Abstract
The objective of this review was to collect information on available additive manufacturing technologies used for the fabrication of either single crowns or fixed-dental prosthesis (FDP) with a focus on the chemistry, surface characteristics and interaction between frameworks and veneering ceramics. Original scientific papers in MEDLINE (PubMed), Embase, Scopus databases, published between 01 January 1996 and 30 June 2020 were included in this review. The following MeSH terms, search terms and their combinations were used: ‘in vitro’, ‘crowns’, ‘denture, partial, fixed’, ‘dentistry’, ‘fixed dental prosthesis’, ‘FDP’, ‘bridges’, ‘additive manufacturing’, ‘alloys’, ‘surface roughness’, ‘adhesion’. Two reviewers performed screening and analysed the data. Only the studies that reported on chemistry, surface characteristics and ceramic adhesion for FDPs were included. The selection process resulted in the final sample of 91 journal articles. In total, 16 articles were identified related to chemistry of alloys used in additive manufacturing: 1 on surface characteristics, and 9 on adhesion of veneering ceramics to alloys. In addition, review articles, books, patents and manufacturers` information were retrieved. Accordingly, it was noted that current additive technologies use mainly Co-Cr or titanium alloys but the production of the starting material presently lacks sufficient standardization and regulations. For these alloys, rougher surface microstructure (3.2 ± 0.4 µm) than for cast alloys (2.3 ± 0.6 µm) was reported which may have clinical implications in implant dentistry. There is some evidence that surface roughness contributes to increased bond strength of veneering ceramic to metal frameworks ranging between 24 ± 10 and 54 ± 14 MPa but the detailed underlying metal-ceramic adhesion mechanism remains to be elucidated.
Introduction
Metal-ceramic reconstructions have been considered as the gold standard for dental restorations for several decades [Citation1,Citation2]. Yet, a major problem in reconstructive dentistry remains chipping of the veneering ceramic from metal frameworks [Citation3]. Even though considerable efforts have been undertaken in order to improve the bond strength between the ceramic and the metal substrate, fractures of ceramic veneers still occur occasionally under clinical conditions. Clinical studies showed that the prevalence of ceramic fractures ranges between 5% and 10% over 10 years of function [Citation4,Citation5]. Although fractures do not necessarily mean the failure of the restoration, the renewal process is both costly and time consuming, and therefore remains a clinical problem. Published literature reveals that the reasons for failures cover a wide spectrum from iatrogenic causes to laboratory errors during processing metals or layering ceramics [Citation3]. The laboratory process, in particular, contributes to failures of metal-ceramic objects due to factors such as compatibility in thermal expansion coefficient, lack of anatomic support, inadequate surface roughness, contamination of the metal, lack of metal oxides on the alloy, and presence of voids in the ceramic [Citation3].
FDP fabrication is complex and it is heavily driven by technicians/operator related factors, and hence usually yields low production in numbers. Typically, the fabrication method for framework metal comprises casting and milling technologies that primarily employ noble or base alloys, including titanium (Ti) [Citation6]. Today, the increased implementation of computerization and automation in technologies favored advancement in technologies such as rapid prototyping (RP) or rapid manufacturing (RM) that ultimately allowed for mass-production of custom-designed products in one single production step. The dental industry has benefited substantially from this technology, especially in FDP fabrication [Citation7–11]. The additive manufacturing (AM) technologies allow for mass production of customized dental restorations with superior quality, avoid outsourcing of labor-intensive and operator-dependent procedures, decrease manufacturing costs, waiting time for the patient, and reduce the risk for human error during manufacturing [Citation7,Citation8,Citation11,Citation12].
The current advancement in AM technologies enabled the production of custom designed dental objects that match [Citation13] or even exceed [Citation14] the quality of traditionally produced objects. Nevertheless, these technologies differ in mechanisms and processing routes of different alloys in the fabrication of dental implants, including FDPs [Citation15]. These differences influence surface characteristics due to layer thickness and object positioning, and thus could eventually affect the ceramic adhesion to metals. Since the operator factor cannot be completely eliminated during manufacturing metal-ceramic FDPs, at least the metal framework fabrication could be more standardized using additive or 3 D printing technologies.
The objective of this review was to collect information on the available AM technologies that are used for the fabrication of single crowns or FDPs with a focus on their working mechanisms, alloy types and chemistry, surface characteristics, and interaction between the framework and the veneering ceramics.
Materials and methods
Search strategy
An electronic search at MEDLINE (PubMed-NCBI) (http://www.ncbi.nlm.nih.gov/pubmed/), Embase, Scopus databases from 01 January 1996 to 30 June 2020 was conducted for articles in English. Following MeSH terms, search terms and their combinations were used for this search: ‘in vitro’, ‘crowns’, ‘denture, partial, fixed’, ‘dentistry’, ‘fixed dental prosthesis’, ‘FDP’, ‘bridges’, ‘additive manufacturing’, ‘alloys’, ‘surface roughness’, ‘adhesion’. A further manual search covering the period from 01 January 1996 up to and including 30 June 2020 was performed on the following journals: Journal of Dental Research, Dental Materials, International Journal of Prosthodontics, Journal of Prosthetic Dentistry, Journal of Prosthodontics, European Journal of Prosthetic and Restorative Dentistry, Journal of Engineering Manufacture, Lasers in Engineering, Additive Manufacturing, Journal of Manufacturing Processes, Expert Review of Medical Devices, Journal of Materials Science: Materials in Medicine, Critical Reviews in Oral Biology and Medicine, Metals-Basel, International Journal of Oral Care and Research, International Journal of Computerized Dentistry, Nigerian Journal of Clinical Practice, Dental and Medical Problems, BioMed Research International, Journal of the American Dental Association and Journal of Dentistry. In addition, hand searches were performed on bibliographies of the selected original, review articles and narrative reviews to find out whether the search process has missed any relevant articles. Further information was obtained from dental laboratory and technology sources, publications of research institutions, conference abstracts, scientific reports, handbooks, product information, manufacturers’ instructions and internet web sites of the manufacturers.
