Abstract
This literature review describes the impact of health professional schools with a social accountability mandate by identifying characteristics of medical education found to impact positively on medical students, health workforce, and health outcomes of disadvantaged communities. A critical appraisal tool was used to identify the strengths and weaknesses of the published articles. Data are presented as a narrative synthesis due to the variety of methodologies in the studies, and characterized using a logic model. Health professional schools aiming to improve health outcomes for their disadvantaged local communities described collaborative partnerships with communities, equitable selection criteria, and community-engaged placements in underserved areas as positively impacting the learning and attitudes of students. Students of socially accountable schools were more likely to stay in rural areas and serve disadvantaged communities, and were often more skilled than students from more traditional schools to meet the needs of underserved communities. However, published literature on the impact of socially accountable health professional education on communities and health outcomes is limited, with only one study investigating health outcomes. The findings of this literature review guide schools on the inputs likely to maximize their socially accountability outputs and increase their impact on students, local health workforce and local communities.
Introduction
About 400 million people globally lack access to one or more essential health services largely because of workforce shortages, skills mix imbalances and uneven geographical distributions of professionally qualified health workers such as doctors, nurses and midwives (Dussault & Franceschini Citation2006; Lehmann et al. Citation2008). There is often a significant mismatch between health professional education and the needs of the local health system as an inevitable consequence of limited collaboration between the health and education sectors; compounded by weak links between educational institutions and the health system that employs their graduates. The under-representation of certain social and cultural groups in higher education is a worldwide phenomenon and top-down approaches to widening participation have had limited success (Thomas Citation2001). With such a massive shortage and mal-distribution of health professionals and a persistent mismatch between education and the realities of health and workforce needs, institutions that train health professionals are essential partners in making Universal Health Coverage (UHC) a reality (Frenk et al. Citation2010).
Health professional (HP) schools have a critical role in addressing inequities and developing high-quality primary health care systems, particularly in disadvantaged regions (Ross et al. Citation2014). HP schools can address this issue by producing highly relevant research, policy guidance, preventive and community-based services, and most importantly, training a health workforce that is willing, work-ready and fit-for-purpose, thus optimally suited to respond to the needs of the most vulnerable populations in their local regions (Boelen & Heck Citation1995; Palsdottir et al. Citation2008; Larkins et al. Citation2013).
Many HP schools around the world currently use community-based placements to provide experiential, holistic learning that reinforces concurrent theoretical learning. Community-Oriented Medical Education (COME) and Community-Based Medical education (CBME) are on a medical education continuum. COME provides a learning perspective on community medicine; CBME provides experiential learning and actual practice development whilst immersed within a community. While COME and CBME have the same overarching educational goals, COME provides the theoretical frame work, while CBME provides experiential learning in context and engages the participation of the community (Magzoub & Schmidt Citation2000). Two strategies are commonly used to align the priorities of health professional institutions with those of the local population are: service learning through community placements; and, more recently, longitudinal integrated clerkships (LIC). Service learning involves re-orientating health professional education toward community placements, where learners are based in the community (Seifer Citation1998; Deans Citation1999). LIC introduce patient-oriented (rather than program) block models of clinical learning, often in a community-based approach. However, persisting inequities in health outcomes have led some HP schools to develop service learning and LIC models even further to include community engagement, and have been instrumental in training graduates who are skilled and committed to stay and work in underserved rural areas – an approach described as “socially-accountable health professional education” (SAHPE). Community Engaged Medical education (CEME) stresses an interdependent and reciprocal relationship between the medical school and the community served; the community people are not just observers or recipients providing the settings for medical education training, but are also engaged and involved in the education and services to provide solutions to their health problem in the community. Students learning experientially within and through the community and not just simply about community. Students’ learning objectives and activities are fundamentally aligned to priority community health care needs with the student as the center of partnership between the community and the medical school for improving community health status (Strasser et al. Citation2015).
