ABSTRACT
In 2016, in Switzerland, we implemented transitional interprofessional and interinstitutional shared decision-making processes (IIPs) between a short-stay inpatient care unit (SSU) and primary care professionals. Between 2018 and 2019, we evaluated this intervention using a realist design to answer the following questions: for whom, with whom, in which context and how have IIPs been implemented? Our initial theory was tested via interviews with patients, primary care professionals and staff from the SSU. Results showed that a patient’s stay at the SSU, with actors committed to facilitating IIPs, reinforced the perceived appropriateness and implementation of those IIPs. However, this appropriateness varied according to different contextual elements, such as the complexity of needs, preexisting collaborative practices and the purpose of the inpatient stay. Since IIPs occurred in a context of fragmented practices, proactive and sustained efforts are required of the actors implementing them and the organizations supporting them.
Introduction
Patients may have high expectations for their healthcare services: “I can plan my care with people who work together to understand me and my carer(s), (…) and bring together services to achieve the outcomes important to me (National Voices, Citation2014).” Patients “living with complexity (Coventry, Small, Panagioti, Adeyemi, & Bee, Citation2015)” face the challenges of fulfilling these expectations.
Complexity, complex needs or complex patients have various definitions (Bunn et al., Citation2018; Coventry et al., Citation2015; Poitras et al., Citation2019; van Reedt Dortland et al., Citation2017). The present study considered patients with complex needs (CNs) – the emergent property resulting from interacting bio-psycho-social and environmental elements, including patients’ individual characteristics (e.g. chronic disease(s), socio-economic difficulties) and the characteristics of the healthcare system (e.g. (multiple) uncoordinated actors). Interprofessional and interinstitutional shared decision-making processes (IIPs), together with adequate coordination between the actors along patients’ care paths, are recommended means of dealing with CNs (Amelung et al., Citation2021; Bunn et al., Citation2018; Coleman & Berenson, Citation2004; Poitras et al., Citation2019).
Patients with CNs face specific issues when transferring between care settings. Indeed, inadequate transitions tend to jeopardize patient safety and autonomy, which can lead to adverse events and rehospitalisation (Amelung et al., Citation2021; Coleman & Berenson, Citation2004). On the contrary, better transitions can improve some of these issues through: i) holistic assessments of patients’ preferences and needs; ii) interprofessional and interinstitutional shared decision-making processes (IIPs) between inpatient and outpatient healthcare providers; and iii) engaging patients and caregivers in shared decision-making processes (Bunn et al., Citation2018; Coleman, Roman, Hall, & Min, Citation2015; Dyrstad, Testad, Aase, & Storm, Citation2015; Graffigna & Barello, Citation2018; Karam, Brault, Van Durme, & Macq, Citation2018; Merten, Van Galen, & Wagner, Citation2017; Philibert & Barach, Citation2012; Poitras et al., Citation2019). Interventions targeting such improvements, that re complex by nature, must manage the healthcare system’s numerous interacting elements (Auschra, Citation2018; Amelung et al., Citation2021; May, Johnson, & Finch, Citation2016). Research on the evaluation of such types of interventions support the assessment not only of processes and outcomes, but also the investigation of contextual elements and mechanisms of change (Amelung et al., Citation2021; May et al., Citation2016). For this purpose, qualitative and mixed methods – including realist evaluation (Emmel, Greenhalgh, Manzano, Monaghan, & Dalkin, Citation2018) – are useful. Such methods have been used to study various aspects of transitions, such as obstacles and facilitators to transitions (Philibert & Barach, Citation2012), effective communication processes (Kripalani et al., Citation2007), and outcomes of transitional processes (Coleman et al., Citation2015). However, to our knowledge, evaluations of interventions targeting the implementation of transitional processes remain scarce.
Background
Several characteristics of Switzerland’s healthcare system make transitions between inpatient and outpatient settings challenging: complicated cost reimbursement schemes hindering simultaneous interventions by inpatient and outpatient professionals; multiple healthcare organizations with their own governance; and hyper-specialized healthcare professionals with traditional (mono)professional roles (De Pietro et al., Citation2015; Kaiser et al., Citation2019; Schmitz, Atzeni, & Berchtold, Citation2020).
In this context, Cité Générations (Eggli, Schaller, & Baudoin, Citation2015), a private medical home in the canton of Geneva, offers outpatient services provided by a variety of healthcare professionals, such as primary care physicians (PCPs), allied health therapists, and two teams from the Geneva Public Institution for Homecare and Assistance (imad throughout the text, for “Institution genevoise de maintien à domicile” (imad, Citation2020), in French). Cité Générations also has a short-stay inpatient care unit (SSU) for patients needing short stays (≤10 days) for medical care and/or geriatric assessment (Eggli et al., Citation2015), and it employs nurses, geriatricians and allied health professionals.
In 2016, Cité Générations began an innovative pilot intervention in its SSU, aiming to improve care transitions for patients with CNs by implementing interprofessional and interinstitutional shared decision-making processes (IIPs). Designed with multi-organizational governance, the intervention adopted a change management approach (Collerette, Schneider, & Lauzier, Citation2013) to diffusing innovation in healthcare services (Greenhalgh, Kyriakidou, & Peacock, Citation2004), and it targeted various components of the healthcare system: i) human resources (introduction of the new position of SSU care coordinator (Nutt & Hungerford, Citation2010)); ii) financing (funding for the care coordinator’s salary); and iii) clinical services delivery (holistic needs assessment and the facilitation of IIPs by the care coordinator). Two types of IIPs were identified: i) iterative IIPs, and ii) meeting IIPs. These differed in terms of the timing of shared decision-making processes: whereas iterative IIPs were multilateral, meeting IIPs were simultaneous (either at the SSU or after the SSU stay). However, the two processes had similar outcomes, and participants had similar characteristics ().
