Abstract
Intrapartum use of oxytocin should entail controlled dosages administered through infusion, continual monitoring of mother and fetus and surgical back-up, since several adverse outcomes have been reported. However, in Uttar Pradesh, north India, small-scale ethnographic studies as well as a large-scale retrospective survey have established that unmonitored intramuscular oxytocin injections are commonly given to birthing mothers to augment labour by unregistered local male practitioners and auxiliary nurse-midwives employed by government during home deliveries. India’s reproductive and child health policy needs to address the inappropriate use of oxytocin. Under a new 2007 policy, female government health workers at peripheral institutions are to be supplied with oxytocin to inject during the third stage of labour to prevent post-partum haemorrhage. The practice of injecting oxytocin intrapartum could readily be reinforced by this policy shift. There is an urgent need to ensure that home births are safer for mothers and babies alike, since India’s current policy goals of raising the numbers of institutional deliveries, ensuring skilled attendance at birth and improving referrals for emergency obstetric care cannot be met in the foreseeable future. In a context of enduringly high infant and maternal mortality, especially in Uttar Pradesh and other large northern states, the question of whether or not inappropriate use of oxytocin is contributing to maternal and newborn morbidity and mortality deserves further research.
Résumé
Pendant l’accouchement, l’ocytocine doit être administrée à doses contrôlées et par perfusion, avec une surveillance permanente de la mère et du fłtus et une assistance chirurgicale, puisque des effets indésirables graves ont été notifiés. Néanmoins, dans l’Uttar Pradesh, en Inde septentrionale, des études ethnographiques à petite échelle et des enquêtes rétrospectives de grande envergure ont montré que des injections intramusculaires non surveillées d’ocytocine sont fréquemment administrées aux femmes pour accélérer le travail par du personnel masculin local non diplômé et des infirmières-sages-femmes auxiliaires employées par l’État pendant les accouchements à domicile. La politique indienne de santé génésique et infantile doit se pencher sur l’administration impropre d’ocytocine. En vertu d’une nouvelle politique de 2007, le personnel de santé féminin employé par l’État dans des institutions périphériques doit recevoir de l’ocytocine à injecter pendant le troisième stade de l’accouchement, pour éviter les hémorragies post-partum. Cette modification pourrait renforcer la pratique de l’injection d’ocytocine pendant l’accouchement. De plus, il est urgent de veiller à ce que les naissances à domicile deviennent plus sûres pour les mères et les bébés, puisque les objectifs actuels de l’Inde qui consistent à relever le nombre de naissances en milieu hospitalier, garantir une assistance qualifiée pendant l’accouchement et améliorer le transfert des urgences obstétricales ne seront pas atteints à brève échéance. Alors que la mortalité maternelle et infantile demeure élevée, particulièrement dans l’Uttar Pradesh et d’autres grands États du nord, la question de savoir si l’utilisation impropre de l’ocytocine contribue ou non à la morbidité et la mortalité de la mère et du nouveau-né mérite davantage de recherches.
Resumen
El uso de oxitocina intraparto debe implicar dosis controladas administradas por infusión, monitoreo continuo de la madre y el feto, y respaldo quirúrgico, dado que se han informado varios resultados adversos. Sin embargo, en Uttar Pradesh, en la India septentrional, los estudios etnográficos de pequeña escala, así como una encuesta retrospectiva de gran escala, han establecido que las inyecciones intramusculares de oxitocina sin monitoreo comúnmente son administradas por prestadores de servicios de sexo masculino no titulados y enfermeras-parteras auxiliares empleadas por el gobierno, durante el parto domiciliario a fin de aumentarlo. La política de la India en cuanto a la salud reproductiva y la salud infantil debe tratar el uso indebido de oxitocina. En conformidad con una nueva política de 2007, las trabajadoras de salud gubernamentales en instituciones secundarias deben ser suministradas con oxitocina para inyectarla durante la tercera etapa del parto a fin de evitar la hemorragia posparto. La práctica de inyectar oxitocina intraparto fácilmente podría ser reforzada por ese cambio en política. Existe una necesidad urgente de garantizar que el parto domiciliario sea seguro tanto para la madre como para el bebé, dado que en el futuro inmediato no es posible lograr los objetivos de la política actual de la India de incrementar el índice de partos institucionales, garantizar asistencia calificada durante el parto y mejorar las referencias para cuidados obstétricos de emergencia. En un contexto de mortalidad materna e infantil perdurablemente altas, especialmente en Uttar Pradesh y otros estados septentrionales importantes, la interrogante en cuanto a si el uso indebido de oxitocina contribuye o no a la morbimortalidad de madres y recién nacidos amerita ser investigada más a fondo.
