Figures & data
Table 1. List of authorized sweeteners in the European Union according to the European Food Safety Authority, with E-numbersCitation11.
Figure 1. Artificial sweeteners affect the gut microbiota and endocrine response. Artificial sweeteners from different dietary products can affect the microbial gut composition via activation of taste receptors linked to the modulation of, eating behavior, glucose tolerance and handling insulin sensitivity and inflammation. AS: artificial sweeteners; T1R2/T1R3: taste receptor type 1 member 2 and 3; HbA1C%: glycosylated hemoglobin.
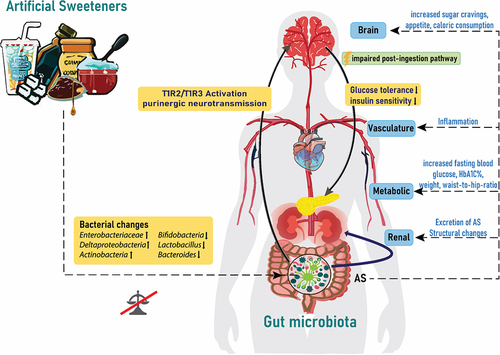
Figure 2. Simplified illustration of uremic toxins, specifically IS, PCS, TMAO and PAG and their association with increased allostatic load and early vascular aging (EVA) in the context of CKD. The diagram outlines the pathways through which these toxins contribute to the increased EVA with a focus on major impact related to vascular function and structure, such as endothelial dysfunction, calcification, cellular senescence and arterial stiffness among others. IS: Indoxyl sulfate; PCS: p-cresyl sulfate; TMAO: Trimethylamine N-oxide; PAG: Phenylacetylglutamine; CKD: chronic kidney disease; EVA: early vascular aging; RAA: renin-angiotensin-aldosterone; NO: Nitric oxide.
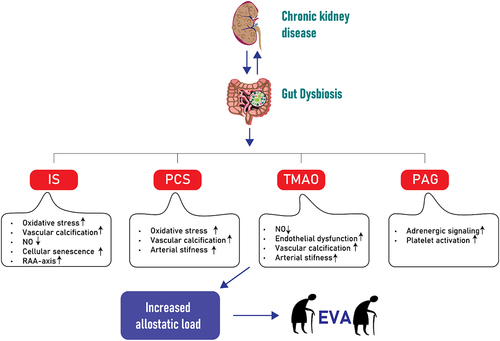
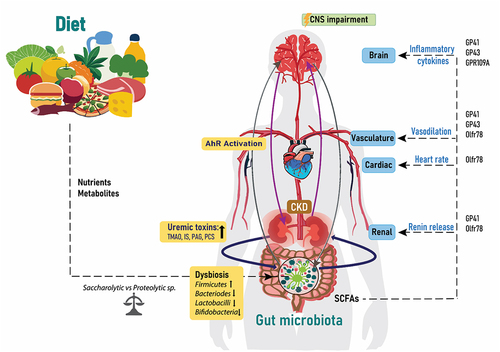
Figure 3. Diet, gut, brain and CKD. The relationship between the gut microbiota, kidney and brain is a circulatory process, which is influenced by the nutrients and metabolites from dietary choices. Increased bacterial changes lead to dysbiosis, which increases the release of uremic toxins into the circulation and activation of the AhR receptors and thereafter effects on the CNS. The amount of SCFAs from the gut microbiota influence renal renin release, heart rate and vasodilation and inflammatory cytokines through acting on the listed proteins. IS: Indoxyl sulfate; PCS: p-cresyl sulfate; TMAO: Trimethylamine N-oxide; PAG: Phenylacetylglutamine; CKD: chronic kidney disease; SCFAs: short chain fatty acids; CNS: central nervous system and AhR: aryl hydrocarbon receptor.
Data availability statement
No data is needed.23–25

