Abstract
Purpose
In daily practice, junior doctors can contribute to quality improvement by providing innovative suggestions for change, referred to as voice behavior. Junior doctors are more likely to engage in voice behavior when they receive sufficient support from supervisors and peers. Such support has also been associated with less burnout and more work engagement. However, whether less burned-out and more work-engaged junior doctors demonstrate more voice behaviors in the face of sufficient supervisor and peer support is unclear. Therefore, we studied whether and how associations of supervisor and peer support with junior doctors’ voice behaviors are mediated by burnout and work engagement.
Materials & methods
Participants were 301 junior doctors that completed a web-based survey including validated questionnaires on supervisor and peer support, burnout, work engagement, and voice behavior.
Results
Supervisor and peer support were associated with lower levels of burnout and higher levels of work engagement. Work engagement, but not burnout, mediated the associations of supervisor and peer support with voice behaviors.
Conclusions
Junior doctors who received more supervisor or peer support were more work-engaged and reported more voice behaviors. Thus, supervisor and peer support should be cultivated to facilitate junior doctors’ roles as work-engaged professionals in quality improvement.
Introduction
Worldwide, doctors who have recently graduated from medical school provide substantial parts of frontline care. They can observe signs of unsafe care at the frontline, as well as practices that could benefit from quality improvement (Roueche and Hewitt Citation2012; Lemer and Moss Citation2013). However, expressing one’s voice about such practices can be challenging for these new doctors; they may feel uncertain about whether suggestions for improvement will be appreciated or rejected by supervisors and other healthcare staff (Martinez et al. 2017; Voogt et al. Citation2020). Alarmingly, a lack of safety in suggesting quality improvement is experienced by doctors across postgraduate medical trajectories worldwide, ranging from interns and foundation doctors to residents and trainees – all of whom are referred to hereafter as junior doctors (Martinez et al. 2017; Voogt et al. Citation2020; Talash et al. Citation2022). Specifically, junior doctors fear rejection of their suggestions for change and negative effects on their performance assessments, and they are concerned about being labeled troublemakers who burden colleagues with the extra work necessary to achieve quality improvement (Voogt et al. Citation2020; Chen et al. Citation2022).
Practice points
Junior doctors report to demonstrate more voice behaviors when they are more work-engaged.
Junior doctors are more work-engaged and less burned-out when receiving more supervisor and peer support.
Supervisor and peer support should be cultivated to help reduce burnout among junior doctors, as well as to facilitate them in being work-engaged professionals who proactively voice their suggestions for quality improvement.
Junior doctors’ active involvement in quality improvement is however widely recognized, and this involvement is increasingly promoted in postgraduate medical education trajectories (Fishbain et al. Citation2019). Accordingly, these trajectories are also reviewed by programs (such as the Clinical Learning Environment Review program) on the criterium of creating a learning environment that facilitates junior doctors’ contribution to patient safety by proactively suggesting quality improvement (Fishbain et al. Citation2019; Kuhn et al. Citation2021). Suggesting quality improvement is referred to as voice behavior, involving the articulation of necessary improvements by providing innovative suggestions for change (Van Dyne and LePine Citation1998; Chen et al. Citation2022). Voice behavior is more likely demonstrated by junior doctors who receive sufficient support from supervisors (Parker et al. Citation2006; Gin et al. Citation2021). Supervisors who are approachable and show an open attitude to change support the voice behavior of junior doctors (Voogt et al. Citation2019; Citation2020). Such behavior is also facilitated by support from peers, which allows junior doctors to make stronger points when suggesting specific changes (Voogt et al. Citation2020).
Supervisor and peer support may thus benefit junior doctors’ voice behaviors, and such support can also promote junior doctor well-being (Prins et al. Citation2007; Abrams Citation2017). Specifically, supervisor and peer support helps junior doctors deal better with the stresses of daily medical practice, thereby facilitating the maintenance of their well-being (Hariharan and Griffin Citation2019). The well-being of junior doctors, which involves their physical, emotional, and occupational health (Shanafelt et al. Citation2003), has been studied widely from the perspective of burnout (Dyrbye et al. Citation2013). Burned-out junior doctors are exhausted, cynical, and less effective, and thus experience suboptimal well-being in their work (Maslach et al. Citation2001). On the other hand, junior doctors experience optimal well-being when they are engaged in their work; they are dedicated, energetic, and concentrated (Bakker Citation2011; van den Berg et al. Citation2017). The concepts of burnout and work engagement help to clarify why support facilitates voice behaviors, following the principles of the evidence-based Job Demands and Resources (JD-R) model (Bakker and Demerouti Citation2007).