Oxytocin is a natural hormone responsible for uterine contractions and the ejection of breastmilk. Nowadays, commercially produced synthetic oxytocin is internationally the most widely known drug used clinically during labour and the post-partum period.Citation1 Oxytocin has three primary uses during delivery:
| • | Labour induction – up to a quarter of labours in western countries are artificially initiated, using oxytocin infusion and artificial rupture of membranes to cause uterine contractions and the progressive dilatation and effacement of the cervix. | ||||
| • | Labour augmentation – when labour has been arrested or is progressing slowly. | ||||
| • | Controlling post-partum haemorrhage – oxytocin administered in the third stage of labour (i.e. after the baby is born but before the placenta has been delivered) is a very effective drug for reducing blood loss.Citation2 | ||||
Oxytocin use to prevent post-partum haemorrhage requires few precautions. For intrapartum use, however, oxytocin is generally administered at a controlled rate by intravenous infusion of a limited amount of oxytocin diluted with isotonic solution. Cases for induction and augmentation should be chosen carefully and maternal and fetal status should be monitored regularly, with surgical back-up available for caesarean section if necessary.Citation1Citation3 Intramuscular use is not recommended. Since it is rapidly metabolised in the gastro-intestinal tract, it is not used orally.
Oxytocin is one of the most important drugs used in obstetric practice. Nevertheless, several adverse maternal and fetal outcomes of intrapartum use have been reported, even in highly monitored institutional settings, for example:
| • | High dosages create hyperstimulation, which can lead to precipitate labour, perineal tears, uterine rupture and fetal distress.Citation4 | ||||
| • | Oxytocin can lower blood pressure and cause imbalance of serum electrolytes, particularly lowering sodium levels (hyponatremia) and causing excess of water in the tissues.Citation1 | ||||
| • | Post-partum blood loss is greater with precipitate labour and oxytocin-and prostaglandin-induced labours, unless an oxytocic agent is continued after delivery.Citation5 | ||||
| • | Induction and augmentation of labour by oxytocin were significant risk factors in post-partum haemorrhage in Israel (OR 1.4 for both).Citation6 | ||||
| • | An increase in intrapartum oxytocin use between 1995 and 2001 in Sweden was associated with increased operative delivery (OR 4.0; 95% CI 3.7–4.2); Apgar score <7 (OR 2.3; 95% CI 1.8–2.9) and neonatal intensive care (OR 1.6; 95% CI 1.5–1.7), especially in shorter deliveries (≤12 hours).Citation7 | ||||
| • | A study from Sweden reported that one third of 77 malpractice claims in 1996–2003 were related to injudicious oxytocin use, improper interpretation of fetal monitoring tracings and failure to recognise fetal distress that resulted in brain damage or death.Citation8 | ||||
| • | A retrospective study of 126 cases of uterine rupture in BP Koirala Institute of Health Sciences, Nepal, between February 1999 and January 2004, reported a strong association between oxytocin use in second stage and uterine rupture where previous delivery was by caesarean section.Citation9 | ||||
Birthing in Uttar Pradesh
In March 2007, the population of Uttar Pradesh was projected to be 186.8 million,Citation10 with an estimated 5.8–6 million births annually. The overwhelming majority of births, especially in rural areas, take place at home.Citation11 In 2005–2006, the National Family Health Survey-3 interviewed 12,183 women aged 15–49 in Uttar Pradesh: 8.8% had delivered in government health facilities, 13.9% in private hospitals and clinics, and the remainder (over 77%) at home.Citation12 Of the women who gave birth at home in the three years prior to the survey, 6.2% were attended by a traditional birth attendant and 8.3% were attended by a doctor or nurse; the remainder were attended by relatives or untrained birth attendants.Citation12 Villagers, however, generally use the term “doctor” to refer to untrained rural practitioners as well as trained MBBS doctors, so the National Family Health Survey may be underestimating the presence of informal health care providers during home deliveries. Moreover, these surveys have collected no information about oxytocin use. Consequently, the National Family Health Survey data can say very little about the extent and distribution of medical intervention in home deliveries in north India, particularly intrapartum oxytocin use.
