Abstract
Team-based learning (TBL) is a structured form of small group learning that can be scaled up for delivery in large classes. The principles of successful TBL implementation are well established. TBL has become widely practiced in medical schools, but its use is typically limited to certain courses or parts of courses. Implementing TBL on a large scale, across different courses and disciplines, is the next logical step. The Lee Kong Chian School of Medicine (LKCMedicine), a partnership between Nanyang Technological University, Singapore and Imperial College London, admitted its first students in 2013. This new undergraduate medical program, developed collaboratively by faculty at both institutions, uses TBL as its main learning and teaching strategy, replacing all face-to-face lectures. TBL accounts for over 60% of the curriculum in the first two years, and there is continued learning through TBL during campus teaching in the remaining years. This paper describes our experience of rolling out TBL across all years of the medical curriculum, focusing on three success factors: (1) “team-centric” learning spaces, to foster active, collaborative learning; (2) an e-learning ecosystem, seamlessly integrated to support all phases of the TBL process and (3) teaching teams in which experts in pedagogical process (TBL Facilitators) co-teach with experts in subject matter (Content Experts).
Introduction
In this paper, we describe the background to TBL and its principles, our experience of developing a new TBL curriculum for delivery across all years of an undergraduate medical program and three key developments that have contributed to the success and sustainability of our approach.
Team-based learning (TBL) is a structured form of small group learning that can be scaled up for implementation in large classes. First developed by Larry Michaelsen in the 1970 s for use in graduate business education (Michaelsen et al. Citation2004), TBL has been widely adopted as an instructional approach across many disciplines (Parmelee and Hudes Citation2012). In a systematic review of TBL research in health professionals education, the majority of published studies showed a positive effect of TBL in two areas compared to traditional lectures; (1) teacher and learner experiences and attitudes and (2) academic achievement in graded assessments (Reimschisel et al. Citation2017). The principles of TBL including its core design elements are well defined (Haidet et al. Citation2012), as are guidelines for its implementation (Parmelee et al. Citation2012). However, a systematic review of TBL implementation found that in medical schools practicing TBL, its use was generally limited to a few sessions of a single course (Burgess et al. Citation2014).
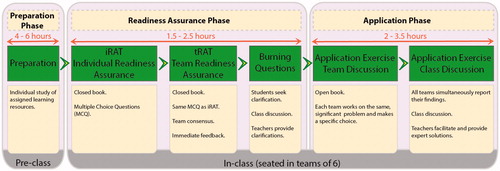
The TBL process consists of three phases. In the preparation phase, individual learning is undertaken before class. Learning resources may include journal articles, videos or voiceover PowerPoints. The subsequent phases occur in class during which students are seated in teams. Teams typically number between 5 and 7 and team composition should remain fixed for an extended period (Parmelee et al. Citation2012).
The second phase is readiness assurance, where the intention is to ascertain whether students have acquired sufficient understanding of the subject studied and to provide clarifications where necessary. This starts with an individual closed book knowledge test, in single best answer multiple-choice question (MCQ) format (Individual Readiness Assurance Test or iRAT). Students then repeat the same closed book test, but this time in their assigned teams (Team Readiness Assurance Test or tRAT). During the tRAT students discuss and come to a consensus on their team answers. Once the team has committed to an answer the correct answer is revealed, providing them with immediate feedback. This form of peer learning enables misconceptions to be clarified and knowledge gaps to be filled. Often the small group discussion leads to additional questions about the subject matter, which can then be discussed classwide or posed to the teacher who provides the necessary clarifications.
In the third and final application exercise phase, students working in their teams are tasked with scenarios – usually clinical problems or cases – that encourage them to apply what they have learned in the previous stages of TBL. These application exercises are undertaken in open book conditions and characterized by the “4S” principle (Michaelsen et al. Citation2009). All student teams discuss the “same” problem, which must be “significant”. Each team’s response requires a “specific” choice reflecting the team‘s consensus. During the second part of the application exercise phase, teams report their choices “simultaneously”. Teams then participate in a classwide discussion that the teacher facilitates. At the end of the class discussion, the teacher may provide an expert’s solution when necessary. In order to aid simultaneous reporting, application exercises are often single best answer MCQs or short answer questions.
