Nature 1994; 369:407-10; PMID:8196768; http://dx.doi.org/10.1038/369407a0
- Franzese O, Kennedy PT, Gehring AJ, Gotto J, Williams R, Maini MK, Bertoletti A. Modulation of the CD8+-T-cell response by CD4+ CD25+ regulatory T cells in patients with hepatitis B virus infection. J Virol 2005; 79:3322-8; PMID:15731226; http://dx.doi.org/10.1128/JVI.79.6.3322-3328.2005
- Zuckerman AJ. Effect of hepatitis B virus mutants on efficacy of vaccination. Lancet 2000; 355:1382-4; PMID:10791517
- Barnaba V, Franco A, Paroli M, Benvenuto R, De Petrillo G, Burgio VL, Santilio I, Balsano C, Bonavita MS, Cappelli G, et al. Selective expansion of cytotoxic T lymphocytes with a CD4+CD56+ surface phenotype and a T helper type 1 profile of cytokine secretion in the liver of patients chronically infected with Hepatitis B virus. J Immunol 1994; 152:3074-87; PMID:7511637
- Shahmoradi S, Yahyapour Y, Mahmoodi M, Alavian SM, Fazeli Z, Jazayeri SM. High prevalence of occult hepatitis B virus infection in children born to HBsAg-positive mothers despite prophylaxis with hepatitis B vaccination and HBIG. J Hepatol 2012;57:515-21; PMID:22617152; http://dx.doi.org/10.1016/j.jhep.2012.04.021
- Ducos J, Bianchi-Mondain AM, Pageaux G, Conge AM, Poncet R, Vendrell JP, Segondy M, Serre A. Hepatitis B virus (HBV)-specific in vitro antibody production by peripheral blood mononuclear cells (PBMC) after vaccination by recombinant hepatitis B surface antigen (rHBsAg). Clin Exp Immunol 1996;103:15-8; PMID:8565275; http://dx.doi.org/10.1046/j.1365-2249.1996.928621.x
- Mancini-Bourgine M, Fontaine H, Brechot C, Pol S, Michel ML. Immunogenicity of a hepatitis B DNA vaccine administered to chronic HBV carriers. Vaccine 2006;24:4482-9; PMID:16310901; http://dx.doi.org/10.1016/j.vaccine.2005.08.013
- Cha CH, Sohn YH, Ko SY, Oh HB. Subgenotype and serotype analysis of hepatitis b virus in korean chronic hepatitis b patients under treatment. Kor J Lab Med 2009; 29:53-8; PMID:19262079