On the other hand, several small-scale studies indicate considerable involvement of untrained practitioners in home deliveries in rural Uttar Pradesh and the frequent use of intrapartum injections of oxytocin. Studies from elsewhere in India indicate that this practice is widespread, as do anecdotal reports from contacts in Bangladesh, Nepal and Pakistan (Personal communications: Marge Koblinsky, Ian Harper, Khawar Mumtaz).
Research in two villages in Bijnor district, western Uttar Pradesh, indicates that between 1983 and 1987, oxytocin was administered by intramuscular injection by the government pharmacist as part of his (illegal) private practice in about 15% of deliveries (n=237).Citation13 In 1998–2002, oxytocin injections were administered by untrained private rural medical practitioners (male) in almost half (48%) of deliveries (n=346).Citation14 Of those, 62.3% of primagravidae (n=53) (whose labours can normally be expected to be longer than others) received injections, compared with 45% of women of higher parities (n=293). Oxytocin was not used to induce labour. Rather, village women saw intrapartum oxytocin injections as the only effective method of speeding up labour. Folk methods still common in the early 1980s had all but disappeared by the early 2000s, and male practitioners were called to attend established labours that the labouring women and/or their female family members and dās (traditional birth attendants) considered to be protracted. These injections were termed dard barhāna (pain-or contraction-increasing) and were popular with women who wanted labour to be over quickly. At Rs 100 to Rs 150 per injection in the early 2000s, they were not prohibitively costly. Many women reported having had several injections within the space of a few hours. Dās, however, did not monitor the frequency or strength of contractions or routinely assess cervical dilatation before summoning the male practitioners. Similarly, the male practitioners did not perform internal examinations and rarely examined the labouring woman externally to ascertain the baby’s presentation. Several women reported footling breech or transverse presentations that were not diagnosed before the administration of oxytocin. Further, the male practitioners and the dās possessed no monitoring technology that would enable timely diagnosis of fetal or maternal distress after the injections had been administered: there were no fetal stethoscopes or trumpets, and no equipment to determine labouring women’s blood pressure or the intensity of uterine contractions. Whilst some of this information is based on direct observations, much of it relies on recall by women about their birthing experiences. Thus, we cannot be unequivocal in our conclusions.