Table 1. Description of interprofessional and interinstitutional shared decision-making processes (IIPs)
This intervention was evaluated in two phases. Between 2017 and 2019, we assessed the intervention’s feasibility, using fidelity and coverage indicators (Schusselé Filliettaz, Moiroux, Marchand, Gilles, & Peytremann-Bridevaux, Citation2021). Then, between 2018 and 2019, we conducted a realist evaluation to better understand for whom, with whom, in which context and how meeting IIPs had been implemented. This manuscript presents the realist evaluation’s results for the issues it is expected to help: i) adjusting the implementation of meeting IIPs for SSU patients with CNs, and ii) implementing meeting IIPs in other similar contexts.
Methods
Realist evaluation
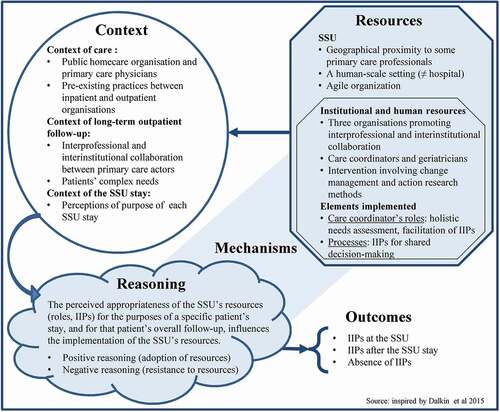
Realist evaluation (RE) is a theory-driven approach considered suitable for evaluating interventions with numerous interacting elements. RE seeks to explain how an intervention worked within a specific context and which mechanisms triggered the expected outcomes in that context (Dalkin, Greenhalgh, Jones, Cunningham, & Lhussier, Citation2015; Emmel et al., Citation2018; Pawson & Tilley, Citation1997) (definitions in ). RE uses an iterative approach: i) an initial intervention theory, based on middle-range theories, describes the key contextual elements and resources used, and outlines the initial mechanisms linking context and outcomes; ii) various Context–Mechanism–Outcome (CMO) configurations are designed and tested using a variety of methods; iii) data analysis produces demi-regularities, which support recommendations resulting from the evaluation. Because RE is challenging, RAMESE’s quality standards were used to support it (Wong et al., Citation2017). Using RE methodology, we planned the steps summarized in and detailed in the following sections.
Table 2. Definitions of intervention, context, mechanisms, outcomes and demi-regularities
Middle-range theories, initial intervention theory and CMO configurations
After a literature review, discussions between the project leaders and preliminary interviews with primary care actors, we selected three middle-range theories:
Dissemination of health innovation. Based on an overall framework (Greenhalgh et al., Citation2004), we focussed on the elements of the assessment of the innovation’s implications for the actors involved, change agents’ characteristics and the specific context of the SSU within the context of care in Switzerland.
Interprofessional and interinstitutional collaboration. Based on an existing overall conceptual framework (D’Amour, Ferrada-Videla, San Martin, & Beaulieu, Citation2005), we focussed on two purposes of IIPs (serving patient and professional needs) and three key elements of collaboration (addressing the complexity of needs, integrating each professional’s perspectives and mutual acquaintanceship).
Partnership between patients and professionals. Based on models advocating partnership (Karazivan et al., Citation2015), and patients’ and relatives’ engagement in care (Carman et al., Citation2013), we focused on patients’ and informal caregivers’ expertise about their priorities and needs, and on their roles as partners in care.
We designed the theoretical elements of our intervention based on elements chosen from three middle-range theories. We considered the occurrence of meeting IIPs to be outcomes with potentially negative and positive consequences. Negative consequences included time spent organizing and conducting IIPs, anxiety resulting from calling care into question, unfamiliar interprofessional and interinstitutional practices, and engaging with colleagues and patients in an unfamiliar care setting. Positive consequences included better quality of care, clearer care plans, increased patient and professional satisfaction, and increased recognition of outpatient actors. We postulated that the innovation’s positive consequences would outweigh its negative ones under the conditions provided by our intervention. Those conditions relied on the middle-range theories used to build the initial intervention theory and the CMO configurations ().
Table 3. Wrapping middle-range theories into an initial intervention theory
Data collection
Data were collected between October 2018 and June 2019 during individual, semi-structured audio-recorded interviews with SSU patients, their primary care professionals and SSU staff. Part one of the interview was descriptive and started with the following question: Could you describe how you/she/he happened to stay at the SSU? This open-ended question enabled the interviewees to recall the context of the SSU stay and the IIPs that happened (or not) during and around this stay. IPPs were mapped out collaboratively by the interviewee and the interviewer on a sheet of paper initially containing only a plain arrow representing time. In accordance with realist interviewing (Manzano, Citation2016), part two of the interview allowed interviewees to confirm, deny or adjust up to nine statements. These statements reflected various CMO configurations testing the initial intervention theory (). For example, the following statement was submitted to the homecare nurses of the SSU patients. It addressed the condition (mutual acquaintanceship) under which the innovation (meeting-IIPs) answered professional needs (preparing the patients’ return).
Mutual acquaintanceship between the UATm staff and me boosts my following my patient even when she/he is no longer at home. I can prepare for her/his return home by participating in or setting up a meeting-IIP.
All original French versions of these statements are available online (see Supplementary Material).
Population and recruitment
Interviewees were selected using non-probabilistic sampling (Manzano, Citation2016), depending on whether meeting IIPs (the outcome) had occurred. This information was available in the SSU electronic health records, in the context of the 2017–2019 intervention feasibility evaluation (see Background section). Starting in mid-2018, we sampled three groups of SSU patients with CNs who: i) had had meeting IIPs at the SSU; ii) had had meeting IIPs within 30 days of discharge from the SSU; and iii) had not had meeting IIPs. Patients were recruited using two additional criteria: i) patients and/or relatives should be able to hold a one-hour conversation in French, and ii) patient follow-up has been and will be by a primary care physician practising in the canton of Geneva and a homecare nurse from the imad. We aimed to recruit three patients per group (expected, n = 9), and for each one accepting to be interviewed, we contacted their primary care physician (PCP), homecare nurse (HN) and the HN’s (Deputy) Team Leader (DTL) (expected, n = 27). We also aimed to interview all the care coordinators and geriatricians active at the SSU during the period studied (expected, n = 4). Appendix ii presents the inclusion flow diagram.