With the numbers of SAHPE schools rising around the world, a consortium of SAHPE institutions of learning was formed in 2008: the Training for Health Equity Network (THEnet). THEnet is committed to achieving health equity through transforming health professional education to meet local needs; working in partnership with communities to provide health services that meet community needs and undertake research that is responsive to community priorities. THEnet schools have a goal of producing health professionals for underserved communities via an equitable selection process for admitting rural applicants and applicants from underserved sub-populations, and students having (compared to more traditional approaches) longer placements in rural communities and greater involvement with local community members (Palsdottir et al. Citation2008; Larkins et al. Citation2013; Ross et al. Citation2014; Strasser et al. Citation2015; Preston et al. Citation2016). This article is part of a series of THEnet collaborative multi-institutions research on ongoing health professional education reform aiming at producing a fit for purpose health workforce.
Despite moves towards social accountability in health professional education, there has been limited evidence of effectiveness. This literature review collects evidence to answer the research question: what global evidence is available on the impact of community-engaged, equity-oriented schools using accountability principles on health services, outcomes and intermediary factors? The objectives of this literature review were to identify and analyze evidence of the impact of community-engaged, equity-oriented socially accountable health professional education (SAHPE) on medical student learning and attitudes, medical health workforce and community health equity compared to schools taking a more traditional educational approach. We focused on SAHPE schools that reported a positive impact, with the aim of identifying the factors contributing to this effectiveness. The purpose of the review was to determine what was known from published quantitative and qualitative studies, evaluation research and descriptive accounts about the inputs and activities required for successful SAPHE and their impact on communities and health services leading to improved health outcomes. This review will assist HP schools looking to become more socially accountable and increase their impact on students, communities and health equity.
Methods
Eligibility criteria
Empirical, peer-reviewed published studies showing evidence of impact of socially accountable medical education on retention of the medical health workforce, regional health, community health, health equity, or health systems were included regardless of design or methodology, in order to be comprehensive and address the paucity of published literature.
Search strategy
Co-authors of the review at the School of Medicine at Flinders University (Flinders) and James Cook University College of Medicine and Dentistry (JCUCMD), both located in Australia, undertook an initial targeted search of the International literature using Medline (via Ovid) and PubMed. To identify key terms, this initial search was then followed by analysis of the text contained in each title, abstract and index terms used to describe the article.
A second, more extensive search of the international literature was then undertaken using these identified key search terms to comprehensively identify relevant studies. The search strategy was limited to English Language, but used a wide range of subject headings and keywords to increase the sensitivity of the search. No date or study design restrictions were applied to keep the search inclusive. A last, detailed search was then constructed in Medline and then translated for each database; PubMed, ERIC (OvidSP), CINAHL, Scopus, Web of Science, Informit, ProQuest (Health & Medicine, Education, Social Sciences), PAIS international and Google Scholar to be consistent with the subject headings and keywords to reduce any bias. A combination of subject headings and text-words were used in databases allowing subject headings searching (). These searches were conducted in November 2014 within Ovid Medline, CINAHL, PubMed, Scopus, Web of Science, ProQuest, ERIC, Informit, PAIS International and Google Scholar and repeated on 29 July 2016 to include more recent papers (). EndNote Library X7.1 software (Philadelphia, PA) was used to manage the articles and remove duplicates.
Table 1. Characteristics of database search for systematic review.
Finally, contact with social accountability content experts resulted in additional articles relevant to our study being identified, and the reference list of included studies was checked by the authors.
Study selection
The title and abstract of each article were independently assessed and evaluated for inclusion by two researchers; disagreements were resolved by consensus of all the co-authors.
Data extraction and synthesis
Data were extracted and summarized from the final studies using a specifically designed table (). The studies were different with respect to design, context and type of impact. This heterogeneity required the use of a narrative approach. A program logic model was used to tabulate studies and identify the impact on student learning and attitudes and health workforce as short- and medium-term impacts expected to lead to improved health outcomes and the long-term goals of improved health equity.