TBL has similarities with problem-based learning (PBL), another widely implemented instructional approach in medical education. Both approaches are based on constructivist learning theory, involve active learning in small groups and make use of professionally relevant problems. However, TBL is distinct in its requirement for preclass preparation, its sequence of in-class individual and team activities, its higher student-teacher ratio, and the way it combines peer learning with immediate feedback and expert clarification (Dolmans et al. Citation2015).
Developing a new team-based learning curriculum
The Lee Kong Chian School of Medicine (LKCMedicine) is Singapore’s newest medical school. A partnership between Nanyang Technological University, Singapore (NTU Singapore) and Imperial College London (Imperial), its first cohort of students was admitted in 2013. The bespoke curriculum was developed jointly by faculty from both institutions, with some elements of the Imperial curriculum adapted and contextualized for Singapore and other elements developed de novo. The program was planned as an integrated systems-based curriculum, with a focus on clinical presentations throughout. In keeping with modern educational practice, a decision was taken to move away from strict memorization of didactic materials and instead adopt principles of active learning with an emphasis on teamwork and application of knowledge (Partridge Citation2013). TBL was established as the School’s principle classroom learning and teaching strategy across all years of the five-year program, dispensing with face-to-face lectures.
In years 1 and 2 around 60% of curriculum time is dedicated to TBL, equating to around 140 TBL class days (two full days of TBL plus two half days of preparation per week). The focus of these TBL classes is the development of foundational scientific understanding, with the application exercises providing a means to contextualize the science to clinical presentations and clinical practice. In years 3, 4 and 5, learning is primarily practice-based in clinical settings. Students do however regroup for campus teaching during which TBL classes provide a means to link clinical presentations with medical decision-making (diagnostic reasoning, management plans), potentially involving multiple disciplines. Across all year groups, cross-cutting courses such as professionalism, ethics, patient safety, pathology and pharmacology are learned through TBL.
An overview of the TBL process at LKCMedicine, with the average time spent in each phase, is shown in . Each TBL session is assigned approximately 4 to 6 hours of scheduled time in the preparation phase, 1.5 to 2.5 hours in the readiness assurance phase and 2 to 3.5 hours in the application phase. The process follows established guidelines (Parmelee and Hudes Citation2012), although we have incorporated an additional step at the end of the readiness assurance phase known as “burning questions” where students are encouraged to submit questions with the intention of having their misunderstandings or uncertainties clarified. In keeping with TBL guidelines, students are in teams of six and team composition changes annually.
The medical school is now in its fifth year of operation and student enrollment is growing year-on-year. The annual student intake has increased from 54 in 2013 to 120 currently.
Key developments
In planning delivery of the new TBL curriculum we were keen to optimize the learning environment for the students, mindful that TBL would be extensively practiced by faculty from different professional backgrounds, in different courses and across all year groups. We were also aware that class sizes might increase to 200 or more. How could we ensure sustainability of the program and minimize the risk of pedagogical “drift”? To this end, we conceived three key approaches: (1) team-centric learning spaces (2) an integrated e-learning ecosystem customized to support the TBL process and (3) teaching teams in every class. These are described below.
Team centric learning spaces
Many institutions planning a new curriculum for TBL (or other large group active learning method) are obliged to adapt existing conventional learning spaces, usually lecture theaters. However, we had the opportunity, starting from scratch, to design spaces bespoke for large TBL classes. For this reason, a decision was taken to forgo conventional lecture theaters and seminar rooms and instead opt for team-centric learning spaces, designed to optimize communication both within and between teams. The architectural principles and human factors underpinning the design of active learning spaces have been well documented (Oblinger and Lippincott Citation2006). Although research specific to TBL is still somewhat limited, there is evidence that students’ attitudes toward TBL improve with greater comfort and physical ease of communication (Espey Citation2008).