A study conducted in rural Kanpur reported similar patterns of use, although the absolute levels were lower at 23% (n=527),Citation15 whilst a study conducted in 12 Uttar Pradesh districts indicated similar oxytocin use in home deliveries (48.2%; n=2,992) across the state (ranging from 74.7% in Muzaffarnagar to 16.7% in Chitrakoot), with almost two-thirds of the women who reported injections having had more than one.Citation16 Both studies found that oxytocin use was more common in primagravidae. It was also more common among women of higher socio-economic status and relatively more educated women, suggesting that oxytocin was used less because of need and more because of ability to pay and an association with “modernity”. This last point is echoed in another study conducted in Sitapur district, where Pinto argues that injections enable local practitioners to re-assert their quasi-institutional authority through association with modern biomedicine.Citation17 In the 12-district study, the traditional birth attendant and the auxiliary nurse-midwife were the primary decision makers for using the injection (29.8% and 29.6% respectively) and the informal private practitioner and the auxiliary nurse-midwife were the primary injection service providers (48.2% and 32.8% respectively).Citation16 In the Kanpur study, there was a statistically significant relationship between injection use and the presence of a provider (trained or otherwise), and there was no clear link between oxytocin use and perceptions of complications.Citation15
A Karnataka study reports that oxytocics were injected in 21% of home deliveries, including more than half those attended by government auxiliary nurse-midwives;Citation18 in institutional deliveries, “[m]ore than 90% of all women, and more than 75% of women with no complications, were given repeated injections or intravenous infusions of oxytocics to hasten labour”.Citation18 Reports from elsewhere in rural Karnataka also indicate widespread intrapartum use of oxytocin,Citation19 whilst in Chennai, intrapartum oxytocin use was normalised as a form of “crowd control” in busy hospitals and “almost routine” for the local multi-purpose health worker during home deliveries.Citation20Citation21 A study in a poor area of Delhi reported oxytocin use in 68.9% of home deliveries, administered by private doctors in 86.8% of cases.Citation22
These studies are relatively small-scale and did not include appropriate control populations. Nevertheless, women who had had intrapartum oxytocin injections experienced higher levels of stillbirths, and neonatal deaths and morbidity (possibly connected with fetal asphyxia) than those who had no injections.Citation15Citation16 In the study across 12 Uttar Pradesh districts,Citation16 preliminary bi-variate analysis indicated higher rates of hospital delivery (OR 4.11; CI 3.21–5.27) and of caesarean section (OR 2.59; CI 1.30–5.24) than among women who had not had oxytocin injections, and women’s more frequent complaints of complications during delivery (OR 5.72; CI 4.07–8.08) and perceptions that their labour had been very difficult (OR 3.72; CI 2.93–4.74). Because of the small sample size, there were few maternal deaths and this study found no statistically significant differences in maternal mortality between those women who had had oxytocin injections and those who had not. There were, however, significant differences in stillbirths (OR 1.74; CI 1.02–2.97), neonatal deaths (OR 1.52; CI 1.06–2.20), babies born very weak (OR 1.96; CI 1.56–2.93) and mothers’ perception of having had a difficult post-partum period (OR 2.13; CI 1.56–2.46). In rural Bijnor, by the early 2000s, 20% of women who had oxytocin injections eventually delivered in institutions, compared to 9% of all women in the two villages giving birth in that period.Citation14
These are, of course, no more than suggestive associations, and adverse effects of oxytocin use cannot be conclusively established. But they merit further research: intramuscular injections rather than controlled infusion, the failure to ascertain the status of the mother and baby before administration, and the lack of monitoring thereafter are all out of line with the protocols for oxytocin use.
Concluding comments
The widespread inappropriate intrapartum use of oxytocin is occurring in a context of enduringly high infant and maternal mortality in India, especially in Uttar Pradesh and other large northern states. In 2005, India’s infant mortality rate was 58 (95% CI 57–60) whilst that in Uttar Pradesh was 73 (95% CI 69–77).Citation23 According to estimates for 1998–99, India’s overall stillbirth rate was 39 per 1,000 deliveries; the neonatal mortality rate was 43 per 1,000 live births, of which deaths within the first week accounted for 33.Citation24 Perinatal and neonatal mortality rates are dropping much more slowly than those for older infants. Maternal mortality ratios remain high in India, especially in the large northern states such as Uttar Pradesh. Recent estimates for India overall range from over 500 per 100,000 live births in 2000,Citation25 to 301 in 2001–03.Citation26 The latter study estimated the maternal mortality ratio in Uttar Pradesh in 2001-03 to be 517, which would mean that the state accounted for about 23% of India’s maternal mortality in this period.Citation26
Since Independence, various policy initiatives have prioritised infant and maternal health.Citation27Citation28 Current targets are to achieve a maternal mortality ratio of 100 per 100,000 live births and an infant mortality rate of 30 per 1,000 live births by 2012, and recent policy emphasis has been on ensuring that women have skilled attendants during childbirth and encouraging institutional deliveries. Here, we highlight just two issues relevant to intrapartum oxytocin use: post-partum haemorrhage, and emergency obstetric care beyond the community level.