Table 2. Program evaluation logic model.
Quality appraisal
Study quality was appraised using the critical appraisal criteria tool (). Studies were assessed as excellent, good, average, poor, very poor and could not assess. Studies classified as poor and very poor were excluded.
Table 3. Critical appraisal criteria questions.
Review results
Description of studies and assessment of their methodological quality
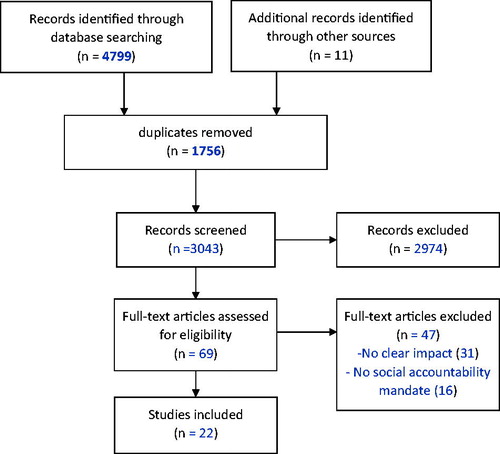
Overall, 4799 citations were retrieved with a further 11 studies identified and screened and 1756 duplicates removed, 2974 were excluded after reading the titles/abstracts, leaving 69 articles to be reviewed in full. Forty-seven citations were later eliminated as they did not meet inclusion criteria or were of poor quality. The remaining 22 papers were included in the final review ().
Figure 1. Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) protocol for study selection process (Moher et al. Citation2009).
There was a paucity of published evidence of the impact of socially accountable medical education, due perhaps to the relatively short time since the establishment of many of the HP schools with a social accountability mandate, and the multifactorial nature of influences on health. The decision was made to use program logic methodology to capture the inputs and activities of schools that lead to increased impact. Impact was categorized as: impact on student learning and attitudes; medical workforce; and, community health outcomes.
The majority of the studies were from high-resource countries with 10 studies from a low resource context. Most of the studies were descriptive comparator or pre-test:post-test studies with only one randomized controlled study. Study quality was mixed with some studies having limited methodology and outcome detail.
Eleven papers studied the impact on student learning with nearly all (10) using self-reported surveys, 5 of which reported rural placements are at least as effective as metropolitan-based placements for clinical education, with 1 study finding no statistical difference (Table 4, available online as Supplemental Material). Four studies reported increased student focus on community primary health care and community needs, while 6 studies using surveys and practice location data described a positive impact on medical workforce composition, retention in areas of need, and quality of graduates (Table 5, available online as Supplemental Material).
There were 5 studies which reported impact on communities, with 1 describing a decrease in infant mortality rates, 1 showing increased service delivery for underserved communities, 2 finding students reported positive changes in health seeking behaviors in the communities they visited, and 1 study that used patient interviews to reveal students underwent professional identity transformation in communities (Table 6, available online as Supplemental Material).
School characteristics
Important inputs of exemplary “socially accountable” schools include preferential selection processes to admit and support students from local rural communities and underserved population groups. A number of SAHPE medical schools have successfully implemented preferential selection processes to admit and support (including financially) students from local rural communities and underserved population groups into medical and health professional schools whom otherwise would not have had the opportunity to train as a health professional (Iputo Citation2008; Reid et al. Citation2011; Elsanousi et al. Citation2016). For example, Walter Sisulu University in South Africa introduced more equitable student selection involving a quota to increase the number of students from minority ethnic groups, which dramatically increased the number of black African doctors and students, and decreased the attrition rate for black students from 23% to fewer than <10% (Iputo Citation2008).