Inclusion/exclusion criteria
Articles in English reporting on working mechanisms of additive manufacturing technologies for dental alloys, alloy types, surface characteristics studies on roughness measurements and adhesion of veneering ceramics to alloys were included. Articles were not included if results were not presented in micron or MPa.
Selection of studies and data extraction
The search process was conducted by two independent reviewers (H.H. and M.Ö.). Data collection sheets were created in Excel. Disagreement regarding data extraction was resolved by discussion and a consensus was reached. The variables that could not be extracted or calculated were scored as ‘not reported’.
Results
The Kappa score for agreement between the reviewers after screening the abstracts was 0.80. The selection process resulted in the final sample of 134 sources, of which 91 journal articles were found relevant including review articles reporting on working mechanisms of additive manufacturing technologies for dental alloys, 16 articles on alloy types, 1 on roughness measurements and 9 on adhesion of veneering ceramics to alloys. Additional information was collected from 5 books along with websites of the manufacturers (). The summary of the findings was as follows.
Table 1. Overview of composition and physical data of CoCr powers used for dental applications as provided by their corresponding manufacturers.
Working mechanisms and principles of AM technologies
Currently available AM technologies for processing dental alloys for FDP frameworks are primarily based on selective laser sintering (SLS), laser beam melting (LBM), selective laser melting (SLM), direct metal laser sintering (DMLS), LBM and electron beam melting (EBM), direct metal deposition (DMD) or laser engineered net shaping (LENS) technologies.
Laser beam melting
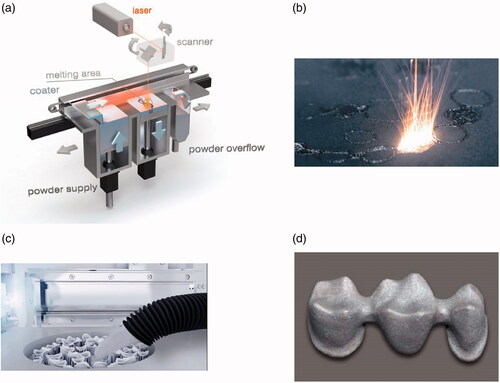
Laser beam melting (LBM) and related methods for AM of metal products, such as SLS, share the same principle in that they are all capable of creating an object with a large degree of geometrical freedom [Citation16–20]. First, a roller or a blade applies a 20 µm thin layer of powdered metal or metal alloy as starting material onto a working platform. A computer-aided design (CAD) software guides a high power laser beam, such as a CO2-laser [Citation21], according to the provided 3 D information [Citation22–24]. The laser operates under a nitrogen or argon atmosphere in order to prevent oxidation of the powdered starting material, scans and directs high-energy beams on defined coordinates in the powder. This energy transfer selectively heats the powder and increases the diffusion of the atoms or molecules, depending on the starting material in the particles [Citation25–27]. The atoms are able to cross the particle boundaries, resulting in fusing or sintering of the targeted particles. After completing this scanning step, the working platform is lowered, a new layer of powder is applied on top of the previous one, and the process is repeated until the final object is completed [Citation22–24]. Hence, the production time depends primarily on the size, and more specifically on the height of the desired object, and not necessarily on the number of objects [Citation7,Citation12]. An overview of the operating principle and the different steps of the production process is presented in .
Figure 1. Images of (a) operating principle of the SLS process (Image courtesy of Concept Laser GmbH). (b) Laser beam melting of metal powder in powder bed fusion), (c) cleaning remaining powder, (d) 3-unit framework of fixed dental prosthesis. Images with courtesy of EOS GmbH, Munich, Germany.
In general, there are two different approaches to obtain the required 3 D information for SLS or any other AM technology. On the one hand, through forward engineering, the surface or the volume is created using CAD [Citation28], and on the other hand, data is obtained by intraoral scanning through reverse engineering. Dental applications usually employ both approaches [Citation28]. The 3 D surface model is then converted into a stereolithography file format (STL) and subsequently processed into a layer representation of the surface geometry [Citation9,Citation29,Citation30]. This information guides the laser through the assembly process. This digital workflow replaces conventional manufacturing route for casting frameworks but requires interdisciplinary effort between the dental technician, prosthodontist and the patient [Citation31].
One very important manufacturing step in SLS technologies is the annealing process, which is the heating of the metal object under argon atmosphere above the critical temperature. After maintaining a stable temperature, the object is allowed to cool down [Citation32,Citation33]. This procedure reduces internal stress, softens and homogenizes the object, and increases its ductility. However, both temperature and atmospheric pressure parameters directly influence the hardness and microstructure of the object and therefore have to be meticulously controlled [Citation32,Citation33]. If executed properly, SLS-manufactured metal frameworks match the required precision for clinical applications, (i.e. approximately 25 µm), and the necessary mechanical strength for FDPs [Citation34]. Theoretically, AM technologies are capable of fabricating very complex and sophisticated oral implants with high precision and reduced labor; however, this is currently not applied in routine. In the near future, this approach will also allow for the production of splinting frameworks for implant-borne FDPs [Citation35].
The term LBM is applied to several different methods, including selective laser sintering (SLS), selective laser melting (SLM), and direct metal laser sintering (DMLS) [Citation7–11,Citation19]. Although there are minor technical differences between these methods, they are often used interchangeably in dentistry. In fact, the laser in SLS does not completely melt the starting material but limits the melting of the particle surface, and produces a final object with certain properties, such as high porosity. Metals, plastics, glass or ceramics are suitable starting materials for SLS. DMLS, on the other hand, is essentially the same as SLS but the starting material is metal [Citation12]. By contrast, SLM is slightly different from both SLS and DMLS as the starting material is not sintered but rather melt, enabling the creation of a very homogeneous product [Citation7,Citation10,Citation36]. For SLM, the starting material should be very pure in order to ensure only one single melting point.