First, post-partum haemorrhage accounts for some 38% of maternal mortality in India.Citation26 Dramatic blood loss soon after delivery can result in rapid death, so there is no time to refer women to distant facilities. Thus, prevention of post-partum haemorrhage must take place where women give birth. Under a new policy in early 2007, female government health workers at peripheral institutions are to be supplied with oxytocin to inject during the third stage of labour to prevent post-partum haemorrhage. The well-established practice of injecting oxytocin intrapartum (by government and non-government providers) could readily be reinforced by this policy shift.
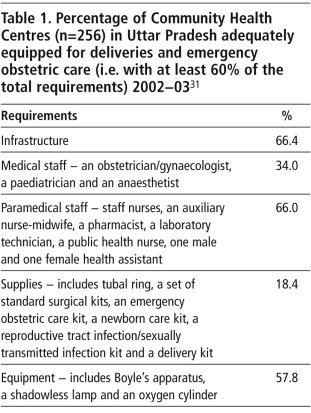
Second, a crucial assumption behind the advocacy of institutional deliveries is that there is (or soon can be) sufficient institutional capacity. This is reflected, for instance, in the Janani Suraksha Yojana (Motherhood Protection Programme) cash assistance scheme to promote universal institutional delivery among poor pregnant women.Citation29 Yet government institutions in Uttar Pradesh are currently incapable of accommodating even routine deliveries, leave aside dealing with complications that require emergency care. Uttar Pradesh’s Community Health Centres, which would be expected to act as first referral units for complications, are inadequately equipped and staffed. All Community Health Centres in Uttar Pradesh were surveyed in 2002–03 (see Table 1). Less than 20% had even 60% of the basic equipment needed to handle an obstetric emergency, and barely a third had 60% of the qualified medical staff required.Citation30 Transport facilities to enable timely referral to urban facilities were also rarely available.
Table 1. Citation31
One reflection of the government health sector’s inadequacies is that all but two of the 54 institutional deliveries between 1993–2002 in the Bijnor study took place in private nursing homes in Bijnor town, of which around 20 offer inpatient maternity care. Most, however, are small-scale (almost half have fewer than 15 beds and most of the remainder had no more than 20), and they also lack crucial facilities (e.g. blood, oxygen, resident anaesthetist, neonatal resuscitation equipment and incubators).Citation32 They are by no means unusual in that.Citation33 As elsewhere in India, the costs of private obstetric care, including for caesarean sections, are higher and more variable than in government facilities.Citation34–36
Thus, in Uttar Pradesh neither government nor private sector can ensure timely care for rural women experiencing obstetric emergencies at appropriate (and affordable) health care facilities. Two points germane to the inappropriate use of oxytocin arise from this. The best-practice recommendation is that oxytocin is administered only if there is surgical back-up for an emergency caesarean section. Clearly, that stipulation is not being met in Uttar Pradesh (or, indeed, many other parts of India). Further, implementing functioning referral systems and ensuring that all birth attendants are appropriately skilled cannot be achieved overnight. In rural Uttar Pradesh, at least, most women will continue to deliver at home (rather than in institutions) for some time to come and will be attended by relatives and various other personnel, among them traditional birth attendants, untrained private rural medical practitioners (male) and auxiliary nurse-midwives. Thus, there is an urgent need for policy initiatives to ensure that home births are safer for mothers and babies alike.