Studies also suggest establishing formal partnerships or relationships between local communities, health services and the HP schools contributes significantly to quality teaching, research and advocacy activities that are relevant to local health services and population needs (Chang et al. Citation2011). Also valuable are: explicit faculty mission statements around a social accountability mandate; the recruitment of staff committed to this vision; partnerships with local communities and other organizations; and, being located in under-served areas with the adequate resource commitment to ensure sustainability (Chang et al. Citation2011). In some cases, these partnerships led to the expansion of health services into underserved communities and increased access to appropriate health care (Elsanousi et al. Citation2016).
Student experiences and activities
Providing positive rural clinical and educational experiences also plays a major role in producing health professionals willing and able to work in underserved areas (WHO Citation2010). The SAHPE approach includes community-based service learning that is significantly longer than used by other medical schools. JCUCMD and Flinders have at least 20 weeks of rural clinical placements, while Northern Ontario School of Medicine (NOSM) in Canada and Ateneo de Zamboanga University, School of Medicine (ADZU-SOM) and University of the Philippines Manila, School of Health Sciences (UPM-SHS) in the Philippines have an entire year (Strasser et al. Citation2013; Ross et al. Citation2014).
Some SAHPE schools also add integrated public health components to their community activities, usually involving the principles of participatory action research, to further prepare students to address local health problems (Jinadu et al. Citation2002; Cristobal & Worley Citation2011).
Impact of socially accountable medical schools on student learning and attitudes
Community placements replicate situations in which most students eventually practice medicine (Satran et al. Citation1993). In contrast, hospital-based teaching often provides relatively small proportions of inpatients both well enough and available for medical students to approach (Sen Gupta et al. Citation2014).
Studies evaluating student placements in rural communities show positive impacts on student competencies; with rurally-based students doing at least as well, and many doing better in developing clinical skills than students studying in traditional, metropolitan hospital-based training sites (Satran et al. Citation1993; Worley et al. Citation2004a, Citation2004b; Iputo & Kwizera Citation2005; Mohamed et al. Citation2014).
There is also some evidence that having most undergraduate training taking place in the community or community health units rather than on campus and in teaching hospitals – a key SAHPE approach – leads to more competent graduates. For example, the internship performance of the first two classes of the University of Gezira medical school (a SAHPE institution) was assessed by senior doctors and found to be better (45%) or comparable to (50%) other medical school graduates who previously worked with the same senior doctors (Rahim et al. Citation1992).
Students training in rural areas also seem pleased with their experience (Satran et al. Citation1993; Howe Citation2001); with several studies showing students report a stronger learning experience rurally than they would have in a metropolitan area (Worley et al. Citation2004b; Birden & Wilson Citation2012; Couper et al. Citation2011; Chang et al. Citation2011; Okayama & Kajii Citation2011). Students also self-report that community placements highlight the importance of dealing with people rather than diseases, and the visual impact of the social environment on health (Howe Citation2001).
Impact on medical workforce
A key strategy for graduating a workforce willing to respond to the needs of the local health system and most vulnerable populations is through providing opportunities for students from the local areas, and in particular from local underserved communities, to enter medical education (Frenk et al. Citation2010).
In addition, longitudinal rural placements have also been shown to increase the desire of students for general practice (Howe & Ives Citation2001; Amalba et al. Citation2016) and rural community service (Howe & Ives Citation2001; Jinadu et al. Citation2002; Amalba et al. Citation2016; Worley et al. Citation2004b; Okayama & Kajii Citation2011). There is also some additional evidence, based on rural patient feedback, that students undergo professional identity transformation in community-based, longitudinal learning environments (Hudson et al. Citation2012).
It must be noted, however, that one US and one Canadian study (Easterbrook et al. Citation1999) contrastingly showed no association between undergraduate exposure to rural practice and graduate rural practice location (though the length of this rural exposure was not provided in either study).
Thus, a significant amount of literature shows community-based training leads to positive student clinical learning experiences, and at least short-term attitudinal changes towards general practice and/or community service. As a result, medical education around the world is increasingly delivered through longitudinal placements in general practice and other community settings (Birden & Page Citation2007).