Data analysis
The following steps were taken (Gilmore, McAuliffe, Power, & Vallières, Citation2019; Punton, Vogel, & Loyd, Citation2016):
Each transcript was structured into part one, part two and a discussion about each CMO configuration statement.
CMO configurations were adjusted, and new CMO configurations were identified.
Adjusted CMO configurations from each specific patient–PCP–HN–DTL group were analyzed together to provide deeper insight from their specific context.
Iterative adjustments were made to analyzed transcripts.
Final CMO configurations, demi-regularities and an adjusted intervention theory were identified.
These steps were largely carried out by the main author alone, with input from her PhD supervisor, three experts in RE and an expert in qualitative methods.
Results
Interviews
Of the 40 interviewees targeted, 32 agreed to participate, including 8 patients (plus their relatives), 21 primary care professionals (6 PCPs, 8 HNs and 7 DTLs), and 3 SSU professionals (2 care coordinators and 1 geriatrician) (Appendix ii).
Findings
The following sections present refined insights into every aspect of our realist research question. First, we textually describe demi-regularities by detailing CMO configurations, which will include Context (C), Mechanisms consisting of Resource (Res) and Reasoning (Rea) interactions, and Outcomes (O) (). We then illustrate the demi-regularities using quotations from interviewees.
For whom should meeting IIPs be implemented?
Interviewees highlighted various CNs, such as patient’s characteristics or pathologies, the involvement of multiple professionals, the lack of interprofessional communication or the lack of a common goal (C).
There is complexity at the level of clients’ personalities and at the level of their pathologies. (HN)
[When there are] very complex situations, and goals have not been achieved, or when there is a need for a clearer position from the physician, to see […] what the common goal should be. (DTL)
Meeting IIPs were appropriate (Rea) for CNs. However, the characteristics of (in)stability (C) seemed to affect their relevance.
There are some complex situations that are stable and others that are unstable. And this is where meeting IIPs make sense—when there’s instability. (HN)
For whom were meeting IIPs at the SSU implemented?
Some primary care actors acknowledged CNs (C) and wanted to adapt their follow-up (Rea) in consequence. Meeting IIPs at the SSU (O) were therefore planned and implemented to collectively identify new solutions (Rea) to CNs (C), thanks to there being a combination of the right place (Res), the right time (C) and the adequate delivery of clinical services (Res).
The goal [of a stay at the SSU] was to get all the stakeholders around the table with the patient to see what could be done to improve the situation and make it possible for him to remain at home, since that is clearly what he wants. (PCP)
Some meeting IIPs at the SSU (O) were unplanned before the stay occurred, yet these were nevertheless considered appropriate because shared decision-making (Res) helped to choose between various care options or identify the care problems (Rea).
We had difficulties keeping the patient at home. It was obvious to us that he couldn’t return home. So, we had the meeting IIP [at the SSU], which was good. (DTL)
There are several reasons for having meeting IIPs: [… when] there are disagreements regarding the [care] project and what should come next […], when there is a radical redefinition of the level of care, [and] when there are repeated failures, with patients going back and forth, and you don’t understand why. (SSU geriatrician)
Meeting IIPs also took place at the SSU (O) specifically to integrate professionals’ perspectives and improve interprofessional collaboration (Rea) between the primary care actors. They occurred because of the SSU stay (C) and thanks to the care coordinator’s role (Res).
It was complicated. Her husband spoke a lot in her place […]. And I could never get hold of the physician. It was hard to make sense of it all. I talked about it with the care coordinator, and I think he helped since he had the contacts, and he had all those people [on hand] at the same time. After that [meeting IIP], things at home went more smoothly. (HN)
Reconciling the patient’s needs and priorities with ambulatory follow-up (C) can represent a challenge for professionals and a risk to patient safety. Meeting IIPs thus also made sense as moments of catharsis (Rea) when actors could share their difficulties and concerns. Driven by the SSU care coordinator (Res), these meeting IIPs (O) made it possible to overcome the perceived incompatibilities, e.g. between a patient’s wishes and the risks considered by professionals (Rea).
We had to create a specific [care plan] and then stick to it. […] I guess the meeting occurred thanks to [the care coordinator]. […] [The patient’s follow-up] could go badly wrong. But at least we were able to say that this was our concern, and perhaps [the meeting IIPs] helped to give us some peace of mind, too. (PCP)
For whom were home-meeting IIPs implemented after their SSU stay?
For some patients with CNs (C), holding meeting IIPs in their home was considered more appropriate (O) than at the SSU. This occurred when a key actor was unable to attend meeting IIPs at the SSU (Rea), whether for logistical, physical or psychological reasons, and when the existing partnership between the stakeholders was endangered by a decision process made in someone’s absence (C).
We knew that [the situation] was difficult, but the SSU team said, ‘You have to […]’. But first, it’s too complicated. And then we’d make [the spouse] angry. […] The purpose of having the meeting [in their home] was [maintaining] the therapeutic alliance. (PCP)
With whom were IIPs implemented?
Patients trusted that healthcare professionals interacted to discuss care options and make decisions, even in the patients’ absence. Processes such as meeting IIPs gathering all the relevant actors (O) were welcome starting points (Rea), but subsequent processes did not necessarily require the presence of every actor and maybe not even the patient (O).
[The meeting IIP] was especially important to know where I was going. Afterwards, the discussions with each doctor separately were more than enough for me. […]And then, they have their own bilateral discussions. That makes me feel 100% reassured. (Patient)
Homecare professionals had diverging opinions on who should participate in IIPs (O), but this should be understood in light of how the imad is organized. Its various professionals include a reference homecare nurse, numerous attending nurses with irregular shifts and clinical activities, and a DTL who remains in the office, has access to the patient’s record and is easily reachable by telephone during business hours (C).
