Figures & data
Figure 2 Escitalopram showed 5-HT transporter occupancy that outlived its plasma concentration.
Copyright © 2007, Springer-Verlag. Adapted with permission from Klein N, Sacher J, Geiss-Granadia T, et al. Higher serotonin transporter occupancy after multiple dose administration of escitalopram compared to citalopram: an [123I]ADAM SPECT study. Psychopharmacology (Berl). 2007;191(2):333–339.Citation13
![Figure 2 Escitalopram showed 5-HT transporter occupancy that outlived its plasma concentration.Copyright © 2007, Springer-Verlag. Adapted with permission from Klein N, Sacher J, Geiss-Granadia T, et al. Higher serotonin transporter occupancy after multiple dose administration of escitalopram compared to citalopram: an [123I]ADAM SPECT study. Psychopharmacology (Berl). 2007;191(2):333–339.Citation13](/cms/asset/2fa62c3a-bc1f-434f-b788-ddd986d744c7/dppa_a_22495_f0002_c.jpg)
Table 1 Comparison of changes in total MADRS scores at 8 weeks (last observation carried forward) among patients with MDD treated with escitalopram, paroxetine, or placebo
Figure 3 Changes in the cumulative non-relapse rate.
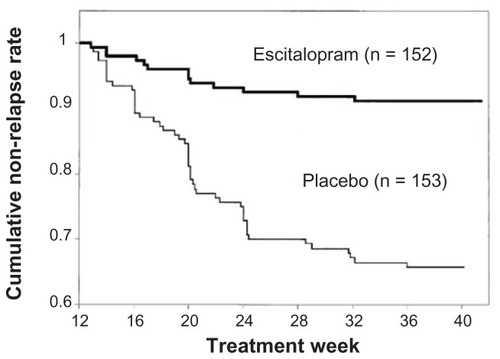
Figure 4 Discontinuation Emergent Signs and Symptoms (DESS 47) scores in the post-therapy observation period.
Copyright © 2006, Lippincott Williams & Wilkins. Adapted with permission from Baldwin DS, Cooper JA, Huusom AK, Hindmarch I. A double-blind, randomized, parallel-group, flexible-dose study to evaluate the tolerability, efficacy and effects of treatment discontinuation with escitalopram and paroxetine in patients with major depressive disorder. Int Clin Psychopharmacol. 2006;21(3):159–169.Citation25
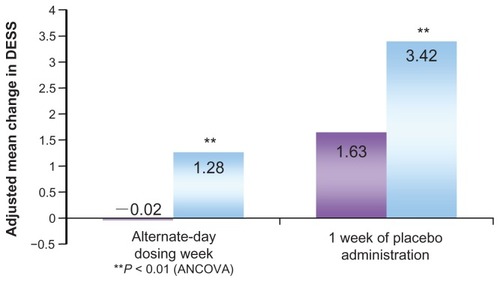
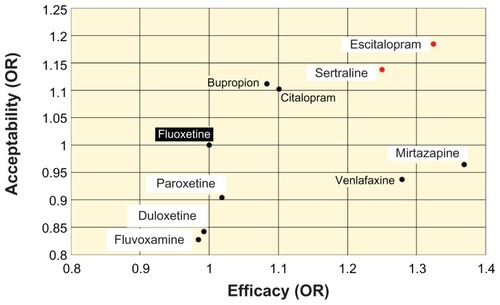
Figure 5 Efficacy and patient acceptability of new antidepressant drugs.
Abbreviation: OR, odds ratio.