In general, it is difficult to differentiate the described methods since the quantity of transferred laser energy can be modulated allowing for sintering, melting or a mixture of both. Ultimately, the scanning speed and the energy output of the laser control are essential for different applications [Citation21]. For instance, intensity modulation of the laser is used during the manufacturing of FDP frameworks in order to transmit low energy for creating internal structures [Citation36,Citation37]. The downside of this approach is a reduced density, and hence a lower mechanical stability of the final framework. The detailed effects of laser modulation and its effect on different starting materials is a very complex and poorly understood phenomenon.
Electron beam melting
The basic principles of LBM apply to EBM as well and have been summarized elsewhere [Citation16–20]. In addition, the interested reader is referred to this recent and comprehensive review on EBM [Citation38]. In contrast to LBM, EBM employs an electron beam instead of a laser beam. The high energy density of the electron beam completely melts the starting material at high temperatures and allows for creating products with very favorable microstructural features superior to LBM technology. The technical demands for EBM are also higher than for LBM because electron beams require vacuum atmosphere. This also makes EBM particularly suitable for processing materials prone to oxidation such as titanium. Nevertheless, the complexity of the processing parameters for EBM limits its application to only a few starting materials. Furthermore, the high energy density of the electron beam excludes the use of alloys containing volatile components. Yet, EBM can process brittle materials that are not suitable for LBM. Brittle materials exhibit challenging thermal expansion and contraction properties, which cause significant internal stress upon cooling, but the very high temperatures of around 870 K during EBM prevent build-up of internal stress. One side effect of the high-energy electron beam is that the production platform typically becomes very hot after completion, and therefore the manufacturing process demands implementation of long cooling durations. Moreover, several cycles of heating and melting may be used per layer, which increases production time and costs.
Direct metal deposition
In DMD or laser engineered net shaping (LENS) technology, a dispenser containing the starting material is used to feed a constant flow of material into the focused laser beam in order to produce fully dense parts at a high deposition rate. Similar to LBM, the laser in DMD requires securely controlled environmental conditions such as argon atmosphere. The laser fully melts the powdered starting material and generates a small molten pool of raw material. DMD permits the use of several dispensers with different starting materials at the same time, and thus creating products with chemical composition gradients. DMD is more complex than LBM or EBM as it comprises processing parameters for both powder flow and molten metal flow. The powder flow rate and fluid flow parameters affect the produced object along with printing process parameters (e.g. laser power and scanning speed) [Citation17]. The DMD process requires maintenance of a narrow energy balance that constantly changes depending on geometry of the substrate, surrounding temperature or other parameters. Thus, DMD is very sensitive to environmental conditions, and the produced layer thickness varies between 0.3 and 1.0 mm, posing a serious challenge for the fabrication and precision of dental applications. Current technological advances address these issues, and e present a path for DMD into the dental industry [Citation39]. All details on DMD have been extensively described earlier [Citation16–19,Citation40], and the interested reader is recommended to consult a recent and comprehensive review [Citation41].
Metals used in AM technologies
FDPs consists of a metal framework and typically a feldspathic ceramic veneering material. Initially, noble metals were more commonly used for the fabrication of metal framework owing to their excellent mechanical properties, biocompatibility and precision [Citation42]. However, due to the relative high costs, metal alloys with lower gold content gradually replaced the noble metals. Increasing financial pressure eventually led to the substitution of gold-containing alloys with alternative base metal alloys on a large scale. Thus, noble metals such as gold and platinum contribute to only a small fraction of today’s market of metal-ceramic FDP frameworks [Citation43]. Palladium-based alloys were one of the first base metal alloys used for dental restorations and have demonstrated excellent properties [Citation44]. However, volatile prices of palladium as well as public controversies about putative biological problems pushed the biomedical market away from palladium-based alloys towards other more cost-effective alloys [Citation44]. Despite public controversies, the literature suggests that the biocompatibility of palladium-based alloys is excellent although corrosion of some alloy variants might be associated with palladium allergy and insensitivity [Citation45,Citation46].
Today, Nickel-Chromium (NiCr) alloys are the most commonly used base metal alloys [Citation32,Citation43]. However, in Central Europa and Scandinavia Cobalt-Chromium (Co-Cr) alloys are the primary choice. The concerns over Ni as risk factor for allergic reactions for both patients and dental professionals promoted the use of Co-Cr as framework metal. In addition, Co-Cr alloys have been commonly used in model casting for many decades, and their mechanical properties are well recognized. Co-based dental alloys do not comprise noble metals but usually include about a quarter of chromium (Cr), 5% Molybdenum (Mo) and 5% Tungsten (W) [Citation47,Citation48]. The specific composition of the individual components defines the properties of the Co-containing alloys. In general, Co-based dental alloys show similar physiochemical properties as noble metals such as high resistance towards corrosion. This resistance is due to the strong tendency of Cr and Co to react with oxygen and subsequently form a stable oxide layer that grants protection from aqueous solutions [Citation47,Citation49,Citation50].
Titanium is another metal often used in dentistry, and undergoes similar rapid oxidation, forming a protective titanium oxide layer [Citation51,Citation52]. Furthermore, Titanium displays a variety of favorable features, such as high strength, good corrosion resistance and excellent biocompatibility [Citation53,Citation54]. The shortcoming of Titanium is its low density that affects its stability, resulting in porosity formation and shrinkage during casting. Titanium is still widely fabricated by lost-wax casting, but the number of Titanium objects manufactured by DMLS is rising.
Current additive manufacturing uses mainly Co-Cr and Titanium alloys in SLS for dental objects. From a technical perspective, there is no substantial difference between Co-Cr alloy particles and Titanium particles. Both Titanium powder and Co-Cr alloy powder react quickly with oxygen, and therefore all steps from production to storage and manufacturing have to be carefully regulated and monitored [Citation29,Citation40]. Nonetheless, Titanium powder possesses a substantially higher affinity to oxygen and it is highly explosive. Consequently, additional safety precautions are necessary, which lead to higher production costs of Titanium powder [Citation29,Citation40]. During SLS, laser scanning is performed under nitrogen or argon atmosphere to avoid oxidation and to prevent metal oxide inclusion and possible instabilities due to welding beads.