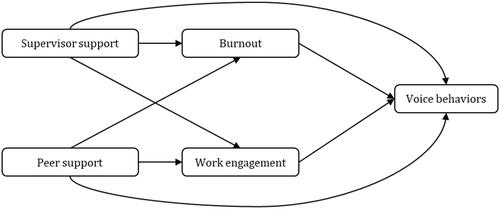
Research based on the JD-R model has shown that burnout and work engagement mediate the association between support and performance; professionals perceiving more support are less burned out and more work engaged, and thereby better able to perform well in their work (Bakker Citation2011; van den Berg et al. Citation2017; Hariharan and Griffin Citation2019). Junior doctors’ performance is reflected by diverse clinical and interpersonal behaviors; voice behaviors illustrate this performance in the domain of quality improvement (Rethans et al. Citation2002). However, little is known about how junior doctors’ voice behaviors are affected by supervisor and peer support, burnout, and work engagement. One study showed that supervisor support affected voice behaviors, while work engagement did not, but the roles of peer support and burnout were not clarified (Voogt et al. Citation2019). Continued research on this topic will provide insight into whether and how supervisor and peer support can help junior doctors become less burned-out and more work-engaged professionals who proactively voice their suggestions for quality improvement. Thus, we studied how supervisor and peer support are associated with voice behaviors, and whether this association is mediated by burnout and work engagement, among junior doctors (see ).
Materials & methods
Study setting and population
This observational study was conducted from 5 February to 17 April 2020, in collaboration with the Young Doctor foundation in the Netherlands – a federation for junior doctors who have not (yet) been selected for postgraduate medical training (e.g. a medical specialty). In the Dutch health care system, recently graduated doctors commonly act as frontline care providers under the supervision of medical specialists or consultants before receiving postgraduate medical training. In other countries, such doctors are referred to as interns, foundation doctors, and senior house officers. Participation was anonymous and voluntary, and respondents provided informed consent at the start of the survey. Ethical approval for this study was waived by the Medical Ethics Committee of the Amsterdam University Medical Centers on 16 April 2020 (reference number W20_152 # 20.191).
Data collection
For this study, the Young Doctor Foundation invited junior doctors to participate in a web-based survey based on convenience and snowball sampling, i.e. through its website and social media (LinkedIn, Facebook, and WhatsApp), as well as by sending emails to contacts in 2 academic and 14 nonacademic hospitals and 7 committees for interns with the request to distribute the survey to the junior doctor staff. The measurements for the survey were selected by the research team, including well-validated instruments for supervisor and peer support, burnout, work engagement, and voice behavior. The survey was first pilot tested by junior doctors of the Young Doctor Foundation and the research team regarding user friendliness and flow, after which the survey was disseminated.
Supervisor and peer support were measured with the support scale of the JD-R questionnaire (Bakker Citation2014; Khan et al. Citation2018). This scale consists of three items (see Supplementary file) to which responses are provided on a 5-point Likert scale from 1 (“never”) to 5 (“always”). Participants responded to these items separately for supervisor and peer support. Two researchers independently translated the English scale to Dutch using the forward-and-back translation method.
Work engagement was measured with the validated nine-item Utrecht Work Engagement Scale (see Supplementary file) (Seppälä et al. Citation2009). Responses to the items are provided on a 7-point Likert scale from 1 (“never”) to 7 (“always – daily”).
Burnout was measured with the ‘work-related burnout’ subscale of the Copenhagen Burnout Inventory (see Supplementary file) (Kristensen et al. Citation2005). Responses to the subscale’s seven items are structured by 5-point Likert scales from 1 (“to a very low degree”) to 5 (“to a very high degree”) for three items; and from 1 (“never”) to 5, (“always”) for four items.