There is also some evidence that medical graduates are more likely to undertake rural practice if they undertake longer rural placements (Heng et al. Citation2007), and some strong evidence from a case control study of South African medical practitioners which found rural public practice GPs were more than twice as likely to have been exposed to rural situations during their training than urban GPs, and five times more likely to state that this exposure had influenced their choice of practice location (Reid et al. Citation2011).
Strong associations with rural practice are also found in SAHPE institutions which have a selection process that equitably selects applicants from rural areas and/or underserved populations and make it mandatory for their students to undertake extensive rural placements (Iputo Citation2008; Cristobal & Worley Citation2011; Reid et al. Citation2011; Sen Gupta et al. Citation2014; Mohamed et al. Citation2014).
Two Philippines SAHPE institutions have also obtained high levels of success in graduate retention rate and distribution in local areas of need, as compared with national trends from other traditional medical schools. The Philippines Ateneo de Zamboanga University School of Medicine (ADZU-SOM), which has students spending 12 months of, where student spend one month per semester in the community from their first year, culminating in a whole year community immersion/engagement in their fourth year, has more than 80% of its graduates practicing in local areas compared to the national average of 68% of medical graduates practicing overseas. ADZU-SOM graduates often practice in areas that previously did not have a doctor, resulting in a 55% increase in the number of municipalities in Zamboanga with a doctor (Cristobal & Worley Citation2012). Similarly, more than 90% of medical graduates from University of the Philippines Manila – School of Health Science, Palo and more than 80% of midwife and nursing graduates serve in local Philippines areas of dire need.
Impact on communities and health systems
Lastly, there is also some evidence that SAHPE benefits local rural communities from having students being based there longitudinally. Just having a SAHPE institution in underserved areas means they are often providing health services where there were none before, with students supporting the local health system while on community placement (Omotara et al. Citation2004; Cristobal & Worley Citation2012; Hudson et al. Citation2012; Talib et al. Citation2013). Evidence also shows having a long-term engagement with the same student is valued by patients (Hudson et al. Citation2012), while further evidence suggests that orientating student learning around local community needs with a service component develops a health professional workforce able to meet local needs, which can impact positively on community health (Reid et al. Citation2011; Talib et al. Citation2013; Mohamed et al. Citation2014). Indeed, in the Philippine region covered by ADZU-SOM, the under-five mortality has dropped from 89 per 1000 live births to just 8 per 1000 since the school’s graduates first went to work in the region over 15 years ago (Cristobal & Worley Citation2012). While these statistics are very promising, attributing health and workforce outcomes to medical school interventions is notoriously difficult due to the multiple complex factors involved in improving health outcomes, and the inability of descriptive studies to prove causality.
Conclusions
The evidence presented in this review suggests longitudinal placements in underserved areas with a service learning approach have an effective and beneficial effect on medical student learning and attitudes towards serving local communities. In addition, these experiences and activities can increase student desire for practice and/or community service in underserved rural areas with implications for increased rural health workforce in the longer term.
Several studies further suggest health profession schools which take a socially-accountable approach (SAHPE) – including having an equitable selection process for admitting rural applicants and applicants from underserved sub-populations, a curriculum that makes it mandatory for students to be placed for extensive periods (20+ weeks) in rural communities, and to undertake preventative health projects targeting priority health issues of local communities – have additional positive impacts on graduate competencies, local health systems, and the health of the local people.
However, as there is a relative paucity of published literature around the impact of SAHPE on rural health workforce, local communities and population health outcomes, the authors are currently addressing this deficiency through more detailed case studies and descriptive studies of the SAHPE institutions that comprise THEnet organization, beginning with the two Philippines health profession schools described in this literature review.