The quality of the manufactured product strongly depends on the quality of the starting material, which currently is poorly regulated and standardized [Citation32]. For dental applications, the particle size of the powdered Co-Cr alloy lies in the lower µm range [Citation29]. The metal powder is produced by atomizing a flow of metal melt under a high-pressure gas stream of nitrogen or argon. This so-called gas atomization creates homogeneous drops with a diameter of less than 50 µm. These particle drops, termed mini ingots, are sieved multiple times into different size fraction that are then used for various applications, depending on the average particle size in these fractions. Such applications range from batteries and paints to tools and rocket fuels and many more [Citation29].
It should be noted that SLS allows for the use of a wide range of alternative materials that display favorable properties for the manufacturing process (e.g. thermoplastic polymers and ceramics) [Citation55]. Nevertheless, Co-Cr is currently the most commonly used alloy type for FDP frameworks that is processed using AM technologies. An overview of commonly used Co-Cr alloys, their composition and mechanical properties are listed .
Surface microstructure and roughness of AM alloys
Active modulation of parameters like scanning speed and energy output of the laser influences physical properties such as thermal stresses and the formation of artifacts [Citation56]. One notable example of such artifact is the so-called balling phenomenon that often occurs in conjunction with SLS and causes distortions in the manufactured object [Citation57]. Examples of typical balling phenomenon are presented in . A highly important physical property of FDP frameworks – and implants in particular – is the surface topography. The surface microstructure substantially contributes to quality of dental objects because it directly affects osseointegration (i.e. the stable anchoring of the dental implant in the living bone) [Citation58]. In principle, microstructures could increase mechanical interlocking, and thereby escalate the bond strength between metal framework and ceramic veneer as well as between metal, abutment tooth and luting cement. It has been previously noted that extreme peaks and valleys in the surface topography may result in stress zones at the ceramic-alloy interface, yielding to deflection and delamination of the veneering ceramic [Citation59]. For this reason, the interplay between roughness and surface topography, and adhesion of veneering ceramic remains to be elucidated.
Figure 2. Examples of typical balling phenomenons: (a) big-sized balls, 500 μm; (b) small-sized balls, 10 μm. Courtesy of Li et al. [Citation57].
![Figure 2. Examples of typical balling phenomenons: (a) big-sized balls, 500 μm; (b) small-sized balls, 10 μm. Courtesy of Li et al. [Citation57].](/cms/asset/f1f65743-c404-4f20-b5c3-4736f58cd35e/tast_a_1899699_f0002_b.jpg)
In general, the metal framework of SLS-manufactured objects presents a rough surface microstructure compared to conventionally manufactured metal frameworks [Citation34,Citation59]. The surface average roughness (Ra) of an SLS-manufactured object was reported to be 3.2 ± 0.4 µm, whereas casted objects display an Ra of 2.3 ± 0.6 µm [Citation59]. It remains unclear whether these differences are clinically significant; nevertheless, they are also associated with the metal substructure any may be clinically relevant on alloy tissue interactions in implant dentistry or biofilm accumulation on implant structures. In case of Co-Cr alloys, conventional manufacturing procedures create a dispersed, heavier second phase in the matrix [Citation61], whereas SLS-manufactured objects contain certain intermetallic phases [Citation62]. Furthermore, SLS causes chemical modification on the alloy surface, including the formation of a specific oxide layer and distribution of elements in the metal framework that affects the bond strength to the feldspathic ceramic veneer [Citation49,Citation63]. Taken together, AM technologies produce more favorable microstructure in the fabricated material than conventional casting and finishing [Citation34,Citation48,Citation49,Citation64].
Notably, there are also differences in the microstructures between SLS and EBM-produced objects. For instance, EBM induces a diffusion process in the titanium alloy Ti-6, Al-4V that creates the so-called Widmanstätten structure [Citation65], whereas SLM does not induce this diffusion process and yields a martensitic-type structure [Citation66]. An example of Widmanstätten structure is presented in . Both SLM and EBM completely melt the Ti-6Al-4V alloy, which requires a heating temperature of 1650 °C to 1660 °C; however, the cooling rate differs between both methods, ultimately affecting the microstructure of the dental object.
Figure 3. Widmanstätten structure. Courtesy of Safdar et al. [Citation65].
![Figure 3. Widmanstätten structure. Courtesy of Safdar et al. [Citation65].](/cms/asset/8f3044f7-5852-4d5a-8c20-8ca319e9b51d/tast_a_1899699_f0003_b.jpg)
Veneering ceramic-alloy interactions in AM technologies
From the perspective of material science, several factors affect the quality of an FDP. Besides mechanical parameters that determine elasticity or stiffness, the coefficient of thermal expansion (CTE) is the most important parameter [Citation67,Citation68]. Both metal framework and ceramic veneering possess different CTE values, yielding a mismatch of differential thermal contraction and expansion between both materials in the FDP. Hence, compensation of this mismatch is necessary in order to avoid internal stresses that jeopardize structural integrity, eventually leading to micro fractures in the prosthesis. There are two strategies for this, namely, the use of bonders or the use of oxides of ceramic particles [Citation69,Citation70].
Bonders are an interlay of a different material, creating an elastic interface between the metal and the ceramic. For instance, the noble element gold is a well-known bonder since it is very ductile, and can easily create an elastic interface, compensating for CTE mismatches [Citation69]. It is crucial to define the optimal thickness of the gold layer in order to ensure the deflection of mastication forces from the ceramic veneer to the metal framework beneath. However, the use of gold comes with disadvantages, such as the risk of formation of galvanic elements, which could cause or enhance corrosion.