Voice behavior was measured with the validated suggestion-focused voice behavior scale of Dyne and LePine (see Supplementary file) (Van Dyne and LePine Citation1998). This scale consists of six items to which responses are provided on a 7-point Likert scale from 1 (“disagree completely”) to 5 (“agree completely”).
Respondents were also asked to indicate the number of years that they had served as junior doctors (time since graduation), their work location (hospital or non-hospital setting), and whether they had a part-time or full-time contract.
Statistical analyses
Sample characteristics were represented using descriptive statistics. The reliability of the support, work engagement, burnout, and voice behavior scales was evaluated by assessing their internal consistency (satisfactory when Cronbach’s α > 0.70), factor loadings (satisfactory when >0.40), and the item–total correlations (satisfactory when Pearson’s r > 0.30). The multicollinearity of the supervisor and peer support scales was checked; variance inflation factor values <2.5 and tolerance values > 0.2 were taken to indicate a lack of multicollinearity.
We performed a mediation analysis to assess whether the associations of supervisor and peer support (independent variables) with voice behavior (dependent variable) were mediated by burnout and work engagement. The mediation analysis consisted of five steps, i.e. four regression analyses and one bootstrap analysis. For step 1, we conducted a regression analysis on the association between the independent variables (supervisor and peer support) and mediator burnout. Step 2 included a regression analysis of the association between the independent variables and the mediator work engagement. Step 3 involved conducting a regression analysis on the association between the independent variables and the dependent variable (voice behaviors). Step 4 was conducted by performing a regression analysis on how both the independent variables and mediators were associated with the dependent variable to detect mediating effects. Finally, for step 5 we conducted two bootstrap analyses with 5000 samples (one for each of the two mediators) to examine the indirect association between the independent and dependent variables through the mediators (burnout and work engagement). Significant indirect associations were considered to reflect mediation. The junior doctors’ years of experience, work location and type of contract (fulltime or parttime) served as covariates in the mediation analysis. In the mediation analyses missing data were handled through listwise deletion. The analyses were performed using IBM SPSS Statistics version 27 and PROCESS macro (model 4) for SPSS version 3.5.3.(Hayes Citation2017).
Results
In total, 497 junior doctors initially responded to the survey and 301 completed it (60.6% completion rate). The majority (81.1%) of participants had ≤2 years of experience as junior doctors and worked in hospital settings (81.8%), while a minority (18.2%) worked outside of hospitals (e.g. in community health centers and mental health care facilities). The support, work engagement, burnout, and voice behavior scales showed good internal consistency (0.80–0.91), adequate factor loadings (>0.40), and good item–total correlation (>0.30; Table 1, Supplementary file). These junior doctors reported average scores of 3.32 (SD = 0.84) and 3.96 (SD = 0.87) for supervisor and peer support, respectively; furthermore, they reported average scores of 2.33 (SD = 0.62) on burnout and 4.96 (SD = 0.95) on work engagement (Table 1, Supplementary file).
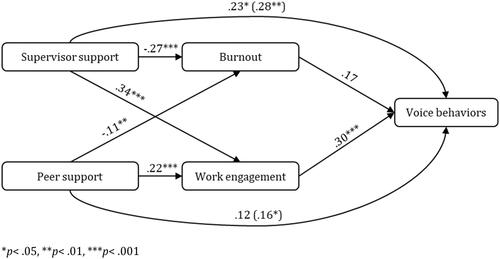
Following step 1 of the mediation analysis, we found both supervisor and peer support to be negatively associated with burnout (B = −.27, 95% CI = −.36, −.18, p< .001; B = −.11, 95% CI = −.20, −.03, p = .007, respectively) (Supplementary file, Table 2, Step 1 and ). Subsequently, step 2 of the mediation analysis showed supervisor as well as peer support to be positively associated with work engagement (B = .34, 95% CI = .21, .47, p< .001; B = .22, 95% CI = .10, .34, p< .001, respectively) (Supplementary file, Table 2, Step 2). Step 3 showed supervisor as well as peer support to be associated with voice behaviors (B = .28, 95% CI = .12, .46, p = .001; B = .126 95% CI = .03, .33, p = .035, respectively) (Supplementary file, Table 2, Step 3). Furthermore, based on step 4, we found supervisor support as well as work engagement to be positively associated with voice behaviors (B = .23, 95% CI = .06, .40, p = .010; B = .30, 95% CI = .14, .45, p< .001, respectively), while peer support and burnout were not associated with voice behaviors (B = .12, 95% CI = −.02, .28, p = .126; B = .17, 95% CI = −.05, .40, p= .129, respectively) (Supplementary file, Table 2, Step 4). Lastly, step 5 of the mediation analysis, i.e. the bootstrap analyses, showed no indirect association in the case of burnout: burnout did not mediate the associations of supervisor and peer support with voice behaviors (B = −.05, 95% CI = −.12, .02; B = −.02, 95% CI = −.05, .01, respectively). On the other hand, the bootstrap analysis showed an indirect association in the case of work engagement: work engagement mediated the associations of supervisor and peer support with voice behaviors (B = .10, 95% CI = .04, .18; B = .06, 95% CI = .02, .13, respectively).