One of the School’s learning studios is shown in . It can accommodate up to 264 people (44 teams of six individuals). The design has been conceptualize to enable small groups seated at round tables to engage in active intra-team discussions. Discussions between teams and with faculty are facilitated by microphones in the center of each table. Wifi connectivity allows students to wirelessly project relevant information and resources to large highly visible projection screens hung around the room. Despite its large size (620m2), the circular design of the TBL Learning Studio and its dual tiered seating arrangement, enable students to see each other and have at least two screens from wherever they are seated in view.
The value of a collaborative approach to designing physical learning spaces and ensuring their alignment with curriculum is well recognized (Nordquist et al. Citation2016). Our commitment to TBL early in the design process and the effective collaboration between faculty, academic leadership, facilities management and architects has transformed the tradition role of a large space for instruction to one that is closely aligned with TBL, providing an engaging environment that is conducive to active, collaborative learning.
Integrated eLearning ecosystem
Aligned with the vision of a student-centric curriculum we wanted to establish an e-learning ecosystem that would provide seamless support during all aspects of the student learning experience, including the spectrum of activities associated with TBL (Gagnon et al. Citation2017). The LKCMedicine eLearning ecosystem was developed using a design-based research approach (Reeves et al. Citation2005). A mobile app (iStudent) provides access to all timetabled activities, associated learning outcomes and resources. During the preparation phase of TBL, students review the expected learning outcomes and retrieve the relevant learning resources.
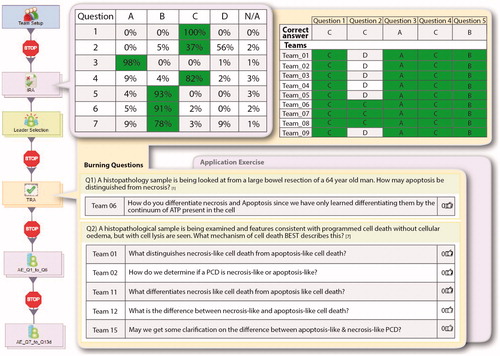
Once in class, the sequence of activities is managed and delivered digitally via a learning activity management system (iLAMS). This enables students to complete the TBL assessments (iRAT, tRAT and application exercises) and ensures that correct responses are revealed to the student teams at the appropriate time. In addition, following the readiness assurance phase of TBL, students are encouraged to submit any remaining queries as “burning questions”. A key feature of iLAMS is the provision of real-time access by faculty to student performance data, including individual (iRAT), team (tRAT, application exercises) and “burning questions”. These data are linked dynamically to a customized dashboard. This is shown in .
The dashboard enables faculty to (i) instantly view student performance (individual and team), (ii) to identify knowledge gaps that are most relevant to the class as a whole (iii) review burning questions arising from tRAT activities and (iv) provide timely focused support during the class. Outside the classroom, this expanding database of student performance data is monitored over time and used in a number of ways (discussed further in Lessons Learned).
Team teaching
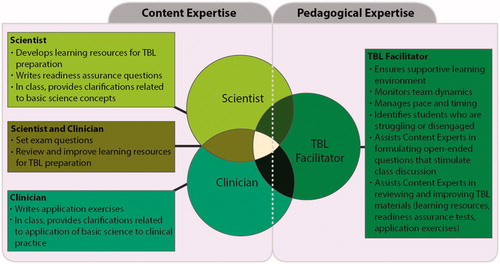
A key initiative in the early development of the School was faculty recruitment for the purpose of curriculum development and teaching. A willingness to engage with, and be trained in, TBL was a prerequisite for joining the School, and experts in TBL pedagogy were recruited to provide the necessary expertise. How could we ensure that so many scientists and clinicians from a variety of different disciplines had the necessary skills to facilitate their TBL sessions? Almost 20 years ago, Harden and Crosby (Citation2000) proposed a theoretical framework identifying 12 teaching roles of future medical teachers. These diverse roles included facilitator, information provider and resource developer. In the context of TBL, the role of “facilitator”, “information provider” and “resource developer” are commonly combined, despite the disparate skill set required. At LKCMedicine, a decision was made that the role of TBL Facilitator would be separated from that of “information provider” and “resource developer”, with the latter roles enacted by a Content Expert. Every class is co-taught by one or more Content Experts who provide subject matter expertise, and a TBL Facilitator who manages productive student discussions and provides the necessary pedagogical expertise. This approach ensures that while the class content is delivered and clarified by at least one Content Expert, constructivist pedagogical practices (Fosnot and Stewart Citation2005) are put in place by the Facilitator, as the “pedagogical process expert”. Furthermore, a particular Content Expert may contribute to only one or two TBL classes every year, whereas each TBL Facilitator is assigned a minimum of 15 TBL classes per year. This ensures that the Facilitators are able to build a relationship with the students over time.
