Abstract
This study aimed to compare the confidence of oncology consultants and specialist registrars (SpRs) in the performance of practical procedures, to contrast this with confidence in other areas of practice and to determine at what grade they felt most confident. Questionnaires were sent to all 57 oncology consultants and SpRs in the South-West region. Respondents scored confidence on a five-point Likert scale. The response rate was 70%. SpRs were significantly more confident in cardiopulmonary resuscitation (p = 0.003) and central line insertion (p = 0.006). Consultants were significantly more confident in developing management plans (p = 0.001) and performing committee work (p = 0.002). Only 6% of consultants felt most confident performing practical procedures as a consultant, and were less confident about these than other tasks (p = 0.001). Some 86% of SpRs considered they were more confident performing practical procedures as senior house officers (SHOs). In conclusion, self-reported confidence in performing practical procedures declines during career progression in oncology. This raises questions about the teaching and supervision of these procedures. If there is a greater emphasis on a consultant-provided service, their educational needs will need to be recognized and retraining or outsourcing of these procedures to other specialties may be necessary.
Introduction
Many competences will be acquired at medical school and during early postgraduate years (Marel et al., Citation2000; Liddell et al., Citation2002). Continuing professional development is an ongoing process and is concerned with not only the acquisition but also the maintenance of competences. The General Medical Council state the importance of this ongoing developmental and maintenance process in the Good Medical Practice guide (General Medical Council, Citation2001). More specifically for oncologists, a similar message is described in the Royal College of Radiologists’ publication Continuing Professional Development (2001). There is, however, a lack of published evidence regarding the maintenance of competences over the long term (Macnab & Macnab, Citation1999; Hammond et al., Citation2003).
In the UK there are calls for a consultant-provided service as an integral part of the multidisciplinary team delivering patient care, and for consultants to be involved in training and assessing junior doctors and medical students (http://www.dh.gov.uk, 2005). One of the authors (KB) identified that she would require retraining in some practical procedures currently undertaken on oncology wards if this were to be the case.
Practice points
The aims of the study were:
to determine if there was a significant difference between the confidence of oncology consultants and SpRs in performing practical procedures;
to identify at which grade consultants and SpRs felt most confident;
to determine whether differences in confidence were related to time since graduation;
to compare the confidence of consultants and SpRs in performing practical procedures with their confidence in performing other aspects of their role.
Methods
The number and type of practical procedures performed in an adult cancer centre serving a population of approximately 1,000,000 were ascertained from April 2003 to March 2004 inclusive. Data were obtained retrospectively from hospital records using codes from the OPCS classification for the relevant procedures. During this time, a practical procedure (other than intravenous infusions) was performed on 8% of the 2674 discharged cases. There were 84 ascitic drains, 77 pleural taps, 27 chest drains and 13 lumbar punctures. Cardiopulmonary resuscitation and central line insertion were not coded. This information was used to design a questionnaire that was sent to all oncology consultants and SpRs in the South-West Region. The questionnaires were anonymous and included questions about year of medical qualification and grade. Respondents scored on a five-point Likert scale (five being most confident) their confidence in a number of tasks. The Likert scale was used as an ordinal measure of the attitude of respondents, ensuring that median values were used as a measure of central tendency and non-parametric statistics in data analysis (Jamieson, Citation2004).
The tasks investigated were:
Group 1 tasks: commonly undertaken by trainees—i.e. cardiopulmonary resuscitation, draining ascites, tapping pleural effusions, inserting chest drains and performing lumbar punctures.
Group 2 tasks: procedures undertaken on oncology patients but usually by an anaesthetist—e.g. central line insertion. These are, however, performed by SHOs in other posts on a medical rotation.
Group 3 tasks: regularly undertaken by consultants—e.g. formulating radiotherapy plans, developing management plans and non-clinical tasks of teaching and committee work.
The confidence ratings for each item were compared between consultants and SpRs using Mann–Whitney U-tests. Within each grade, a division was made into those that had qualified earlier and later than the median year of qualification. Confidence ratings were then compared between those qualified earlier and later, for each grade separately, using Mann–Whitney U-tests. Confidence ratings for all the clinical and non-clinical items were compared with one another using Wilcoxon matched pairs signed-rank tests for consultants and for SpRs. Since multiple comparisons were being made between groups, a significance level of p < 0.01 was used. All statistical analysis was performed using SPSS version 12.0.
Results
In total, 40 of 57 (70%) questionnaires were returned: 27 of the 37 (73%) consultants responded and 13 of the 20 SpRs replied (65%). Median, 25th and 75th quartiles for the confidence scores of consultants and SpRs for the tasks are illustrated in . In the figure, where the quartile value is equal to the median value, there is no extension of the interquartile line beyond the median point.
Figure 1. Median and inter-quartile range for self-assessed confidence in tasks by consultants and specialist registrars in oncology.
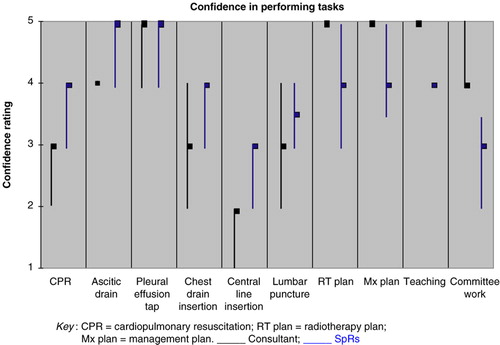
There were significant differences between SpRs and consultants, with the junior doctors being more confident in cardiopulmonary resuscitation (p = 0.003) and central line insertion (p = 0.006). Consultants were more confident in developing a management plan (p = 0.001) and radiotherapy plan (p = 0.001), as well as in performing committee work (p = 0.002).