The DTL [should be in contact with the SSU] because DTLs are much more easily available and have all the information. (DTL)
The [reference] HN tries to maintain regular contact with patients we are responsible for, who are either at the SSU or in the hospital. […] That’s the difference between the [reference] HN in the field—who really knows the situation, the environment, and all the other problems that can revolve around it—and my position [as DTL], only having the elements in the patient’s record and oral feedback. (DTL)
Sometimes, depending on the topics to be addressed in shared decision-making processes, actors accepted not participating in the meeting IIPs (O) as they deemed their expertise to be effectively represented by somebody else (Rea).
A couple of times, I didn’t go to the meeting IIPs. […] I could have been there, but the decisions could still have been made, and the expertise [available at the SSU] meant that I wasn’t needed. (PCP)
Even with specific patients’ characteristics, e.g. those having cognitive impairments (C), meeting IIPs also made sense (O). However, preliminary iterative IIPs seemed to be appropriate (O) for improving the diversity of data used for shared decision-making processes (Rea).
I think [meeting IIPs] are appropriate. It is just that I think there should be preliminary discussions on the side. Because when you talk to my relative, he’s going to say “yes” to almost everything. He has lost his bearings a little bit. So, you’re going to have a lot of things that aren’t right. […] That’s why I think it’s good to do it this way: [first multilateral IIPs, then meeting IIPs]. (Relative)
In which contexts were meeting IIPs implemented?
CNs assessment had been implemented at the SSU to provide new insights into long-term follow-up (C). Depending on how primary care actors reacted (Rea) to such assessment (Res), IIPs did or did not occur (O).
Some primary care actors acknowledged their patient’s CNs and the risk that they might become chronic (C). Additionally, those primary care actors did not feel threatened (Rea) by the SSU carrying out a CNs assessment and suggesting IIPs (Res). In these cases, meeting IIPs took place at the SSU (O).
A stay at the SSU may be a sign […] that some issues need to be examined again. […] The SSU’s professionals also have a fresh take on the situation. […] They gather information from all sides; they re-centralise it a bit. That’s something which I sometimes might not do on my own or which [homecare] might not necessarily initiate. [An SSU stay] might be the time to send out an alert […]: should we have a meeting IIP or not? (PCP)
Meeting IIPs were considered inappropriate (O) in situations where the actors decided not to question decisions about follow-up (Rea). This decision relied on a cost–benefit analysis, weighing the probable reactions of the actors involved, the energy required, and the shared decision-making processes’ potential benefits to the patient’s CNs (Rea).
It’s often the HN who says, ‘[…] it’s not working too badly; it’s holding up as well as can be expected. […]’ Sometimes you feel that it’s not the right moment because they’re here for a rest, not for anything else. And the shared goal is not to stir things up. (SSU care coordinator)
Sometimes, in these types of situations, it’s not easy to reach [any kind of shared decision]. […] There are some situations that I call super-complex: which ever way you turn them […] your solutions won’t float, they just sink. (SSU care coordinator)
Throughout the interviews, it appeared that interprofessional processes already occurred in care settings other than the SSU (C). IIPs including patients and inpatient and outpatient professionals, however, were considered innovative. When one of their patients stayed at the SSU, many primary care professionals drew parallels with practices experienced in other inpatient settings (C), and they expected less communication in general (O). Expecting the usual inpatient model, but experiencing a different one, elicited various reactions from primary care professionals.
Indeed, several HNs interrupted their follow-up during an SSU stay and refrained from proactively asking for news (C). They reduced their involvement during inpatient stays, passively awaiting instructions on the patient’s return home (C).
Once people leave [home], we have other things to think about, unfortunately. I must admit that I don’t necessarily check in. I figure that when they leave [the inpatient setting], I’ll be informed. (HN)
The idea of the SSU actively involving homecare professionals (Res) was thus a welcome innovation (O). Indeed, it acknowledged that HNs were experts in outpatient follow-up. It enabled horizontal, partnership-based communication and shared decision-making that met both patients’ and professionals’ needs (Rea).
The SSU contacted [the reference HN] several times, to discuss setting up a meeting IIP, to check on how they all saw the future. […] [The HN] was pleasantly surprised. […] We don’t necessarily have any direct contact with other [inpatient] structures, with information being asked for or knowing what’s being done. It’s usually more like, ‘The patient was admitted on this date, they’ll come out on that date, and this is what will be asked of you.’ (HN)
When the SSU solicited the active involvement of PCPs, there were different perceptions. On the one hand, some PCPs continued to take care of their patients during their SSU stay (C), and in this context, the SSU’s resources (Res) appeared to be normal (Rea), and IIPs were welcome (O) as part of daily collaborative practice (Rea).
When my patients are at the SSU, I follow them; I see them practically every day. As a result, I interact with one of the two nurses […] who also assesses their needs with regard to a possible return home. […] I can communicate how I would like the processes to go. In general, though, we pretty much share the same vision. It really is a collaboration. (PCP)
On the other hand, some PCPs reduced their involvement during their patient’s SSU stay (C) and considered that the SSU geriatrician (Res) should be in charge. However, PCPs seemed to be ambivalent about the degree to which their involvement should be reduced during the SSU stay: whereas they acknowledged their lack of time and physical distance, PCPs still wanted to be part of decision-making processes (Rea).
As a fairly important link, the PCP has to be there, but not as the instigator of meeting IIPs. I’d say that maybe we should be a little bit more behind the scenes than when the patient is at home. (PCP)
Although the context is fragmented, with heterogeneous practices and expectations (C), these quotations reflected primary care actors’ positive reasoning about the SSU’s resources. However, inducing this positive reasoning required considerable efforts on the part of the SSU (Res), and primary care actors acknowledged this.