Introduction of additional oxides or ceramic particles alters the chemical composition of the material [Citation70]. Oxides react with the opaque ceramic during the ceramic firing, whereas ceramic particles link mechanically and chemically with the metal framework, allowing for stronger interaction with the opaque during the synthesis of the ceramic veneer. Generally, noble and base metal alloys provide sufficient bond strength with ceramic materials so that bonders are not always necessary [Citation69]. Nonetheless, bonders are recommended for titanium due to its low CTE value, creating substantial CTE value mismatch with commonly used base metal alloys [Citation71]. Titanium alloys are a potential exception for this recommendation; however, they are rarely used and are still under development [Citation72]. There are two types of failure for bonders: the cohesive and the adhesive failure mode. The cohesive failure mode describes structural separation within a single type of molecular structure (i.e. within the bonder), whereas the adhesive failure mode refers to separation at the interface of two different materials (i.e. ceramic from the metal framework or ceramic veneer from the bonder) [Citation73]. The incident of both failure modes is called mixed failure mode. Current studies on bond strength of SLS manufactured FDPs show results comparable to previous adhesion studies on metal ceramic objects [Citation74,Citation75]. Nonetheless, failure types of bonders tend to display adhesive failure modes, indicating the need for further development.
Among AM technologies, SLS displays a seemingly favorable role over conventional manufacturing regarding bond strength. SLS-manufactured metal objects appear to have higher bond strengths, which is highly desirable for FDPs. A growing body of evidence suggests that SLS increases the bond strength at a range of 24 ± 10 MPa to 54 ± 14 MPa, and reduces the occurrence of adhesive failures [Citation32,Citation34,Citation48,Citation49,Citation64,Citation70,Citation71,Citation76]. Currently, there is no sufficient explanation for this observation, and further investigation is required. For example, a correlation between different microstructures of the AM-fabricated alloy surfaces and the veneer-alloy bond strength values could provide some evidence of the underlying mechanism.
Discussion
This review focused on the summary of technical improvements in additive technologies with a particular focus on the production of metallic FDP frameworks in the dental industry. Accordingly, in general, SLS is a highly versatile technology that can employ a large variety of different materials and can create very complex objects with well-defined interior fit. It should be noted that there is no standardized procedure for determining both marginal and internal fit, and hence there are no universal guidelines on acceptable thresholds for clinical applications [Citation14,Citation60]. Nonetheless, dental research deems the marginal gap acceptable if it remains below 100 µm [Citation13,Citation14]. A growing body of evidence implicates that SLS-manufactured objects display an internal fit that fulfils the requirement for dental applications [Citation13,Citation14,Citation60,Citation77,Citation78]. Some research even suggests that AM results in a higher degree of precision and increased fitting accuracy [Citation68]. Moreover, the majority of studies point out that SLS-manufactured dental objects provide better vertical marginal fit parameters than traditional fabrication processes [Citation14,Citation77–82]. These superior properties appear independent of anatomical features since studies on molar and premolar crowns did not find any significant differences in vertical marginal fit.
Current limitations of AM technologies are the lack of standardization or regulation of the production of the starting powder material, which causes heterogeneities [Citation32]. This produces melt pool instabilities, influencing the quality of the dental object. Another limitation concerns logistics and safety. Some metal powders, in particular titanium powder, is highly explosive and demands specialized handling and storage [Citation29,Citation40]. Furthermore, the application of SLS and related AM technologies relies on specific skill sets and education that requires a different training of dental technicians [Citation83]. In addition, AM technology consumes a large amount of energy due to the application of high-energy laser or electron beams, thus exhibits a higher energy-consumption than conventional manufacturing for one dental object [Citation84,Citation85]. However, since SLS can produce several objects at the same time, this should compensate the increased production time or energy per single object [Citation7,Citation12]. Finally, SLS-manufactured dental objects differ from conventionally produced objects by several properties, in particular porosity and surface microstructure [Citation34,Citation59]. This might affect the use and quality for dental applications. All these criteria also apply to EBM except for surface properties [Citation86].
Today, there is an increasing trend for metal-free reconstructions in dentistry, in particular for zirconium-based materials, and recent studies show similar survival for all-ceramic and metal-ceramic FDPs [Citation87–89]. However, all-ceramic materials are slightly more prone to failures, such as fractures or chippings [Citation90]. On the other hand, the advantages of SLS for metals cannot be implemented for ceramics [Citation11]. Technological advancement and the improvement of AM technologies (e.g. EBM and DMD) might overcome this limitation soon [Citation39,Citation91].
The rise of computerization and automation affects the dental industry, providing fast and cost-effective customized mass-production of metal-ceramic FDPs using SLS technologies. SLS is still a very young technology that entered the dental market only several years ago. Many technical and practical questions remain unanswered. Regardless of the advances in technologies and materials, dental professionals should be aware of the possibilities with and limitations of SLS manufactured dental objects. Nevertheless, the focus of this review on the clinical parameters of ceramic-metal adhesion and surface roughness could be rated as acceptable. Yet, the minute differences in the latter may have clinical implications in implant-tissue interactions, which need to be further investigated.
Conclusions
From this review, the following could be concluded:
Current additive manufacturing (AM) technologies for the fabrication of frameworks of single crowns or fixed-dental prosthesis (FDP) process mainly Co-CR or titanium alloys.
Selective laser sintering (SLS) seems more suitable for Co-Cr alloys, whereas electron beam melting (EBM) appears to process Titanium alloys better.
AM technologies generate a rougher surface microstructure in the range of 3 to 4 µm compared to conventional cast objects (2–3 µm) which may be clinically relevant for implant structures but not for other dental applications.
Bond strength between the veneering ceramic and AM fabricated alloys exceed 20 MPa but correlation with metal surface topography and failure types analysis remains to be elucidated.
Clinical relevance
Additive manufacturing technologies can currently process Co-Cr and titanium alloys for the fabrication of FDP frameworks with rougher surface texture than those of cast or milled versions. Bond strength between veneering ceramic and alloys seems comparable to cast versions but adhesive failure types need further elaboration regarding surface chemistry and microstructure.