Current usage patterns of oxytocin in home deliveries fall far short of international recommendations. This, we suggest, is sufficiently worrying to warrant further research to assess whether, and if so to what extent, unmonitored intrapartum injections of oxytocin may be contributing to the continuing high levels of maternal and neonatal morbidity and mortality in rural north India. In the short term, maternal and neonatal health campaigns should include messages about oxytocin misuse and policy initiatives such as the Integrated Management of Neonatal and Childhood Illness and the National Rural Health Mission should also take this into account. In the longer term, more far-reaching efforts are needed to improve state regulation of rural medical practice to ensure that minimum standards are met.
Acknowledgements
Patricia and Roger Jeffery wish to thank the Economic and Social Research Council for funding their Bijnor research in 1982–83 and 1985 and the Wellcome Trust who funded their research in 2002–04. Abhijit Das is grateful to the Mahila Samakhya of UP for their help in conducting the 12-District Study.
References
- J Smith, D Merrill. Oxytocin for induction of labor. Clinical Obstetrics and Gynaecology. 49(3): 2006; 594–608.
- Elbourne DR, Prendiville WJ, Carroli G, et al., Prophylactic use of oxytocin in the third stage of labour. Cochrane Database of Systematic Reviews 2001 (4:CD001808).
- GG Briggs, SR Wan. Drug therapy during labor and delivery, part 2. American Journal of Health-System Pharmacists. 63(15 June): 2006; 1131–1139.
- CEC den Hertog, ANJA de Groot, PWJ van Dongen. History and use of oxytocics. European Journal of Obstetrics & Gynecology and Reproductive Biology. 94(1): 2001; 8–12.
- H Phillip, H Fletcher, M Reid. The impact of induced labour on postpartum blood loss. Journal of Obstetrics and Gynaecology. 24(1): 2004; 12–15.
- E Sheiner, L Sarid, A Levy. Obstetric risk factors and outcome of pregnancies complicated with early postpartum hemorrhage: a population-based study. Journal of Maternal Fetal and Neonatal Medicine. 18(3): 2005; 149–154.
- M Oscarsson, I Amer-Wahlin, H Rydhstroem. Outcome in obstetric care related to oxytocin use. A population-based study. Acta Obstetricia et Gynecologica Scandinavica. 85(9): 2006; 1094–1098.
- M Jonsson, SL Norden, U Hanson. Analysis of malpractice claims with a focus on oxytocin use in labour. Acta Obstetricia et Gynecologica Scandinavica. 86(3): 2007; 315–319.
- N Chuni. Analysis of uterine rupture in a tertiary center in Eastern Nepal: lessons for obstetric care. Journal of Obstetric and Gynaecological Research. 32(6): 2006; 574–579.
- Registrar-General India. Report of the Technical Group on Population Projections constituted by the National Commission on Population, Office of the Registrar General and Census Commissioner India. 2006
- S RamaRao, L Caleb, ME Khan. Safer maternal health in rural Uttar Pradesh: do primary health services contribute?. Health Policy and Planning. 16(3): 2001; 256–263.
- Ministry of Health and Family Welfare. NFHS-3 (2005–06) Fact Sheets (Provisional Results). 2006. At: <http://mohfw.nic.in/nfhsfactsheet.htm> Accessed 5 April 2007
- P Jeffery, R Jeffery, A Lyon. Labour Pains and Labour Power: Women and Childbearing in India. 1989; Zed Books: London.
- Jeffery P, Jeffery R. Safe motherhood and/or the health care market: a twenty year perspective from UP. Paper presented at workshop on Post-Liberalization State in India. Stanford, June 2005. (Unpublished)
- M Sharan, D Strobino, S Ahmed. Intrapartum oxytocin use for labor acceleration in rural India. International Journal of Gynecology and Obstetrics. 90: 2005; 251–257.