Depending on the case, I either go [to the SSU or] leave it up to [the SSU geriatrician]. It’s not highly codified. […] I can get involved in the situation or not, and they’ll adapt. They make it easier for us. (PCP)
The SSU staff showed resilience and agility (Res) in the face of all kinds of reasoning by primary care actors (Rea). When asked about the reasons for this resilience and agility, SSU staff described various elements, including individual characteristics (Res), such as their engagement and determination, and their readiness to adjust the limits of their role.
[We] are rather bold. We have a rather crazy vision of what a nurse’s role should be. I’m not saying that’s a bad thing, but it is rather different when it comes to taking risks and breaking out of that role’s boundaries. (SSU care coordinator)
It requires a lot of adaptability from the SSU staff. […] The SSU geriatrician should not be too touchy. He must not want to take the place of the PCP, but he must nevertheless get quite involved and consult with the PCP. So, it requires discussion and not a little diplomacy. (SSU geriatrician)
Second, organizational elements at the SSU were also highlighted as resources facilitating IIPs, such as managerial vision and the choice of agile staff (Res).
I think that leadership in the choice of staff […] is important. The people working at the SSU are not there by chance. […] I think that a lot depends on [leadership] and on the impetus it gives to human relationships. (SSU geriatrician)
Finally, the geographical proximity of the SSU and the imad’s two homecare offices (Res) had a positive impact on the imad interviewees’ reasoning about the SSU’s resources: it facilitated and strengthened direct interpersonal links, thus increasing interinstitutional collaboration at the operational level, e.g. serving their respective professional needs (Rea), such as proactively providing information.
We make things easier on both sides because we know each other. […] And I think we’re privileged because of our geographical [proximity] to the SSU. (DTL)
Unexpected results
Although interviewees found IIPs appropriate, some raised concerns about how decisions were implemented.
I don’t mind [meeting IIPs]. […] Sometimes, I wish they were more concrete—that things were implemented. In fact, every time [my relative] returns home from somewhere, suggestions are made but never implemented. […] They listen to you, but then afterwards, everybody does their own thing. And that’s what bothers me. (Relative)
Whatever the shortcomings in the implementation of decisions made during meeting IIPs, our findings revealed no negative ripple effects on the implementation of further IIPs.
Discussion
The present realist evaluation aimed to provide a better understanding of for whom, with whom, in which context and how meeting IIPs had been implemented at our participating SSU. Findings showed that the implementation of IIPs made sense, especially for patients with CNs. IIPs seemed especially legitimate and were implemented when actors considered that CNs were undergoing acute changes, such as growing instability in the patient’s health status or major readjustments in healthcare service provision or interprofessional practices. Meeting IIPs were also welcome when actors felt uneasy about chronic CNs, and they were ready to re-discuss care and practices with the SSU’s professionals. On the contrary, meeting IIPs did not seem necessary when the actors felt CNs had stabilized. In general, all actors were considered to have a role in IIPs. However, depending on elements such as the time available and the potential impact of the decisions made, some actors were not included in IIPs, did not attend them or took part in iterative IIPs but not meeting IIPs.
Refined intervention theory
A refined intervention theory was formulated based on these findings ().
A patient’s SSU stay (Res), with actors committed to facilitating IIPs (Res), will reinforce the perceived appropriateness (Rea) and implementation of meeting IIPs (O). Perceptions of this appropriateness will vary according to different contextual elements, such as the complexity of needs (C), pre-existing collaborative practices (C) and the purpose of the SSU stay (C).
Resources (Res)
Initially, three resources for the intervention were identified: i) the interinstitutional nature of the intervention; ii) the change management approach used; and iii) the newly created position of the SSU care coordinator, delivering specific services (i.e. needs assessment and facilitation of IIPs). However, three additional elements, linked to the SSU itself, also emerged in the adjusted CMO configurations. First, the location of the SSU within the Cité Générations medical home, which hosts both inpatient and outpatient care providers, created physical proximity and facilitated contact between professionals. Second, the SSU’s professionals, chosen by their managers for their professional and personal characteristics, were considered especially innovative and flexible in their responses to the variety of CNs. Finally, the SSU’s configuration and small size were considered to favor the formation of interpersonal and interprofessional acquaintanceships. These resources (Res) resonated with important dimensions of interprofessional and interinstitutional collaboration (Axelsson & Bihari Axelsson, Citation2006; D’Amour et al., Citation2005; Mickan & Rodger, Citation2005): mutual acquaintanceship, local leadership, interconnections between individuals and institutions, management support for innovation, and role flexibility.
Context (C)
Our theory’s context was refined into three categories.
The global context of care and its systemic elements, such as fragmented financing, institutions and practices. These elements favor a traditional division of tasks between actors and hinder IIPs (Gurtner & Wettstein, Citation2019; Schmitz et al., Citation2020). This was very much assimilated by primary care professionals and was transposed to the SSU, which they considered as a hospital. As a result, primary care actors tended to reduce their involvement during their patient’s SSU stay, requiring additional efforts from the SSU professionals to reach out to primary care actors and to implement IIPs.
The challenges of primary care follow-up. When facing chronic CNs and their potential burden in terms of duration, workload and possible failures of care (Sav et al., Citation2015; Sinnott, Georgiadis, Park, & Dixon-Woods, Citation2020), primary care actors’ readiness to question care and interprofessional practices was heterogeneous and required adaptability on behalf of the SSU professionals.
The purpose of a specific SSU stay. Within long-term, overall outpatient follow-up, an SSU stay was perceived as either an important step or just a parenthesis disconnected from that overall follow-up. This influenced what primary care actors expected from the SSU stay and made meeting IIPs appropriate or not.
Reasoning (Rea)
Reasoning () was formulated as follows: the perceived appropriateness of SSU resources – for the purposes of both a specific patient’s stay and their overall follow-up – influences the implementation of the SSU’s resources. That is, if the SSU’s resources were perceived as inappropriate, meeting IIPs were not implemented. If the resources were perceived as appropriate, actors adopted IIPs (e.g. meeting IIPs at the SSU) or adjusted them (e.g. meeting IIPs at patients’ homes).