Acknowledgments
The authors acknowledge EOS GmbH, Munich, Germany, 3D Systems, Rock Hill, South Carolina, USA, Concept Laser, Lichtenfels, Germany, BEGO, Bremen, Germany, SLM Solutions, Lübeck, Germany for providing information on their technologies.
Disclosure statement
The authors have no commercial interest in any of the materials or technologies mentioned in this study.
References
- Zarone F, Russo S, Sorrentino R. From porcelain-fused-to-metal to zirconia: clinical and experimental considerations. Dent Mater. 2011;27(1):83–96.
- Walton TR. The up to 25-year survival and clinical performance of 2,340 high gold-based metal-ceramic single crowns. Int J Prosthodont. 2013;26(2):151–160.
- Özcan M. Fracture reasons in ceramic-fused-to-metal restorations. J Oral Rehabil. 2003;30(3):265–269.
- Coornaert J, Adriaens P, De Boever J. Long-term clinical study of porcelain-fused-to-gold restorations. J Prosthet Dent. 1984;51(3):338–342.
- Özcan M, Niedermeier W. Clinical study on the reasons for and location of failures of metal-ceramic restorations and survival of repairs. Int J Prosthodont. 2002;15:299–302.
- Drago C, Howell K. Concepts for designing and fabricating metal implant frameworks for hybrid implant prostheses. J Prosthodont. 2012;21(5):413–424.
- Beguma Z, Chhedat P. Rapid prototyping--when virtual meets reality. Int J Comput Dent. 2014;17(4):297–306.
- Berman B. 3-D printing: the new industrial revolution. Bus Horiz. 2012;55(2):155–162.
- Dawood A, Marti Marti B, Sauret-Jackson V, et al. 3D printing in dentistry. Br Dent J. 2015;219(11):521–529.
- Kruth JP, Van Den Broucke B, van Vaerenbergh J, et al. Rapid manufacturing of dental prostheses by means of selective laser sintering/melting. Les 11emes Assises europeennes du Prototypage rapide (AFPR) 4–5 October 2005, Paris, France, S4; 2005.
- Sun J, Zhang FQ. The application of rapid prototyping in prosthodontics. J Prosthodont. 2012;21(8):641–644.
- van Noort R. The future of dental devices is digital. Dent Mater. 2012;28(1):3–12.
- Quante K, Ludwig K, Kern M. Marginal and internal fit of metal-ceramic crowns fabricated with a new laser melting technology. Dent Mater. 2008;24(10):1311–1315.
- Örtorp A, Jönsson D, Mouhsen A, et al. The fit of cobalt-chromium three-unit fixed dental prostheses fabricated with four different techniques: a comparative in vitro study. Dent Mater. 2011;27(4):356–363.
- Alharbi N, Wismeijer D, Osman RB. Additive manufacturing techniques in prosthodontics: where do we currently stand? A critical review. Int J Prosthodont. 2017;30(5):474–484.
- Hirt L, Reiser A, Spolenak R, et al. Additive manufacturing of metal structures at the micrometer scale. Adv Mater. 2017;29(17):1604211.
- Trevisan F, Calignano F, Aversa A, et al. Additive manufacturing of titanium alloys in the biomedical field: processes, properties and applications. J Appl Biomater Funct Mater. 2018;16(2):57–67.
- Gokuldoss PK, Kolla S, Eckert J. Additive manufacturing processes: selective laser melting, electron beam melting and binder jetting-selection guidelines. Materials. 2017;10(6):672.
- Herzog D, Seyda V, Wycisk E, et al. Additive manufacturing of metals. Acta Mater. 2016;117:371–392.
- Sing SL, An J, Yeong WY, et al. Laser and electron-beam powder-bed additive manufacturing of metallic implants: a review on processes, materials and designs. J Orthop Res. 2016;34(3):369–385.
- Dikova T, Panova N, Simov M. Application of laser technologies in dental prothetics. Mach Technol Mater. 2011;6:32–35.
- Niemann P. Laser-Sinterverfahren in der CAD/CAM-Technik. Quintessenz Zahntechnik. 2003;29:38–42.
- Rudolph MS. J. Ein CAD/CAM-System mit aufbauender Lasertechnologie. Quintessenz Zahntechnik. 2007;33:582–587.
- Szwedka G, Claisse L. CAD-unterstützte lasergestützte Fertigung von Zahnersatz - Fallbeispiele aus der Kombinationstechnologie. Quintessenz Zahntechnik. 2011;37:374–380.
- Childs THC, Hauser C, Badrossamay M. Selective laser sintering (melting) of stainless and tool steel powders: experiments and modelling. P I Mech Eng B-J Eng. 2005;219(4):339–357.
- Guo LF, Yue TM, Man HC. Melting behaviour of a powder bed under laser irradiation. Laser Eng. 2006;16:215–234.
- Lepski D, Kusch HG, Reitzenstein W. Modelling of diffusion controlled moving boundary processes during the laser remelting of ferritic nodular cast iron – carbon diffusion in laser remelting. Laser Eng. 1997;5:247–274.
- Gischer F, Klare M. Grundlagen von Schichtbauverfahren und deren Auswirkungen auf den Dentalmarkt. Quintessenz Zahntechnik. 2009;35:1128.
- Riquier R. Frästechnik versus Lasersintern. Quintessenz Zahntechnik. 2006;32:534–546.
- Williams RJ, Bibb R, Eggbeer D, et al. Use of CAD/CAM technology to fabricate a removable partial denture framework. J Prosthet Dent. 2006;96(2):96–99.
- Revilla-Leon M, Sanchez-Rubio JL, Besne-Torre A, et al. A report on a diagnostic digital workflow for esthetic dental rehabilitation using additive manufacturing technologies. Int J Esthet Dent. 2018;13:184–196.
- Ayyildiz S, Soylu EH, Ide S, et al. Annealing of Co-Cr dental alloy: effects on nanostructure and Rockwell hardness. J Adv Prosthodont. 2013;5(4):471–478.