Figure 2. Results of the mediation analysis including the independent variables (supervisor and peer support), the mediators (burnout and work engagement) and the dependent variable (voice behaviors). *p< .05, **p< .01, ***p< .001. The path coefficients in parentheses represent the total effects (Step 3). Coefficients of the control variables years of experience, type of contract and work location were omitted for figure clarity.
Discussion
Main findings
In this observational study among junior doctors in the Netherlands, we found supervisor and peer support to be associated with less burnout and more work engagement. While burnout was not associated with junior doctors’ voice behaviors, more work-engaged junior doctors reported demonstrating more voice behaviors. Specifically, work engagement mediated the association of supervisor and peer support with voice behaviors. On the other hand, the association between supervisor or peer support and voice behaviors was not mediated by burnout.
Explanation of findings
To the best of our knowledge, this was the first study to show that work engagement mediates the associations of supervisor as well as peer support with voice behaviors of junior doctors. This indicates that voice behaviors are more likely demonstrated by work-engaged junior doctors who perceive sufficient supervisor and peer support in their learning environment. As junior doctors are learners and patient care providers at the same time, in an early career stage, supervisor and peer support fosters the feeling of being accepted and valued, thereby promoting their work engagement. In turn, work-engaged junior doctors are dedicated to performing the best they can and go the extra mile for quality improvement, as demonstrated by their report of more voice behaviors. While this finding is in line with the theoretical and empirical underpinnings of the Job Demands and Resources (JD-R) model (i.e. that work engagement mediates associations of support with work behaviors), this study is the first to show this mediating role of work engagement in the context of junior doctors’ voice behaviors (Bakker Citation2011).
While a previous study did not find this mediating role of work engagement (Voogt et al. Citation2019), this study focused on medical trainees, while the current study included junior doctors who were not yet enrolled in postgraduate medical training. These junior doctors provide – under supervision of medical specialists – substantial parts of frontline care while also extending their medical skills in preparation for medical specialty training. This group of junior doctors is commonly in an early career stage while they have a relatively short time (for example because of clinical rotations or short-term contracts) to contribute to quality improvement at the department. In this context, especially work-engaged junior doctors may be dedicated to making the most of their time and learning process at the department by contributing to quality improvement. Indeed, related research – in non-medical settings – found work engagement to be positively associated with voice behaviors (Abdullah et al. Citation2021; Kao et al. Citation2021).
We found voice behaviors to be facilitated by supervisor and peer support, possibly, as both establish junior doctors’ trust that one’s suggestions for change will be appreciated – thereby fostering them to engage in voice behaviors. While both supervisor and peer support were perceived as beneficial for voice behaviors, the junior doctors participating in this study reported that they received less supervisor than peer support (see Results). The receipt of insufficient supervisor support may undermine not only junior doctors’ perceived safety to express their voice but also their ability to deliver optimal patient care (van der Leeuw et al. Citation2012). Good supervision may, however, not always be feasible in the face of time pressures in daily practice, and junior doctors may feel reluctant to seek it due to the fear of decreased credibility (Jansen et al. Citation2021). This fear can be reduced by supervisors’ sharing of their expectations about when and how junior doctors should ask for supervision or offer suggestions for quality improvement. This articulation of expectations would demonstrate supervisors’ openness to junior doctors’ voice behaviors, which has been shown to motivate professionals to speak up (Lebel and Processes Citation2016); whether this is the case for junior doctors has not yet been studied. Furthermore, speaking up could be promoted by team communication training, including improvement of speaking up culture in teams (Jones et al. 2021).