Implications of these findings
Suggestions for the SSU
This realist evaluation, made after a three-year pilot implementation, showed that IIPs could indeed be implemented within specific CMO configurations, including the individual characteristics of the two SSU care coordinators. They showed great motivation and flexibility, which are crucial psychological characteristics for the diffusion of innovation (Greenhalgh et al., Citation2004). However, it is unclear whether such psychological characteristics would be appropriate for the sustainable implementation of IIPs. Additionally, further resources will be essential to financing the care coordinator’s position once the pilot intervention is over. For this specific purpose, bundled (Berchtold, Reich, Schimmann, & Zanoni, Citation2017) SSU payments will be investigated so as to include coordination.
Suggestions for other short-term inpatient care units
If new, similar, short-term stay medical units are to be created, or if other existing units want to improve their IIPs, they should consider the following elements. First, initial projects should be designed with a focus on agility, and professionals should be selected based on their ability to innovate and work with uncertainties (Greenhalgh et al., Citation2004). Second, small units should be considered to ensure that they are at a human-scale, as highlighted by respondents. Third, SSUs should be built close to primary care actors to facilitate mutual acquaintanceship. Finally, community-oriented models (Lalani, Fernandes, Fradgley, Ogunsola, & Marshall, Citation2019; Monsen & De Blok, Citation2013), promoting interprofessional primary-care teamwork and limiting catchment areas, could increase the number of patients taken care of by the same professionals (e.g. PCPs and HNs). This could also increase mutual acquaintanceship between primary care actors (D’Amour et al., Citation2005), reduce the “fragility and volatility” of interprofessional collaboration (Axelsson & Bihari Axelsson, Citation2006) and reinforce the perceived appropriateness of IIPs during inpatient stays.
Suggestions for homecare
Several elements explain homecare professionals’ various opinions about the relevance of IIPs: i) the diverse “task relevance (Greenhalgh et al., Citation2004)” of IIPs for patients with and without CNs; ii) the “feasibility (Greenhalgh et al., Citation2004)” of IIPs, related to the physical distance between many homecare teams’ offices and the SSU; iii) the “differentiation (Axelsson & Bihari Axelsson, Citation2006)” between inpatient and homecare structures; and vi) collaboration with the SSU, heterogeneously assigned to the HN or the DTL. To overcome these challenges, homecare stakeholders should identify relevant approaches like: i) providing proactive and targeted information about the specificities of the SSU’s resources for transitional processes; and ii) clarifying the respective roles and professional needs of HNs and DTLs during an inpatient stay.
Strengths and limitations
This work has two main strengths. First, the sampling of interviewees helped us to gain deeper insight into the research question by targeting groups of primary care actors related to three different outcomes. Second, three of this realist evaluation paper’s authors also led the implementation of IIPs at the SSU. Whereas this might be considered a limitation in summative evaluations, it made sense in our context and helped us gain extra ontological depth.
Nevertheless, the following major limitation must be considered when interpreting our findings. Realist data analysis is a methodological challenge (Malengreaux, Doumont, & Aujoulat, Citation2020), which must often be handled by a group of researchers (Emmel et al., Citation2018). Because this group handling was impossible, the quality of the analysis was improved through iterative procedures. To further refine our CMO configurations and the intervention theory, to adjust the intervention in the field and to adjust the lessons learnt for further contexts, several workshops with different stakeholders in the canton of Geneva will take place in the near future.
Conclusions
The present realist evaluation of the implementation of interprofessional and interinstitutional transitional processes showed their appropriateness for meeting a variety of complex needs, including interprofessional and interinstitutional collaboration. Since IIPs occurred within an overall context of fragmented, heterogeneous practices, those processes required sustained efforts from the actors implementing them and the organizations supporting them.
Ethical approval
This study was approved by the Geneva Cantonal Research Ethics Committee (Req-2018-00801).
Authors’ contributions
SSF designed the study, with input from SM and GM, under the supervision of IPB. SSF performed all the interviews, transcribed the interviews with the help of two assistants and analysed the data. SSF prepared the manuscript with input from IPB, IG, SM & GM. All the authors read and approved the final manuscript.
Supplemental Material
Download JPEG Image (1.5 MB)Supplemental Material
Download JPEG Image (716.6 KB)Acknowledgments
The authors gratefully acknowledge the patients, informal caregivers, SSU staff and primary care professionals who were invaluable actors in our study. Special thanks go to: Dr Philippe Schaller, founder of Cité Générations, who supported this evaluation; Prof. Jean-François Balavoine and Francis Waldvogel of the PRISM Association, which funded the main researcher’s salary and part of the care coordinator’s salary; the Geneva Institution for Homecare and Assistance (imad), which granted us access to homecare data and facilitated change management; and Lucile Battaglia, a nurse at imad, who participated in study implementation and contributed to data collection.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website.
Additional information
Funding
References
- Amelung, V., Stein, V., Suter, E., Goodwin, N., Nolte, E., and Balicer, R. (Eds.). (2021). Handbook integrated care (2nd ed.). Cham, Switzerland: Springer International Publishing. doi:https://doi.org/10.1007/978-3-030-69262-9
- Auschra, C. (2018). Barriers to the integration of care in inter-organisational settings: A literature review. Int J Integr Care, 18(1), 5 doi:https://doi.org/10.5334/ijic.3068.