- Ayyildiz S. The place of direct metal laser sintering (DMLS) in dentistry and the importance of annealing. Mater Sci Eng C Mater Biol Appl. 2015;52:343.
- Barucca G, Santecchia E, Majni G, et al. Structural characterization of biomedical Co-Cr-Mo components produced by direct metal laser sintering. Mater Sci Eng C Mater Biol Appl. 2015;48:263–269.
- Revilla-Leon M, Sanchez-Rubio JL, Oteo-Calatayud J, et al. Impression technique for a complete-arch prosthesis with multiple implants using additive manufacturing technologies. J Prosthet Dent. 2017;117(6):714–720.
- Strietzel R. Selektives Laserschmelzen für die Verarbeitung dentaler Legierungspulver. Quintessenz Zahntechnik. 2009;35:1112–1125.
- Fischer J, Stawarczyk B, Trottmann A, Hämmerle CHF. Festigkeit lasergesinterter Brückengerüste aus einer CoCr-Legierung. Quintessenz Zahntechnik. 2008;34:140–149.
- Galati M, Iuliano L. A literature review of powder-based electron beam melting focusing on numerical simulations. Addit Manuf. 2018;19:1–20.
- Arias-Gonzáleza F, del Vala J, Comesañab R, et al. Additive manufacturing based on laser cladding of Cp-Ti for dental implants. Lasers in Manufacturing Conference 2015, 2015.
- Schütz M. Rapid manufacturing. Quintessenz Zahntechnik. 2009;35:1174–1178.
- Ahmed N. Direct metal fabrication in rapid prototyping: a review. J Manuf Process. 2019;42:167–191.
- Pini NP, Aguiar FH, Lima DA, et al. Advances in dental veneers: materials, applications, and techniques. Clin Cosmet Investig Dent. 2012;4:9–16.
- Park JK, Lee WS, Kim HY, et al. Accuracy evaluation of metal copings fabricated by computer-aided milling and direct metal laser sintering systems. J Adv Prosthodont. 2015;7(2):122–128.
- Wataha JC, Shor K. Palladium alloys for biomedical devices. Exp Rev Med Dev. 2010;7(4):489–501.
- Berzins DW, Kawashima I, Graves R, et al. Heat treatment effects on electrochemical corrosion parameters of high-Pd alloys. J Mater Sci Mater Med. 2008;19(1):335–341.
- Geurtsen W. Biocompatibility of dental casting alloys. Crit Rev Oral Biol Med. 2002;13(1):71–84.
- Zeng L, Xiang N, Wei B. A comparison of corrosion resistance of cobalt-chromium-molybdenum metal ceramic alloy fabricated with selective laser melting and traditional processing. J Prosthet Dent. 2014;112(5):1217–1224.
- Wu L, Zhu H, Gai X, et al. Evaluation of the mechanical properties and porcelain bond strength of cobalt-chromium dental alloy fabricated by selective laser melting. J Prosthet Dent. 2014;111(1):51–55.
- Henriques B, Soares D, Silva FS. Microstructure, hardness, corrosion resistance and porcelain shear bond strength comparison between cast and hot pressed CoCrMo alloy for metal-ceramic dental restorations. J Mech Behav Biomed Mater. 2012;12:83–92.
- Tuna SH, Özçiçek Pekmez N, Kürkçüoğlu I. Corrosion resistance assessment of Co-Cr alloy frameworks fabricated by CAD/CAM milling, laser sintering, and casting methods. J Prosthet Dent. 2015;114(5):725–734.
- Nakajima H, Okabe T. Titanium in dentistry: development and research in the U.S.A. Dent Mater J. 1996;15(2):77–90.
- ADA Council on Scientific Affairs. Titanium applications in dentistry. J Am Dent Assoc. 2003;134:347–349.
- Kanazawa M, Iwaki M, Minakuchi S, et al. Fabrication of titanium alloy frameworks for complete dentures by selective laser melting. J Prosthet Dent. 2014;112(6):1441–1447.
- Mangano F, Chambrone L, van Noort R, et al. Direct metal laser sintering titanium dental implants: a review of the current literature. Int J Biomater. 2014;2014:461534
- Franco A, Lanzetta M, Romoli L. Experimental analysis of selective laser sintering of polyamide powders: an energy perspective. J Clean Prod. 2010;18(16–17):1722–1730.
- Bae EJ, Kim JH, Kim WC, et al. Bond and fracture strength of metal-ceramic restorations formed by selective laser sintering. J Adv Prosthodont. 2014;6(4):266–271.
- Li R, Liu J, Shi Y, et al. Balling behavior of stainless steel and nickel powder during selective laser melting process. Int J Adv Manuf Technol. 2012;59(9–12):1025–1035.
- Gupta S, Dahiya V, Shukla P. Surface topography of dental implants: a review. J Dent Implant. 2014;4(1):66.
- Castillo-Oyague R, Osorio R, Osorio E, et al. The effect of surface treatments on the microroughness of laser-sintered and vacuum-cast base metal alloys for dental prosthetic frameworks. Microsc Res Tech. 2012;75(9):1206–1212.
- Ucar Y, Akova T, Akyil MS, et al. Internal fit evaluation of crowns prepared using a new dental crown fabrication technique: laser-sintered Co-Cr crowns. J Prosthet Dent. 2009;102(4):253–259.
- Takaichi A, Suyalatu, Nakamoto T, Joko N, et al. Microstructures and mechanical properties of Co-29Cr-6Mo alloy fabricated by selective laser melting process for dental applications. J Mech Behav Biomed Mater. 2013;21:67–76.
- Xin XZ, Chen J, Xiang N, et al. Surface properties and corrosion behavior of Co-Cr alloy fabricated with selective laser melting technique. Cell Biochem Biophys. 2013;67(3):983–990.