Notes on contributors
Dr Carole Reeve, PhD, is a rural general practitioner and public health physician involved in health service and education research in rural and remote areas. Her research and teaching interests are around research translation to improve health equity in disadvantaged populations.
Dr Torres Woolley, PhD, is the Evaluation Coordinator for the JCU College of Medicine & Dentistry. Torres has been an active researcher for 20 years using both quantitative and qualitative methodologies, and is experienced in a range of research and evaluation methods, analyses and software.
Simone J. Ross, BPsych, MDR, is the Project Manager for the Training for Health Equity Network, and Lecturer and PhD candidate in General Practice and Rural Medicine, College of Medicine and Dentistry, James Cook University.
Leila Mohammadi, Masters in Medical Library and Information Studies, is a Medical Librarian at Flinders University and an expert in teaching rigorous search strategy construction for systematic reviews and Evidence Based Practice in Healthcare. Her research interests are Evidence Based Medicine curriculum, knowledge translation and online learning.
Servando “Ben” Halili, Jr., PhD, teaches research and culture studies at the Ateneo de Zamboanga University, Zamboanga City, Philippines. He is a Fulbright Research Fellow and is currently on fellowship at the Foundation for the Advancement of International Education and Research (FAIMER) in Philadelphia.
Dr Fortunato Cristobal, MD, MPH, a pediatric gastroenterologist is the founding dean of the Ateneo de Zamboanga University School of Medicine. Since 1993, he has worked to develop a medical curriculum that is locally-relevant and community engaged. He is also founding member of the board of the Training for Health Equity Network.
Jusie Lydia J. Siega-Sur, RN, MHPEd, is an Associate Professor and was Dean of the University of the Philippines Manila-School of Health Sciences from 2006 to 2010.
Dr. A.-J. Neusy, MD, DTM&H, is a retired Professor of Medicine at New York University School of Medicine. He co-founded the Training for Health Equity Network (THEnet) in 2008. He is currently THEnet’s Senior Advisor and a visiting professor in several universities around the world. His work focuses on health workforce and institutional development.
Reeve_et_al._supplemental_content.docx
Download MS Word (20.3 KB)Acknowledgments
We would like to thank and acknowledge comments from: Sarah Larkins, Amy Clithero, Paul Worley, Roger Strasser from THEnet.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
Funding
This work was supported by the Atlantic Philanthropies who have funded the Training for Health Equity Network (THEnet; Grant number 0003), via Resources for Health Equity, to conduct an impact study of SAPHE in the Philippines (www.atlanticphilanthropies.org/grantees/resources-for-health-equity).
References
- Amalba A, van Mook WN, Mogre V, Scherpbier AJ. 2016. The perceived usefulness of community based education and service (COBES) regarding students’ rural workplace choices. BMC Med Educ. 16:1.
- Boelen C, Heck J. 1995. Defining and Measuring the Social Accountability of Medical Schools [Internet]; No. WHO/HRH/95.7 Unpublished; Geneva: World Health Organisation; [cited 2015 Oct 22]. Available from: http://www.who.int/iris/handle/10665/59441.
- Birden H, Page S. 2007. 21st Century medical education. Austral. Health Rev. 31:341–350.
- Birden HH, Wilson I. 2012. Rural placements are effective for teaching medicine in Australia: evaluation of a cohort of students studying in rural placements. Rural Remote Health. 12:2167.
- Chang LW, Kaye D, Muhwezi WW, Nabirye RC, Mbalinda S, Okullo I, Groves S, Kennedy CE, Bollinger RC, Sisson S, Burnham G. 2011. Perceptions and evaluation of a community-based education and service (COBES) program in Uganda. Med Teach. 33:e9–e15.
- Couper I, Worley PS, Strasser R. 2011. Rural longitudinal integrated clerkships: lessons from two programs on different continents. Rural Remote Health. 11:1665.
- Cristobal F, Worley PS. 2011. Transforming health professional’s education. Lancet. 377:1235–1236.