- Axelsson, R., & Bihari Axelsson, S. (2006). Integration and collaboration in public health—A conceptual framework. Int. J. Health Plan. Manag., 21(1), 75–88. doi:https://doi.org/10.1002/hpm.826
- Berchtold, P., Reich, O., Schimmann, F., & Zanoni, U. (2017). Modèles de rémunération liée à la performance à l’horizon 2025 [Pay-for-performance models towards 2025] Matière à réflexion No 3). Neuaegeri, Switzerland: Forum Managed Care Retrieved 10 06 2017. www.fmc.ch
- Bunn, F., Goodman, C., Russell, B., Wilson, P., Manthorpe, J., Rait, G., & Durand, M.-A. (2018, 18). Supporting shared decision making for older people with multiple health and social care needs: A realist synthesis. BMC Geriatrics, 18(1), 165. doi:https://doi.org/10.1186/s12877-018-0853-9
- Carman, K. L., Dardess, P., Maurer, M., Sofaer, S., Adams, K., Bechtel, C., & Sweeney, J. (2013). Patient and family engagement: A framework for understanding the elements and developing interventions and policies. Health Affairs (Millwood), 32(2), 223–231. doi:https://doi.org/10.1377/hlthaff.2012.1133
- Coleman, E. A., & Berenson, R. A. (2004). Lost in transition: Challenges and opportunities for improving the quality of transitional care. Annals of Internal Medicine, 141(7), 533–536. doi:https://doi.org/10.7326/0003-4819-141-7-200410050-00009
- Coleman, E. A., Roman, S. P., Hall, K. A., & Min, S. (2015). Enhancing the care transitions intervention protocol to better address the needs of family caregivers. J Healthc Qual, 37(1), 2–11. doi:https://doi.org/10.1097/01.JHQ.0000460118.60567.fe
- Collerette, P., Schneider, R., & Lauzier, M. (2013). Le pilotage du changement [Change management] (2nd ed., 293 p. ISBN 978-2-7605-2533-7). Quebec, Canada: University of Quebec Press.
- Coventry, P. A., Small, N., Panagioti, M., Adeyemi, I., & Bee, P. (2015). Living with complexity; marshalling resources: A systematic review and qualitative meta-synthesis of lived experience of mental and physical multimorbidity. BMC Family Practice, 16(171), 12. doi:https://doi.org/10.1186/s12875-015-0345-3
- D’Amour, D., Ferrada-Videla, M., San Martin, R. L., & Beaulieu, M. D. (2005). The conceptual basis for interprofessional collaboration: Core concepts and theoretical frameworks. J Interprof Care, 19(Suppl 1), 116–131 doi:https://doi.org/10.1080/13561820500082529.
- Dalkin, S. M., Greenhalgh, J., Jones, D., Cunningham, B., & Lhussier, M. (2015). What’s in a mechanism? Development of a key concept in realist evaluation. Implement Sci, 10(1), 49. doi:https://doi.org/10.1186/s13012-015-0237-x
- De Pietro, C., Camenzind, P., Sturny, I., Crivelli, L., Edwards-Garavoglia, S., Spranger, A., Wittenbecher, F., and Wilm, Q., 2015). Health system review: Switzerland Health Systems in Transition No 4, Vol. 17). Copenhagen, Denmark: European Observatory on Health Systems and Policies Retrieved 25 02 2017. www.euro.who.int
- Dyrstad, D. N., Testad, I., Aase, K., & Storm, M. (2015). A review of the literature on patient participation in transitions of the elderly. Cognition, Technology & Work, 17(1), 15–34. doi:https://doi.org/10.1007/s10111-014-0300-4
- Eggli, Y., Schaller, P., & Baudoin, F. (2015). Évaluation d’une structure gériatrique entre l’ambulatoire et l’hospitalier [Evaluation of a geriatric structure between outpatient and inpatient settings]. Santé publique, 1(HS), 167–175. doi:https://doi.org/10.3917/spub.150.0167
- Emmel, N., Greenhalgh, J., Manzano, A., Monaghan, M., and Dalkin, S. (Eds.). (2018). Doing realist research (1st ed., 251 p. ISBN 978-1-4739-7789-1). Los Angeles, USA: Sage.
- Gilmore, B., McAuliffe, E., Power, J., & Vallières, F. (2019). Data analysis and synthesis within a realist evaluation: Toward more transparent methodological approaches. Int J Qual Methods, 18, 11. doi:https://doi.org/10.1177/1609406919859754
- Graffigna, G., & Barello, S. (2018). Spotlight on the Patient Health Engagement model (PHE model): A psychosocial theory to understand people’s meaningful engagement in their own health care. Patient Prefer. Adherence, 12, 1261–1271. doi:https://doi.org/10.2147/PPA.S145646
- Greenhalgh, T., Kyriakidou, O., & Peacock, R. (2004). How to spread good ideas : A systematic review of the literature on diffusion, dissemination and sustainability of innovations in health service delivery and organisation). London, UK: National Co-ordinating Centre for NHS Service Delivery and Organisation R&D (NCCSDO) Retrieved 08 06 2018. http://citeseerx.ist.psu.edu
- Gurtner, S., & Wettstein, M. (2019). Interprofessionelle Zusammenarbeit im Gesundheitswesen - Anreize und Hindernisse in der Berufsausübung [Interprofessional collaboration in the health sector: Facilitators and obstacles in professional practices]). Bern, Switzerland: Federal office of public health Retrieved 17 10 2019. www.bag.admin.ch
- imad. (2020). Institution genevoise de maintien à domicile (imad) [Geneva institution for homecare and assistance] [Internet]. Retrieved from www.imad-ge.ch
- Kaiser, N., Amann, F., Meier, N., Inderbitzi, L., Haering, B., Eicher, M., and Stanic, J, 2019). Berufsausübung: Potenziale für Interprofessionalität [Professional practice: Potentials for interprofessionality] (90 p. Retrieved 18 10 2019). Bern, Switzerland: Federal office of public health (FOPH). www.bag.admin.ch
- Karam, M., Brault, I., Van Durme, T., & Macq, J. (2018). Comparing interprofessional and interorganizational collaboration in healthcare: A systematic review of the qualitative research. Int J Nurs Stud, 79, 70–83. doi:https://doi.org/10.1016/j.ijnurstu.2017.11.002