- Das A, Agarwal M, Tripathi K, et al. Use of pre-delivery injections during home deliveries in rural north India: implications for maternal and neonatal health programmes under NRHM. Paper presented at 10th International Women’s Health Meeting, New Delhi, 21–25 September 2005. (Unpublished)
- S Pinto. Development without institutions: ersatz medicine and the politics of everyday life in rural north India. Cultural Anthropology. 19(3): 2004; 337–364.
- Z Matthews, J Ramakrishna, S Mahendra. Birth rights and rituals in rural south India: care seeking in the intrapartum period. Journal of Biosocial Science. 37: 2005; 385–411.
- A George, A Iyer, G Sen. Gendered health systems biased against maternal survival: preliminary findings from Koppal, Karnataka, India. Working Paper 253. 2005; Institute of Development Studies: Brighton.
- C Van Hollen. Birth on the threshold: childbirth and modernity in south India. 2003; University of California Press: Berkeley.
- C Van Hollen. Invoking Vali: painful technologies of modern birth in South India. Medical Anthropology Quarterly. 17(1): 2003; 49–77.
- LE Caleb. Women’s health in the postpartum period and the influence of infant gender on postpartum practices in a low-income community in Delhi, India. 1995; Johns Hopkins University School of Hygiene and Public Health: Baltimore.
- Registrar-General India. Sample Registration Bulletin 2006;41(1). New Delhi: Registrar-General India, 2006.
- International Institute for Population Sciences/ORC Macro. National Family Health Survey-2 1998–99: India. 2000; International Institute for Population Sciences/ORC Macro: Mumbai/Calverton, MD.
- Smit J. Millennium Development Goals: Progress in Asia and the Pacific 2006, United Nations Economic and Social Commission for Asia and the Pacific, United Nations Development Programme, Asian Development Bank.
- Registrar-General India. Maternal Mortality in India, 1997–2003: Trends, Causes and Risk Factors I. Registrar General/Centre for Global Health Research, University of Toronto. 2006
- Ministry of Health and Family Welfare. National Population Policy. 2000; Ministry of Health and Family Welfare, Government of India: New Delhi.
- Ministry of Health and Family Welfare. National Health Policy. 2002; Ministry of Health and Family Welfare, Government of India: New Delhi.
- Ministry of Health and Family Welfare. Janani Suraksha Yojana: Features and frequently asked questions and answers as in October 2006. 2006; Maternal Health Division, Government of India: New DelhiAt: <http://mohfw.nic.in/dofw%20website/JSY_features_FAQ_Nov_2006.htm>. Accessed 9 April 2007
- International Institute for Population Studies. Facility Survey National Report under Reproductive and Child Health Project Phase II. IIPS. 2003 At: <www.rchindia.org/fs_india.htm>
- Ministry of Health and Family Welfare. Uttar Pradesh Facility Survey 2002–2003. 2003; Ministry of Health and Family Welfare, Government of India: New Delhi.
- Jeffery P, Jeffery R. “Money itself discriminates”: obstetric emergencies in the time of liberalisation. Contributions to Indian Sociology (Forthcoming)
- A Jesani. Social objectives of health care services: regulating the private sector. KS Prabhu, R Sudarshan. Reforming India’s Social Sector: Poverty, Nutrition, Health and Education. 2003; Social Science Press: New Delhi, 205–220.
- S Chakraborty. Private Health Provision in Uttar Pradesh, India. DH Peters, AS Yazbeck, RR Sharma. Better Health Systems for India’s Poor. 2002; World Bank: Washington DC, 257–277.
- SJ Jejeebhoy, L Caleb Varkey. Maternal health and pregnancy-related care. SJ Jejeebhoy. Looking Back, Looking Forward: A Profile of Sexual and Reproductive Health in India. 2004; Rawat Publications/Population Council: Jaipur/New Delhi, 44–87.
- S Mishra. Public health scenario in India. KS Parikh, R Radhakrishna. India Development Report 2004–05. 2005; Oxford University Press for Indira Gandhi Institute of Development Research: New Delhi, 62–83.