We also found that junior doctors perceive supervisor and peer support to positively contribute to their work-related well-being, as they report being less burned out and more work-engaged. Indeed, preventing burnout and promoting work engagement can be facilitated by supervisors who coach junior doctors and adjust work to their competence levels (van Vendeloo et al. Citation2018; Lases et al. Citation2019). Furthermore, peers’ sharing about stressful experiences (e.g. the emotional demands of patient care delivery) can prevent burnout and improve solidarity through learning from each other’s struggles and successes in maintaining well-being in a stressful practice environment (Abrams Citation2017).
Strengths and limitations
This study was, to the best of our knowledge, the first to investigate how both burnout and work engagement mediated the associations of supervisor as well as peer support with voice behaviors of junior doctors. It used validated instruments and the sample of junior doctors – not yet enrolled in specialty training – was rather unique, as previous research on voice behaviors mostly focused on medical trainees. Yet, junior doctors are an important group to study since they – as frontline care providers – can observe opportunities for quality improvement in daily practice while their junior position in the medical hierarchy may require deliberate support to decrease barriers in demonstrating voice behaviors.
The participating junior doctors self-reported their perceptions of support, work engagement, burnout and voice behaviors, and we cannot exclude the possibility of social desirability bias. However, junior doctors were explicitly informed about the anonymous character of the survey, which was distributed via a generic web link – data could thus not be linked to individual respondents. As respondents were recruited through convenience sampling, we could not calculate the response rate. Thus, we cannot exclude the possibility of self-selection bias, which would mean that scale scores may have been higher or lower in the entire population than in our study sample. Nonetheless, the scale scores were not the focus of the current study, but rather the direction and strength of the associations between the study concepts (based on scale scores). Indeed, the directions and strength of the observed associations among the study concepts were in line with related findings from studies conducted in diverse settings (Teoh et al. Citation2019; Voogt et al. Citation2019).
Furthermore, the cross-sectional design of this study precluded the assessment of causal associations. Longitudinal associations among job resources (including support), burnout, work engagement, and work behaviors have been identified (Lesener et al. Citation2019; Rahmadani et al. Citation2020); but longitudinal associations with voice behaviors in particular have not yet been clarified. Furthermore, additional research is needed to determine the degree to which current findings are generalizable to other healthcare systems; nonetheless our results align with previous findings of related research in diverse healthcare systems (Keyko et al. Citation2016; Teoh et al. Citation2019).
Implications for practice and research
The findings of this study suggest that supervisor and peer support for junior doctors should be proactively promoted. Peer support programs with trained peer coaching of junior doctors, for example, could encourage a culture in which mutual respect, trust, and teamwork are valued and promoted (Shapiro and Galowitz 2016). In addition, regular peer meetings could be held to provide opportunities for junior doctors to empathize with their peers’ experiences in the context of personal and professional development (Abrams Citation2017). Peer support has increasingly been incorporated into well-being programs for junior doctors, and has been shown to reduce their stress levels (Hategan and Riddell Citation2020). Additional research will serve to determine whether peer support programs also help to promote junior doctors’ work engagement.
Given the time pressures experienced in daily practice, the creation of protected time for supervision would facilitate supervisors’ provision of sufficient support to junior doctors. Furthermore, supervisors could proactively teach quality improvement to stimulate junior doctors’ voice in quality improvement, for example by discussing domains of healthcare quality, teaching process mapping, demonstrating root cause analysis or presenting plan-do-study-act cycles (Narayanan et al. Citation2018). Supervisors’ support of junior doctors’ voice behaviors could also be addressed in faculty development programs focusing on how supervisors could cultivate role modeling techniques to stimulate voice behaviors (Passi et al. Citation2013; Sirianni et al. Citation2020). Additionally, supervisors could actively involve junior doctors in quality improvement trajectories, regularly inquiring about their ideas regarding necessary improvements in daily medical practice. Such involvement would enable open dialog about barriers to and opportunities for quality improvement, which should be part of daily practice to foster junior doctors’ perceived safety to engage in voice behaviors. Ultimately, voice behaviors of junior doctors would contribute to their active involvement in quality improvement, which would align with standards of accreditation frameworks worldwide (e.g. the Accreditation Council for Graduate Medical Education) to promote residents’ serving as learners and mentors in delivering high-quality care (Fishbain et al. Citation2019). Further research is needed to clarify how junior doctors’ voice behaviors result in specific improvements of patient care quality.