The contrasting roles of the Content Experts and Facilitators are reinforced during faculty training workshops. The Facilitator optimizes the TBL process by ensuring, that students are held accountable for their responses, that student teams respond to one another, and that students have exhausted their propensity to answer before approaching the Content Expert for the best response. Facilitators are skilled at expressing questions at the appropriate level for the students. They are also able to clarify questions posed by Content Experts, many of whom are unaccustomed to formulating extempore questions verbally during a lesson. The Facilitator’s student-centered classroom management skills require an expert understanding of learning and teaching principles as well as significant experience of facilitation. Content Experts are briefed during faculty training to avoid being overly didactic, to encourage students to think critically about the topics and not to disclose the correct answer to students too quickly.
In addition to the Content Expert – Facilitator teaching team, there may be more than one Content Expert present in class. For example, in the early “preclinical” years, there may be two Content Experts; a scientist who takes responsibility for teaching the basic science content while a clinician explains how the scientific concepts are applied in clinical contexts. In the clinical years, the Content Expert would commonly be a clinician. However, clinicians from different specialties may co-teach in order to provide an interdisciplinary perspective on the management of a particular clinical presentation or problem.
Based on experience of TBL at LKCMedicine, a model for team teaching roles is shown in , using Year 1 as an example. Of note, Content Experts have multiple roles outside the classroom (e.g., developing learning resources for TBL preparation, writing application exercises, setting examination questions) as well as within the classroom. By its very nature, “team teaching” requires shared decision-making and compromise. This is evident in the interactions between Facilitator and Content Expert and – in classes where more than one Content Expert is present – between Content Experts of different professional or specialty backgrounds. An added benefit of the ‘team teaching’ approach is that it demonstrates to students that teachers can also work together in teams to promote a student-centric learning environment.
Lessons learned
Since LKCMedicine admitted its first cohort of students in 2013, TBL has remained the School’s main classroom learning and teaching strategy. Our team-centric learning spaces, e-learning ecosystem and “team teaching” have characterized the way we deliver TBL to expanding cohorts across all years of the curriculum. Our pedagogical approach to TBL has remained consistent over time. As a young school, it is too early to demonstrate definitive evidence of TBL’s success; however, early indicators are positive; our students and faculty remain highly engaged with the TBL process. Student attendance at TBL classes is over 95% and students come to class prepared. Students’ iRAT scores are highly predictive of examination success. A number of lessons have been learned that are of particular relevance to large scale implementation of TBL. These are highlighted below.
Central co-ordination of TBL
A fully digitalized TBL curriculum and consistent adherence to the principles of TBL benefit from central management and co-ordination by academic and administrative staff. Linked with this is the need for a rigorous faculty development program, encompassing training in TBL. While it could be argued that a TBL program consistently delivered according to established principles might stifle the creativity of individual faculty, including those who are passionate about teaching but wish to explore alternative innovative approaches, we believe that this consideration is outweighed by the benefits to students of a consistently applied evidence-based, student-centric pedagogy. Furthermore, it is our experience that committed educators, even those who are initially skeptical, will generally become engaged and value being part of the teaching team.