- Al Jabbari YS, Koutsoukis T, Barmpagadaki X, et al. Metallurgical and interfacial characterization of PFM Co-Cr dental alloys fabricated via casting, milling or selective laser melting. Dent Mater. 2014;30(4):e79–88.
- Kul E, Aladag LI, Duymus ZY. Comparison of the metal-ceramic bond after recasting and after laser sintering. J Prosthet Dent. 2015;114(1):109–113.
- Safdar A, Wei LY, Snis A, et al. Evaluation of microstructural development in electron beam melted Ti-6Al-4V. Mater Charact. 2012;65:8–15.
- Xu W, Lui EW, Pateras A, et al. In situ tailoring microstructure in additively manufactured Ti-6Al-4V for superior mechanical performance. Acta Mater. 2017;125:390–400.
- Hammad IA, Talic YF. Designs of bond strength tests for metal-ceramic complexes: review of the literature. J Prosthet Dent. 1996;75(6):602–608.
- Hama Suleiman S, Vult von Steyern P. Fracture strength of porcelain fused to metal crowns made of cast, milled or laser-sintered cobalt-chromium. Acta Odontol Scand. 2013;71(5):1280–1289.
- Böhme NS. R. Bonder für edelmetallfreie Legierungen? Quintessenz Zahntechnik. 2009;35:274–283.
- Xin XZ, Chen J, Xiang N, et al. Surface characteristics and corrosion properties of selective laser melted Co-Cr dental alloy after porcelain firing. Dent Mater. 2014;30(3):263–270.
- Iseri U, Ozkurt Z, Kazazoglu E. Shear bond strengths of veneering porcelain to cast, machined and laser-sintered titanium. Dent Mater J. 2011;30(3):274–280.
- Simoes S. Recent progress in the joining of titanium alloys to ceramics. Metals. 2018;8(11):876.
- de Vasconcellos LG, Buso L, Lombardo GH, et al. Opaque layer firing temperature and aging effect on the flexural strength of ceramic fused to cobalt-chromium alloy. J Prosthodont. 2010;19(6):471–477.
- Kumar R, Pathak R, Singh P, et al. Comparison of bond strength and fracture toughness of metal–ceramic restorations fabricated by conventional lost-wax technique and selective laser sintering. Int J Oral Care Res. 2019;7(2):43–45.
- Revilla-Leon M, Meyer MJ, Ozcan M. Metal additive manufacturing technologies: literature review of current status and prosthodontic applications. Int J Comput Dent. 2019;22:55–67.
- Akova T, Ucar Y, Tukay A, et al. Comparison of the bond strength of laser-sintered and cast base metal dental alloys to porcelain. Dent Mater. 2008;24(10):1400–1404.
- Oyague RC, Sanchez-Turrion A, Lopez-Lozano JF, et al. Evaluation of fit of cement-retained implant-supported 3-unit structures fabricated with direct metal laser sintering and vacuum casting techniques. Odontology. 2012;100(2):249–253.
- Oyague RC, Sanchez-Turrion A, Lopez-Lozano JF, et al. Vertical discrepancy and microleakage of laser-sintered and vacuum-cast implant-supported structures luted with different cement types. J Dent. 2012;40:123–130.
- Gunsoy S, Ulusoy M. Evaluation of marginal/internal fit of chrome-cobalt crowns: direct laser metal sintering versus computer-aided design and computer-aided manufacturing. Niger J Clin Pract. 2016;19(5):636–644.
- Nassif QK, Alshaarani FF. Influence of porcelain firing on changes in the marginal fit of metal-ceramic fixed partial dental prostheses fabricated with laser sintering: an in vivo study. Dent Med Probl. 2020;57(2):185–190.
- Pompa G, Di Carlo S, De Angelis F, et al. Comparison of conventional methods and laser-assisted rapid prototyping for manufacturing fixed dental prostheses: an in vitro study. Biomed Res Int. 2015;2015:1–7.
- Presotto AGC, Barao VAR, Bhering CLB, et al. Dimensional precision of implant-supported frameworks fabricated by 3D printing. J Prosthet Dent. 2019;122(1):38–45.
- Despeisse M, Minshall T. Skills and education for additive manufacturing: a review of emerging issues. In: Lödding H, Riedel R; Thoben KD, Von Cieminski G, Kiritsis D, editors. Advances in production management systems. The path to intelligent, collaborative and sustainable manufacturing. Cham: Springer; 2017. p. 289–297.
- Liu ZY, Li C, Fang XY, et al. Energy consumption in additive manufacturing of metal parts. Procedia Manuf. 2018;26:834–845.
- Verhoef LA, Budde BW, Chockalingam C, et al. The effect of additive manufacturing on global energy demand: an assessment using a bottom-up approach. Energ Policy. 2018;112:349–360.
- Revilla-Leon M, Ceballos L, Martinez-Klemm I, et al. Discrepancy of complete-arch titanium frameworks manufactured using selective laser melting and electron beam melting additive manufacturing technologies. J Prosthet Dent. 2018;120(6):942–947.
- Limones A, Molinero-Mourelle P, Azevedo L, et al. Zirconia-ceramic versus metal-ceramic posterior multiunit tooth-supported fixed dental prostheses: a systematic review and meta-analysis of randomized controlled trials. J Am Dent Assoc. 2020;151(4):230–238.e237.
- Sailer I, Balmer M, Husler J, et al. 10-Year randomized trial (RCT) of zirconia-ceramic and metal-ceramic fixed dental prostheses. J Dent. 2018;76:32–39.
- Tanner J, Niemi H, Ojala E, et al. Zirconia single crowns and multiple-unit FDPs-An up to 8 -year retrospective clinical study. J Dent. 2018;79:96–101.
- Heintze SD, Rousson V. Survival of zirconia- and metal-supported fixed dental prostheses: a systematic review. Int J Prosthodont. 2010;23(6):493–502.
- Körner C. Additive manufacturing of metallic components by selective electron beam melting — a review. Int Mater Rev. 2016;61(5):361–377.

