Figures & data
Table 1 Currently Available Data on Osteoporosis Serum Biomarkers and Their Applicability in the Diagnosis, Progression and Monitoring of Osteoporosis
Figure 1 Metabolic imbalance is the source of biomarkers in osteoporosis In osteoporosis, a balanced activity between osteoblasts and osteoclasts is of utmost importance. An imbalance between the bone-forming and disturbing activities on the hand of the latter results in altered bone formation and eventually osteoporosis. Bone turnover biomarkers are promising candidates to monitor these molecular changes in this microcosm. Collagen type I produced by osteoblasts is of key importance in bone integrity and homeostasis. Under proteolytic activity promoted by osteoclast derived CTSK, collagen type I is degraded into several remnants, like CTX-I, NTX, PYD, and DPD. These collagen degradation products are candidate molecules for laboratory diagnosis of osteoporosis from biological fluids (patients’ sera and urine), CTX-I being currently the most widely accepted BTM for this clinical purposes. On the other hand, procollagens and osteocalcin are key participants in bone metabolism. According to the current guidelines PINP is considered the clinical counterpart of CTX-I, as a BTM of osteoporosis. Wnt signal molecules have a cardinal role in the interplay of cellular participants in bone tissues. Osteocyte derived sclerostin and DKKs secreted by BMSCs and osteoblasts, as inhibitors of the Wnt pathways and subsequently bone formation are two nominee molecules for future perspectives. Arrows in green represent activation or secretory mechanisms. Arrows in red indicate inhibition or degradation mechanisms.
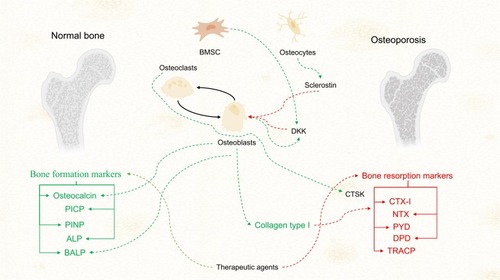
Table 2 Currently Available Evidence of Soluble Biomarkers for the Diagnosis, Staging and Monitoring of Osteoarthritis
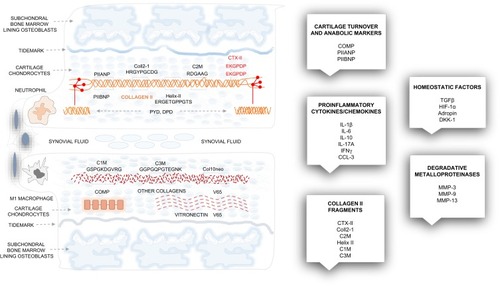
Figure 2 The basic structures of the cartilage, molecular sources and main groups of osteoarthritis biomarkers. Superficial and deep cartilage, synovial membrane and the subchondral bone marrow are all affected in osteoarthritis. Inflammatory cells invade the synovial membrane, the subchondral bone suffers intense remodeling, and the metabolic turnover of the extracellular matrix components is high. Collagen type II fragments: CTX-II, Coll2-1, Helix II, C2M are cleaved and released in the synovial fluid and the blood. Collagen I, III, vitronectin and proteoglycans are also excessively degraded, which results in the loss of matrix. The main groups of osteoarthritis biomarkers: cartilage turnover/anabolic markers, proinflammatory cytokines/chemokines, collagen II fragments, matrix metalloproteinases, and various homeostatic molecules are shown in boxes.