Ensuring the curriculum remains up to date
One of the challenges of any curriculum, particularly in an undergraduate medical program, is ensuring it remains up to date and responsive to student and faculty feedback. While our e-learning system has an effective way of capturing feedback in a timely manner and reporting responses back to students, changes to a digitalized curriculum are time-consuming to make. Furthermore, in the context of TBL any changes to learning outcomes may impact not only TBL preparation materials (e.g., voiceover PowerPoints), but also in-class assessments (readiness assurance tests and application exercises). A digitalized TBL curriculum requires adequate resources to ensure its sustainability and benefits substantively from an effective curriculum mapping capability.
Student performance data
In addition to being used in real-time during TBL classes, we have been impressed by the added value of TBL performance data (iRAT, tRAT, application exercises) outside the classroom. These data are used in a number of ways. Firstly, in years 1 and 2, they act as an “early warning” system for students or teams who may be in difficulty. A School committee meets on a monthly basis to identify underperforming students so that appropriate remediation and/or welfare support can be offered. Secondly, these data are used to inform quality improvement of the curriculum. For instance, a topic area for which student performance is consistently poor may indicate a need to improve certain learning resources, refocus learning outcomes or improve the quality of TBL assessments. A review of “burning questions” related to the same topic may provide additional data to inform improvements. Finally, the data provide a rich source of information that can be correlated with other performance data (e.g., admissions, examinations) to inform program evaluation.
TBL research
With TBL practiced so consistently and with extensive amounts of student performance data captured on a routine basis, we have a unique opportunity to study TBL in more comprehensive ways than has been done before. We have taken first steps in this direction and initiated a formal research program on TBL, in which we have started to examine how cognitively engaged students are during the different phases of TBL (Rotgans et al. Citation2017), how the role of Facilitators and Content Experts affect student learning, and which psychological factors in TBL are responsible for arousing and sustaining student interest in the topics we teach (Ahn et al. Citation2017).
Relevance to broader medical education community
We acknowledge that as a well-resourced medical school and starting afresh we had the opportunity to introduce innovations that may not be feasible for some schools or for individual faculty implementing TBL in their own courses. However, there are elements that could be adapted for smaller scale implementation of our approach. Take for example the design of our team centric learning spaces; a key aspect of which is the small round tables and accompanying chairs which were specifically configured for TBL groups. This design can be easily and cost effectively transferred to smaller scale implementations to fit within many existing classrooms.
We also recognize that TBL is but one effective active learning strategy, We believe that the initiatives that have helped us achieve success are also applicable to other active teaching and learning methods delivered on a large scale. However, for teaching teams to be effective and for e-learning systems to be aligned, medical programs must adopt a common learning and teaching strategy.
Conclusions
Every few years in medical education the suggestion is made to abandon lectures and move towards more evidence-based teaching approaches (Prober and Heath Citation2012; Schwartzstein and Roberts Citation2017). While these approaches can be challenging to implement across multiple courses and disciplines, from our experience of introducing a new TBL curriculum on a large scale, we have identified three key factors – bespoke learning spaces, integrated e-learning systems and team-teaching approach – that have been instrumental in achieving success.
Acknowledgements
The authors would like to acknowledge Li Meihui for assistance on the graphic design of the figures.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
Additional information
Notes on contributors
Preman Rajalingam
Preman Rajalingam, PhD, is a Senior Lecturer in Medical Education and Lead for Educational Development and TBL Facilitation at the Lee Kong Chian School of Medicine.
Jerome I. Rotgans
Jerome I. Rotgans, PhD, is an Assistant Professor of Medical Education Research at the Lee Kong Chian School of Medicine and adjunct Associate Professor at Erasmus MC.
Nabil Zary
Nabil Zary, PhD, is an Acting Director of the Medical Education Research and Scholarship Unit (MERSU) at the Lee Kong Chian School of Medicine and Technical Director of the Games for Health Innovations Centre (ALIVE), Singapore.
Michael Alan Ferenczi
Michael Alan Ferenczi, PhD, is an Assistant Dean, Years 1 & 2 and Vice-Dean, Faculty Affairs the Lee Kong Chian School of Medicine.