- Karazivan, P., Dumez, V., Flora, L., Pomey, M.-P., Del Grande, C., Ghadiri, D. P., & Lebel, P. (2015). The Patient-as-Partner approach in health care: A conceptual framework for a necessary transition. Academic Medicine, 90(4), 437–441. doi:https://doi.org/10.1097/ACM.0000000000000603
- Kripalani, S., LeFevre, F., Phillips, C. O., Williams, M. V., Basaviah, P., & Baker, D. W. (2007). Deficits in communication and information transfer between hospital-based and primary care physicians: Implications for patient safety and continuity of care. JAMA, 297(8), 831–841. doi:https://doi.org/10.1001/jama.297.8.831
- Lalani, M., Fernandes, J., Fradgley, R., Ogunsola, C., & Marshall, M. (2019). Transforming community nursing services in the UK; lessons from a participatory evaluation of the implementation of a new community nursing model in East London based on the principles of the Dutch Buurtzorg model. BMC Health Services Research, 19(1), 945. doi:https://doi.org/10.1186/s12913-019-4804-8
- Malengreaux, S., Doumont, D., & Aujoulat, I. (2020,). L’approche réaliste pour évaluer les interventions de promotion de la santé: éclairages théoriques [The realistic approach to evaluating health promotion interventions: Theoretical insights]). Louvain-la-Neuve, Belgium: Service universitaire de promotion de la santé de l’Université catholique de Louvain Retrieved 14 06 2020. https://promosante.org
- Manzano, A. (2016). The craft of interviewing in realist evaluation. Evaluation, 22(3), 342–360. doi:https://doi.org/10.1177/1356389016638615
- May, C. R., Johnson, M., & Finch, T. (2016). Implementation, context and complexity. Implementation Science, 11(1), 141. doi:https://doi.org/10.1186/s13012-016-0506-3
- Merten, H., Van Galen, L. S., & Wagner, C. (2017, 9). Safe handover. BMJ, 359, j4328. doi:https://doi.org/10.1136/bmj.j4328
- Mickan, S. M., & Rodger, S. A. (2005). Effective health care teams: A model of six characteristics developed from shared perceptions. J Interprof Care, 19(4), 358–370. doi:https://doi.org/10.1080/13561820500165142
- Monsen, K. A., & De Blok, J. (2013). Buurtzorg Nederland: A nurse-led model of care has revolutionized home care in the Netherlands. AJN, 113(8), 55–59. doi:https://doi.org/10.1097/01.NAJ.0000432966.26257.97
- Nutt, M., & Hungerford, C. (2010, August). Nurse care coordinators: Definitions and scope of practice. Contemporary Nurse, 36(1–2), 71–81. doi:https://doi.org/10.5172/conu.2010.36.1-2.071
- Pawson, R., & Tilley, N. (1997). Realistic evaluation 235 p. ISBN 9780761950080). London, UK: SAGE Publications Ltd.
- Philibert, I., & Barach, P. (2012). The European HANDOVER Project: A multi-nation program to improve transitions at the primary care—inpatient interface. BMJ Quality & Safety, 21(Suppl 1), i1–6. doi:https://doi.org/10.1136/bmjqs-2012-001598
- Poitras, M.-E., Hudon, C., Godbout, I., Bujold, M., Pluye, P., Vaillancourt, V. T., Debarges, B., Poirier, A., Prevost, K., Spence, C., and Legare, F., 2019). Decisional needs assessment of patients with complex care needs in primary care. J Eval Clin Pract. doi:https://doi.org/10.1111/jep.13325.
- Punton, M., Vogel, I., & Loyd, R. (2016). Reflections from a realist evaluation in progress: Scaling ladders and stitching theory (Centre for Development Impact Practice Paper Nr 18). UK: UK Department for International Development Retrieved 03 03 2020. www.ids.ac.uk/cdi
- Redding, D., Gentry, T., Shand, J., and Stuart, L. (2014). I’m still me: A narrative for coordinated support for older people). UK: National Voices, Age UK & UCL Partners Retrieved 16 01 2017. www.nationalvoices.org.uk
- Sav, A., King, M. A., Whitty, J. A., Kendall, E., McMillan, S. S., Kelly, F., & Wheeler, A. J. (2015, June). Burden of treatment for chronic illness: A concept analysis and review of the literature. Health Expectations, 18(3), 312–324. https://doi.org/10.1111/hex.12046
- Schmitz, C., Atzeni, G., & Berchtold, P. (2020). Interprofessionelle Zusammenarbeit in der Gesundheitsversorgung: Erfolgskritische Dimensionen und Fördermassnahmen [Interprofessional cooperation in health care: Critical dimensions and support measures]. Swiss Academies Communications, 15(2), 136 Retrieved 18 02 2020 www.samw.ch.
- Schusselé Filliettaz, S., Moiroux, S., Marchand, G., Gilles, I., & Peytremann-Bridevaux, I. (2021, March). Transitional shared decision-making processes for patients with complex needs: A feasibility study. J Eval Clin Pract., 1–9 org/10.1111/jep.13561.
- Sinnott, C., Georgiadis, A., Park, J., & Dixon-Woods, M. (2020). Impacts of operational failures on primary care physicians’ work: A critical interpretive synthesis of the literature. Ann Fam Med, 18(2), 159–168. https://doi.org/10.1370/afm.2485
- van Reedt Dortland, A. K. B., Peters, L. L., Boenink, A. D., Smit, J. H., Slaets, J. P. J., Hoogendoorn, A. W., … Ferrari, S. (2017). Assessment of biopsychosocial complexity and health care needs: Measurement properties of the INTERMED self-assessment version. Psychosomatic Medicine, 79(4), 485–492. doi:https://doi.org/10.1097/PSY.0000000000000446
- Wong, G., Westhorp, G., Greenhalgh, J., Manzano, A., Jagosh, J., & Greenhalgh, T. (2017). Quality and reporting standards, resources, training materials and information for realist evaluation: The RAMESES II project. Health Serv Res, 5(28), 1–108. doi:https://doi.org/10.3310/hsdr05280