- Cristobal F, Worley P. 2012. Can medical education in poor rural areas be cost-effective and sustainable: the case of the Ateneo de Zamboanga University School of Medicine. Rural Remote Health. 12:1835.
- Deans T. 1999. Service-learning in two keys: Paulo Freire’s critical pedagogy in relation to John Dewey’s pragmatism. Michigan J Commun Service Learn. 6:15–29.
- Dussault G, and Franceschini MC. 2006. Not enough there, too many here: understanding geographical imbalances in the distribution of the health workforce. Human Resour Health. 4:12.
- Easterbrook M, Goodwin M, Wilson R, Hodgetts G, Brown G, Pong R, Najgebauer E. 1999. Rural background and clinical rural rotations during medical training: effect on practice location Can Med Assoc J. 160:1159–1163.
- Elsanousi S, Elsanousi M, Khalafallah O, Habour A. 2016. Assessment of the social accountability of the faculty of medicine at University of Gezira, Sudan/Évaluation de la redevabilité sociale de la Faculté de médecine de l'Université de Gezira, Soudan. Eastern Mediterranean Health J. 22:258.
- Frenk J, Chen L, Bhutta ZA, Cohen J, Crisp N, Evans T, Fineberg H, Garcia P, Ke Y, Kelley P, Kistnasamy B. 2010. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. 376:1923–1958.
- Heng D, Pong R, Chan B, Degani N, Crichton T, Goertzen J, McCready W, Rourke J. 2007. Graduates of northern Ontario family medicine programs practise where they train. Can J Rural Med. 3:146–152.
- Howe A. 2001. Patient-centered medicine through student-centered teaching: a student perspective on the key impacts of community-based learning in undergraduate medical education. Med Educ. 35:666–672.
- Howe A, Ives G. 2001. Does community-based experience alter career preference? New evidence from a prospective longitudinal cohort study of undergraduate medical students. Med Educ. 35:391–397.
- Hudson JN, Knight PJ, Weston KM. 2012. Patient perceptions of innovative longitudinal integrated clerkships based in regional, rural and remote primary care: a qualitative study. BMC Fam Pract. 13:72.
- Iputo JE. 2008. Faculty of health sciences, Walter Sisulu University: training doctors from and for rural South African communities. MEDICC Rev. 10:25–29.
- Iputo JE, Kwizera E. 2005. Problem-based learning improves the academic performance of medical students in South Africa. Med Educ. 39:388–393.
- Jinadu MK, Ojofeitimi EO, Oribabor P. 2002. Evaluation of an innovative approach to community-based medical undergraduate education in Nigeria. Educ Health. 15:139–148.
- Larkins S, Preston R, Matte M, Lindemann IC, Samson R, Tandinco FD, Buso D, Ross SJ, Pálsdóttir B, Neusy AJ, Training for Health Equity Network Thenet. 2013. Measuring social accountability in health professional education: development and international pilot testing of an evaluation framework. Med Teach. 35:32–45.
- Lehmann U, Dieleman M, Martineau T. 2008. Staffing remote rural areas in middle-and-low-income countries: a literature review of attraction and retention. BMC Health Serv Res. 8:19.
- Lenthall S, Wakerman J, Knight S. 2009. The frontline and the ivory tower: a case study of service and professional-driven curriculum. Austr J Rural Health. 17:129–133.
- Lyon PM, McLean R, Hyde S, Hendry G. 2008. Students’ perceptions of clinical attachments across rural and metropolitan settings. Assess Eval High Educ. 33:63–73.
- Mafigiri DK, Ayebare F, Baingana R, Okello E, Sewankambo N. 2014. Medical education for equitable services for all Ugandans (MESAU) consortium: development and achievement. Acad Med. 89:S65–S68.
- Magzoub, ME, Schmidt HG. 2000. A taxonomy of Community-based Medical Education. Academic Medicine. 75:699–707.