Conclusions
In this study, junior doctors who received more supervisor and peer support reported less burnout. Burnout was however not associated with junior doctors’ voice behaviors, while junior doctors reported more voice behaviors when being work-engaged professionals who perceive their supervisors and peers to be supportive. Therefore, sustained efforts to cultivate supervisor and peer support are in place, to not only facilitate junior doctors’ work engagement but also their roles as active agents who voice suggestions for health care quality improvement.
Supplemental Material
Download MS Word (33.6 KB)Acknowledgements
The authors wish to thank all junior doctors that participated in the study as well as the Young Doctor for their collaboration in this study. Furthermore, the authors are thankful for Sardes who provided an online platform for the study questionnaire.
Disclosure statement
The authors report there are no conflict of interest.
The web-based platform for the survey was provided by Sardes with financial support of the organization All is health. These organizations had no role in design of the study, analyses of the data and interpretation of the findings.
Additional information
Funding
Notes on contributors
Renée A. Scheepers
Renée Scheepers, PhD, is an Assistant Professor at the department of Socio-Medical Sciences, Erasmus School of Health Policy and Management, Erasmus University of Rotterdam, The Netherlands.
Aline J. Boxem
Aline Boxem, MD, is a PhD Candidate at the department of Pediatrics and the Generation R Study Group (Na-29), Erasmus Medical Center, University Medical Center, Rotterdam, the Netherlands.
Meike M. J. Blezer
Meike Blezer, MD, is a resident at the department of General Practice, Intellectual Disability Medicine of the Erasmus Medical Center, Rotterdam, the Netherlands.
References
- Abdullah H, Ismail I, Alnoor A, Yaqoub E. 2021. Effect of perceived support on employee’s voice behaviour through the work engagement: a moderator role of locus of control. IJPMB. 11(1):60–79. doi: 10.1504/IJPMB.2021.112253.
- Abrams MP. 2017. Improving resident well-being and burnout: the role of peer support. J Grad Med Educ. 9(2):264–264. doi: 10.4300/JGME-D-16-00805.1.
- Bakker AB. 2011. An evidence-based model of work engagement. Curr Dir Psychol Sci. 20(4):265–269. doi: 10.1177/0963721411414534.
- Bakker AB. 2014. The Job Demands–Resources Questionnaire. Rotterdam: Erasmus University.
- Bakker AB, Demerouti E. 2007. The job demands-resources model: state of the art. J Manag Psychol. 22(3):309–328. doi: 10.1108/02683940710733115.
- Chen YC, Issenberg SB, Issenberg Z, Chen H-W, Kang Y-N, Wu J-C. 2022. Factors associated with medical students speaking-up about medical errors: a cross-sectional study. Med Teach. 44(1):38–44. doi: 10.1080/0142159X.2021.1959904.
- Dyrbye LN, Varkey P, Boone SL, Satele DV, Sloan JA, Shanafelt TD. 2013. Physician satisfaction and burnout at different career stages. Mayo Clin Proc. 88(12):1358–1367. doi: 10.1016/j.mayocp.2013.07.016.
- Fishbain D, Danon YL, Nissanholz-Gannot R. 2019. Accreditation systems for postgraduate medical education: a comparison of five countries. Adv Health Sci Educ Theory Pract. 24(3):503–524. doi: 10.1007/s10459-019-09880-x.
- Gin BC, Tsoi S, Sheu L, Hauer KE. 2021. How supervisor trust affects early residents’ learning and patient care: a qualitative study. Perspect Med Educ. 10(6):327–333. doi: 10.1007/s40037-021-00674-9.