Consultants felt most confident in performing tasks in Groups 1 and 2 at SHO (41%) and SpR (53%) level, with only 6% feeling most confident as a consultant. In comparison, 86% of the SpRs were most confident at these tasks as an SHO. When the date of medical qualification was taken into account for consultants, there was significantly less confidence in inserting a central line (p = 0.002) for those who had been qualified longer. However, 90% of consultant replies revealed superior confidence at consultant grade for the tasks in Group 3. Overall, consultants were more confident in the non-clinical skill of committee work when compared with clinical tasks (p = 0.001).
Discussion
Self-reported confidence in performing tasks in Groups 1 and 2 declines in the consultant grade. One possible explanation is that doctors become more self-critical with age. For example, more time spent in a clinical setting may include greater awareness and personal experience of recognized complications from practical procedures. The consequence of this may be that confidence is eroded. However, confidence was higher in the consultant group for tasks in Group 3, which argues against this possibility.
Another explanation is due to the recognized association between frequency of performing practical procedures and degree of self-assessed confidence (Hicks et al., Citation2000); it may be that consultants are not performing some of the clinical tasks regularly. The number of practical procedures required for competence has been examined in surgical series. Wibe et al. (Citation2005) discovered an overall survival difference in favour of the individual surgeons operating on more than 30 cases of rectal cancer per year compared with a group with experience of less than 10 per year. Similar findings were reported by Ingram et al. (Citation2005) for breast cancer patients for an individual caseload of greater compared with less than 20 in a year. However, there was no survival difference in centres treating more than 60 cases compared with less than 60 cases of prostate cancer by radical prostatectomy in a year, although the less experienced centres did have an increased complication rate (Hu et al., Citation2003). It is not clear from the literature how many of the procedures in our groups are required to maintain competence.
The model of oncology training as the acquisition of competences as the trainee progresses to become a consultant who then maintains these competences is challenged by this study. The expertise in some competences was seen by both SpRs and consultants as being held at SHO grade, despite the fact that these procedures are undertaken ostensibly under the supervision of the consultants. Further work is required to investigate how these competences are learnt by the present SHOs.
This study also has implications for implementing work-based competence assessments of F1 and F2 (first- and second-year doctors) as envisaged in Modernizing Medical Careers (http://www.mmc.nhs.uk/pages/assessment, 2005). If consultants are not confident to undertake procedures, they may be less able to assess their trainee's competence, for example in a direct observation of procedural skills (DOPS). Possible solutions include the increased availability of skills laboratories, although this may not address the problem of clinical supervision of trainees on the wards. The training needs of consultants should be recognized and transfer of some of the procedures to other departments, e.g. anaesthetics or radiology, may be indicated.
Additional information
Notes on contributors
A. H. Thomson
ALASTAIR THOMSON is a Consultant in clinical oncology and works at the Royal Cornwall Hospital.
C. J. W. Foy
CHRIS FOY works in the Research and Development Unit at Gloucester Royal Hospital.
K. Benstead
KIM BENSTEAD is a Consultant in clinical oncology and works at the Gloucestershire Oncology Centre.
References
- Evans AW, Leeson RM, Newton John T.R, Petrie A. The influence of self-deception and impression management upon self-assessment in oral surgery. British Dental Journal 2005; 198(12)765–759
- General Medical Council. Good Medical Practice3rd. GMC, London 2001
- Hammond I, Taylor J, McMenamin P. Anatomy of complications workshop: an educational strategy to improve performance in obstetricians and gynaecologists. Australia and New Zealand Obstetrics and Gynaecology 2003; 43(5)395–396
- Hicks CM, Gonzalez R, Morton MT, Gibbons RV, Wigton RS, Anderson RJ. Procedural experience and comfort level in internal medicine trainees. Journal of Internal Medicine 2000; 15(10)716–722
- Hu JC, Gold KF, Pashos CL, Mehta SS, Litwin MS. Role of surgeon volume in radical prostatectomy outcomes. Journal of Clinical Oncology 2003; 21(3)393–394
- Ingram DM, McEvoy SP, Byrne MJ, Fritschi L, Joseph DJ, Jamrozik K. Surgical caseload and outcomes for women with invasive breast cancer treated in Western Australia. Breast 2005; 14(1)11–17
- Jamieson S. Likert scales: how to (ab)use them. Medical Education 2004; 38: 1217–1218
- Liddell MJ, Davidson SK, Taub H, Whitecross LE. Evaluation of procedural skills in an undergraduate curriculum. Medical Education 2002; 36(11)1035–1041
- Macnab AJ, Macnab M. Teaching pediatric procedures: the Vancouver model for instructing Seldinger's technique of central venous access via the femoral vein. Pediatrics 1999; 103(1)E8
- Marel GM, Lyon PM, Barnsley L, Hibbert E, Parise A. Clinical skills in early postgraduate medical trainees: patterns of acquisition of confidence and experience among junior doctors in a university teaching hospital. Medical Education 2000; 34(12)1013–1015
- Mattheos N, Nattestad A, Falk-Nilsson E, Attstrom R. The interactive examination: assessing students’ self-assessment ability. Medical Education 2004; 38(4)378–389
- Royal College of Radiologists. Continuing Professional Development. RCR, London 2001
- Wibe A, Eriksen MT, Syse A, Tretli S, Myrvold HE, Soried O. Effect of hospital caseload on long-term outcome after standardization of rectal cancer surgery at a national level. British Journal of Surgery 2005; 92(2)217–224