- McLean RG, Pallant J, Cunningham C, DeWitt DE. 2010. A multiuniversity evaluation of the rural clinical school experience of Australian medical students. Rural Remote Health. 10:1492.
- Mohamed KG, Hunskaar S, Abdelrahman SH, Malik EM. 2014. Scaling up family medicine training in Gezira, Sudan – a 2-year in-service master programme using modern information and communication technology: a survey study. Hum Resour Health. 12:1.
- Moher D, Liberati A, Tetzlaff J, Altman DG. 2009. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals Intern Med. 151:264–269.
- Okayama M, Kajii E. 2011. Does community-based education increase students’ motivation to practice community health care? – a cross sectional study. BMC Med Educ. 11:19.
- Omotara BA, Padonu MO, Yahya SJ. 2004. Assessment of the impact of community-based medical education of the University of Maiduguri on communities in three local government areas of Borno State, Nigeria: community leaders’ perspectives. Educ Health. 17:6–16.
- Palsdottir B, Neusy A, Reed G. 2008. Building the evidence base: networking innovative socially accountable medical education programs. Educr Health. 8:177.
- Preston R, Larkins S, Taylor J, Judd J. 2016. From personal to global: understandings of social accountability from stakeholders at four medical schools. Med Teach. 38:987–994.
- Rahim IMD, Mustafa AE, Ahmed BO. 1992. Performance evaluation of graduates from a community-based curriculum: the housemanship period at Gezira. Med Educ. 26:233–240.
- Reid SJ, Couper ID, Volminik J. 2011. Educational factors that influence the urban-rural distribution of health professionals in South Africa: a case-control study. South African Med J. 100:29–33.
- Ross SJ, Preston R, Lindemann IC, Matte MC, Samson R, Tandinco FD, Larkins SL, Palsdottir B, Neusy AJ. 2014. The training for health equity network evaluation framework: a pilot study at five health professional schools. Educ Health. 27:116–126.
- Satran L, Harris IB, Allen S, Anderson DC, Poland GA, Miller WL. 1993. Hospital-based versus community-based clinical education: comparing performances and course evaluations by students in their second-year Pediatrics rotation. Acad Med. 68:380–382.
- Sen Gupta T, Woolley T, Murray R, Hays R, McCloskey T. 2014. Positive impacts on rural and regional workforce from the first seven cohorts of James Cook University medical graduates. RRHJ. 14:2657.
- Seifer SD. 1998. Service-learning: community-campus partnerships for health professions education. Acad Med. 73:273–277.
- Strasser R, Hogenbirk JC, Minore B, Marsh DC, Berry S, McCready WG, Graves L. 2013. Transforming health professional education through social accountability: Canada's Northern Ontario School of Medicine. Med Teach. 35:490–496.
- Strasser R, Worley P, Cristobal F, Marsh DC, Berry S, Strasser S, Ellaway R. 2015. Putting communities in the driver's seat: the realities of community-engaged medical education. Acad Med. 90:1466–1470.
- Talib ZM, Baingana RK, Sagay AS, van Schalkwyk SC, Mehtsun S, Kiguli-Malwadde E. 2013. Investing in community-based education to improve the quality, quantity and retention of physicians in three African countries. Educ Health. 26:109–113.
- Thomas L. 2001. Power, assumptions and prescriptions: a critique of widening participation policy-making. High Educ Policy. 14:361–377.
- WHO. 2010. Increasing access to health workers in remote and rural areas through improved retention: global policy recommendations. Geneva: World Health Organization.
- Worley P, Esterman A, Prideaux D. 2004a. Cohort study of examination performance of undergraduate medical students learning in community settings. BMJ. 328:207–209.
- Worley PS, Strasser R, Prideaux D. 2004b. Can medical students learn specialist disciplines based in rural practice: lessons from students’ self-reported experience and competence. Rural Remote Health. 4:338.