- Hariharan TS, Griffin B. 2019. A review of the factors related to burnout at the early-career stage of medicine. Med Teach. 41(12):1380–1391. doi: 10.1080/0142159X.2019.1641189.
- Hategan A, Riddell TJ. 2020. Bridging the gap: responding to resident burnout and restoring well-being. Perspect Med Educ. 9(2):117–122. doi: 10.1007/s40037-020-00567-3.
- Hayes AF. 2017. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New York: Guilford Press.
- Jansen I, Stalmeijer RE, Silkens ME, Lombarts KM. 2021. An act of performance: exploring residents’ decision‐making processes to seek help. Med Educ. 55(6):758–767. doi: 10.1111/medu.14465.
- Kao K-Y, Hsu H-H, Thomas CL, Cheng Y-C, Lin M-T, Li H-F. 2021. Motivating employees to speak up: linking job autonomy, PO fit, and employee voice behaviors through work engagement. Curr Psychol. 41(11):7762–7776. doi: 10.1007/s12144-020-01222-0.
- Keyko K, Cummings GG, Yonge O, Wong CA. 2016. Work engagement in professional nursing practice: a systematic review. Int J Nurs Stud. 61:142–164. doi: 10.1016/j.ijnurstu.2016.06.003.
- Khan A, Teoh KR, Islam S, Hassard J. 2018. Psychosocial work characteristics, burnout, psychological morbidity symptoms and early retirement intentions: a cross-sectional study of NHS consultants in the UK. BMJ Open. 8(7):e018720. doi: 10.1136/bmjopen-2017-018720.
- Kristensen TS, Borritz M, Villadsen E, Christensen KBJW. 2005. The Copenhagen Burnout Inventory: a new tool for the assessment of burnout. Work & Stress. 19(3):192–207. doi: 10.1080/02678370500297720.
- Kuhn CM, Newton RC, Damewood MD, Zaidan JR, Wagner R, Koh NJ, Weiss KB. 2021. New CLER Insights Into the Operative and Procedural Areas of Clinical Learning Environments. J Grad Med Educ. 13(2):301–302. doi: 10.4300/JGME-D-21-00210.1.
- Lases LS, Arah OA, Busch OR, Heineman MJ, Lombarts KM. 2019. Learning climate positively influences residents’ work-related well-being. Adv Health Sci Educ Theory Pract. 24(2):317–330. doi: 10.1007/s10459-018-9868-4.
- Lebel RD, Processes HD. 2016. Overcoming the fear factor: how perceptions of supervisor openness lead employees to speak up when fearing external threat. Organizational Behavior and Human Decision Processes. 135:10–21. doi: 10.1016/j.obhdp.2016.05.001.
- Lemer C, Moss F. 2013. Patient safety and junior doctors: are we missing the obvious? BMJ Qual Saf. 22(1):8–10. doi: 10.1136/bmjqs-2012-001705.
- Lesener T, Gusy B, Wolter C. 2019. The job demands-resources model: a meta-analytic review of longitudinal studies. Work & Stress. 33(1):76–103. doi: 10.1080/02678373.2018.1529065.
- Martinez W, Etchegaray JM, Thomas EJ, Hickson GB, Lehmann LS, Schleyer AM, Best JA, Shelburne JT, May NB, Bell SK. 2015. ‘Speaking up’about patient safety concerns and unprofessional behaviour among residents: validation of two scales. BMJ Qual Saf. 24(11):671–680. doi: 10.1136/bmjqs-2015-004253.
- Maslach C, Schaufeli WB, Leiter MP. 2001. Job burnout. Annu Rev Psychol. 52(1):397–422. doi: 10.1146/annurev.psych.52.1.397.
- Narayanan M, White AA, Gallagher TH, Mookherjee S. 2018. Twelve tips for teaching quality improvement in the clinical environment. Med Teach. 40(10):1060–1066. doi: 10.1080/0142159X.2017.1388501.
- Parker SK, Williams HM, Turner N. 2006. Modeling the antecedents of proactive behavior at work. J Appl Psychol. 91(3):636–652. doi: 10.1037/0021-9010.91.3.636.