Paul Gagnon
Paul Gagnon, MEd, is the Director of E-Learning and Instructional Systems and Services at the Lee Kong Chian School of Medicine.
Naomi Low-Beer
Naomi Low-Beer, MBBS, MD, MEd, is the Vice-Dean (Education) at the Lee Kong Chian School of Medicine.
References
- Ahn HS, Rotgans JI, Rajalingam P, Lee JJR, Koh YYJ, Low-Beer N. 2017. Assessing how students learn in team-based learning: validation of the knowledge re-consolidation inventory. Health Prof Educ. 3:118–127.
- Burgess AW, McGregor DM, Mellis CM. 2014. Applying established guidelines to team-based learning programs in medical schools. Acad Med. 89:678–688.
- Dolmans D, Michaelsen L, van Merriënboer J, van der Vleuten C. 2015. Should we choose between problem-based learning and team-based learning? No, combine the best of both worlds! Med Teac. 37:354–359.
- Espey M. 2008. Does space matter? Classroom design and team-based learning. Rev Agri Econ. 30:764–775.
- Fosnot C, Stewart R. 2005. Constructivism: a psychological theory of learning. In: Fosnot CT, editors. Constructivism, theory, perspectives and practice. New York: Teachers College Press; p. 8–38.
- Gagnon P, Mendoza R, Carlstedt-Duke J. 2017. A technology-enabled flipped classroom model. In: The flipped classroom. Singapore: Springer Singapore; p. 211–228.
- Haidet P, Levine RE, Parmelee DX, Crow S, Kennedy F, Kelly PA, Perkowski L, Michaelsen L, Richards BF. 2012. Perspective: guidelines for reporting team-based learning activities in the medical and health sciences education literature. Acad Med. 87:292–299.
- Harden RM, Crosby J. 2000. AMEE Guide No 20: the good teacher is more than a lecturer-the twelve roles of the teacher. Med Teach. 22:334–347.
- Michaelsen LK, Knight AB, Fink LD. 2004. Team-based learning: a transformative use of small groups in college teaching. 1st ed. Westport (CT): Greenwood publishing group.
- Michaelsen LK, Sweet M, Parmelee DX. 2009. Team-based learning: Small group learning’s next big step. San Francisco (CA): Jossey-Bass.
- Nordquist J, Sundberg K, Laing A. 2016. Aligning physical learning spaces with the curriculum: AMEE Guide No. 107. Med Teach. 38:755–768.
- Oblinger D, Lippincott J. 2006. Learning spaces (c2006. 1 v). Boulder (CO): EDUCAUSE.
- Parmelee D, Hudes P. 2012. Team-based learning: a relevant strategy in health professionals’ education. Med Teach. 34:411–413.
- Parmelee D, Michaelsen LK, Cook S, Hudes PD. 2012. Team-based learning: a practical guide: AMEE Guide No. 65. Med Teach. 34:e275–e287.
- Partridge MR. 2013. Redefining medicine, transforming healthcare: the Lee Kong Chian school of medicine. Ann Acad Med Singapore. 42:165–167.
- Prober CG, Heath C. 2012. Lecture halls without lectures: a proposal for medical education. N Engl J Med. 366:1657–1659.
- Reeves TC, Herrington J, Oliver R. 2005. Design research: a socially responsible approach to instructional technology research in higher education. J Comput High Educ. 16:96–115.
- Reimschisel T, Herring AL, Huang J, Minor TJ. 2017. A systematic review of the published literature on team-based learning in health professions education. Med Teach. 39:1227–1237.
- Rotgans JI, Schmidt HG, Rajalingam P, Hao JWY, Canning CA, Ferenczi MA, Low-Beer N. 2017. How cognitive engagement fluctuates during a team-based learning session and how it predicts academic achievement. Adv Health Sci Educ. http://doi.org/10.1007/s10459-017-9801-2
- Schwartzstein RM, Roberts DH. 2017. Saying Goodbye to Lectures in Medical School — Paradigm Shift or Passing Fad? N Engl J Med. 377:605–607.