- Passi V, Johnson S, Peile E, Wright S, Hafferty F, Johnson N. 2013. Doctor role modelling in medical education: BEME Guide No. 27. Med Teach. 35(9):e1422–e1436. doi: 10.3109/0142159X.2013.806982.
- Prins JT, Hoekstra-Weebers JEHM, Gazendam-Donofrio SM, Van De Wiel HBM, Sprangers F, Jaspers FCA, van der Heijden FMMA. 2007. The role of social support in burnout among Dutch medical residents. Psychol Health Med. 12(1):1–6. doi: 10.1080/13548500600782214.
- Rahmadani VG, Schaufeli WB, Stouten J, Zhang Z, Zulkarnain Z. 2020. Engaging leadership and its implication for work engagement and job outcomes at the individual and team level: a multi-level longitudinal study. Int J Environ Res Public Health. 17(3):776. doi: 10.3390/ijerph17030776.
- Rethans JJ, Norcini J, Baron‐Maldonado M, Blackmore D, Jolly B, LaDuca T, Lew S, Page G, Southgate L. 2002. The relationship between competence and performance: implications for assessing practice performance. Med Educ. 36(10):901–909. doi: 10.1046/j.1365-2923.2002.01316.x.
- Roueche A, Hewitt J. 2012. ‘Wading through treacle’: quality improvement lessons from the frontline. BMJ Qual Saf. 21(3):179–183. doi: 10.1136/bmjqs-2011-000545.
- Seppälä P, Mauno S, Feldt T, Hakanen J, Kinnunen U, Tolvanen A, Schaufeli W. 2009. The Construct Validity of the Utrecht Work Engagement Scale: multisample and Longitudinal Evidence. J Happiness Stud. 10(4):459–481. doi: 10.1007/s10902-008-9100-y.
- Shanafelt TD, Sloan JA, Habermann TM. 2003. The well-being of physicians. Am J Med. 114(6):513–519. doi: 10.1016/s0002-9343(03)00117-7.
- Sirianni G, Glover Takahashi S, Myers J. 2020. Taking stock of what is known about faculty development in competency-based medical education: a scoping review paper. Med Teach. 42(8):909–915. doi: 10.1080/0142159X.2020.1763285.
- Talash K, Corfield L, Latcham N, Lavelle C, Williams R, Machin LL. 2022. Exploring UK foundation doctors’ perceptions surrounding raising concerns in the workplace. J Vocat Educ Train. 74(3):513–527. doi: 10.1080/13636820.2020.1792535.
- Teoh K, Hassard J, Cox T. 2019. Doctors’ perceived working conditions and the quality of patient care: a systematic review. Work Stress. 33(4):385–413. doi: 10.1080/02678373.2019.1598514.
- van den Berg JW, Mastenbroek NJJM, Scheepers RA, Jaarsma ADC. 2017. Work engagement in health professions education. Med Teach. 39(11):1110–1118. doi: 10.1080/0142159X.2017.1359522.
- van der Leeuw RM, Lombarts KM, Arah OA, Heineman MJ. 2012. A systematic review of the effects of residency training on patient outcomes. BMC Med. 10(1):65. doi: 10.1186/1741-7015-10-65.
- Van Dyne L, LePine JA. 1998. Helping and voice extra-role behaviors: evidence of construct and predictive validity. Acad Manag J. 41(1):108–119. doi: 10.2307/256902.
- van Vendeloo SN, Godderis L, Brand PL, Verheyen KC, Rowell SA, Hoekstra H. 2018. Resident burnout: evaluating the role of the learning environment. BMC Med Educ. 18(1):54. doi: 10.1186/s12909-018-1166-6.
- Voogt JJ, Taris TW, van Rensen EL, Schneider MM, Noordegraaf M, van der Schaaf MF. 2019. Speaking up, support, control and work engagement of medical residents. A structural equation modelling analysis. Med Educ. 53(11):1111–1120. doi: 10.1111/medu.13951.
- Voogt JJ, Kars MC, van Rensen EL, Schneider MM, Noordegraaf M, van der Schaaf MF. 2020. Why medical residents do (and don’t) speak up about organizational barriers and opportunities to improve the quality of care. Acad Med. 95(4):574–581. doi: 10.1097/ACM.0000000000003014.