ABSTRACT
Objectives
Fear avoidance is associated with symptom persistence after mild traumatic brain injury (mTBI). In this study, we investigated whether fear avoidance was associated with other outcomes such as return to work-related activity (RTW).
Materials and Methods
We analyzed associations between fear avoidance and RTW 6–9 months after mTBI, in two merged prospective mTBI cohorts. Adult participants aged 16 or over (n=175), presenting to outpatient services in New Zealand within 3 months of their injury, who were engaged in work-related activity at the time of injury, were included. Participants completed the Fear Avoidance Behavior after Traumatic Brain Injury (FAB-TBI) questionnaire at enrollment and 6 months later. Associations between FAB-TBI scores and RTW outcome were analyzed using multivariate approaches.
Results
Overall, 53% of participants had RTW by 6–9 months after mTBI. While early fear avoidance was weakly associated with RTW, persistent high fear avoidance between study assessments or increasing avoidance with time were associated with greater odds of still being off work 6–9 months after injury.
Conclusions
Pervasive and increasing avoidance of symptom triggers after mTBI were associated with lower rates of RTW 6–9 months after mTBI. Further research is needed to better understand transition points along the recovery trajectory where fear avoidance behaviors fade or increase after mTBI.
KEYWORDS:
Introduction
Mild traumatic brain injury (mTBI) is a common injury, representing up to 90% of all traumatic brain injuries, with an estimated incidence exceeding 600 per 100,000 cases a year globally (Citation1). It is common among adults of working age where return to pre-injury levels of work and productivity are important and expected outcomes (Citation2). However, following an mTBI, return to work can be delayed, incomplete, or not achieved (Citation3). Up to a third or more of mTBI cases experience difficulties with employment more than 6 months after injury (Citation4–6). Rates vary across studies, and to some extent in relation to differences in the way return to work outcomes have been conceptualized.
Return to work, employment, and productivity are terms that are often used interchangeably in the mTBI literature. Some studies have defined return to work pragmatically as any return to work after mTBI regardless of type, level, or quality (Citation4). However, return to some or any work-related activity, as opposed to return to usual pre-injury work and productivity levels, are very different outcomes. Others have applied stringent return to work criteria. For example, in a prospective study examining the impacts of post-concussion symptoms and work outcomes in Taiwan (n = 179) (Citation7), outcomes were defined in terms of pre-injury work status versus post-injury status, as well as stability of employment after injury, capturing additional nuances in outcomes. Aside from the economic benefits, paid work improves well-being and life satisfaction and can be protective against loss of self-worth and identity and financial hardship (Citation8,Citation9). For those in paid work before their mTBI, non-return and even partial return to paid work can have negative economic and psychosocial consequences (Citation10). Identifying and addressing barriers to and prognostic factors for, achieving optimal return to work outcomes after mTBI is an important focus of ongoing research.
Recent systematic reviews and population-based studies considering factors associated with mTBI return to work outcomes have inconsistently identified different person factors such as younger or older age (Citation1,Citation11,Citation12); higher or lower levels of education (Citation1,Citation13); injury factors such as radiology outcomes, overall symptom burden, particular acute symptoms such as nausea and vomiting (Citation1,Citation2); occupational factors such as work type, levels of responsibility and autonomy (Citation4); and litigation status (Citation1), as important. Few studies have investigated malleable psychological factors and return to work outcomes in any depth, even though a growing literature exists demonstrating important associations between various psychological factors and other mTBI outcomes (Citation14). These psychological factors include expectations and beliefs (Citation15), anxiety (Citation16), psychological flexibility (Citation17) and fear avoidance (Citation18).
Fear avoidance is a validated risk factor for poor outcomes from a variety of health conditions (Citation19), originally developed to explain the transition from acute to chronic lower back pain (Citation20). It has recently been applied to understanding the development of persistent symptoms after mTBI (Citation18,Citation19,Citation21,Citation22). Theories of fear avoidance have a long history in psychology (Citation23). Fear avoidance involves learning to avoid not only an expected aversive event but also aversive antecedent stimuli. For example, a person may learn to avoid activities and situations that are perceived to provoke or worsen symptoms after mTBI (antecedent stimuli), in an effort to avoid experiencing unpleasant symptoms themselves (the aversive event). Accordingly, the fear avoidance model suggests that when symptoms attributed to mTBI are perceived as dangerous, this contributes to fear-based avoidance of activities identified as symptom triggers (Citation24). While this can be adaptive early after injury (such as within the first 24–48 hours) (Citation18,Citation19), sustained avoidance of symptoms and activities may become maladaptive and lead to increasing symptom persistence through deconditioning and sensitization (Citation18,Citation25,Citation26). Theories of fear avoidance would also predict that as symptoms persist, relationships between fear avoidance beliefs and behaviors, and a widening range of perceived symptom triggers, could strengthen with time through cyclic processes of classical and operant learning principles, as well as generalization (Citation23). For certain individuals, this could result in an increasing range of avoided activities perceived as symptom triggers, resulting in constricting levels of activity and function with time.
A core activity with potential for symptom exacerbation and concomitant fear-based avoidance is return to work. To date, only one study was found examining the role of fear avoidance and return to work (one of a panel of outcomes) after mTBI (Citation18). Participants (n = 87) were recruited from outpatient clinics in Canada and return to work was defined by structured interview as return to usual levels of work (same work activity, hours, responsibilities) versus incomplete or no return, measured at 7 months following mTBI. There were significant associations between early fear avoidance and later symptomatic, functional disability, and psychiatric outcomes, although not return to work outcome. The researchers felt fear avoidance and return to work associations may have been weakened by other factors separate from injury, such as availability of workplace modifications. In addition, patients attending outpatient clinics early after mTBI are typically encouraged to pace return to usual activity (Citation27,Citation28). Slower progress over time may be associated with increasing fear avoidance behaviors through the cyclic learning principles discussed above. Encouragement by health-care providers to pace return to activity such as work and, for example, to avoid symptom triggers at work (Citation29), could unintentionally reinforce fear avoidance for some (Citation30). Given the limited focus to date, further investigation of the associations between fear avoidance and return to work after mTBI is warranted. This may help to identify triggers along recovery timelines where interventions may need to shift focus.
Study objectives
The aim of this study was to examine associations between fear avoidance over time and return to usual levels of work-related activity (RTW) after mTBI in a sample of participants recruited from outpatient concussion services. Those presenting to such tertiary services are likely to be a select sub-population of people with mTBI, with higher levels of psychosocial risk and potential for prolonged recovery (Citation18). Driven by the theoretical understandings of fear avoidance described above, we hypothesized that for this mTBI sub-population i) fear avoidance behaviors early after injury (i.e., <3 months) would not be strongly predictive of RTW outcomes 6–9 months after mTBI. This is because in the sub-acute phase (<3 months), such behaviors can be adaptive and avoidance of symptom triggers is incorporated into early treatment guidelines (Citation29), ii) high fear avoidance at six-nine months after mTBI would be associated with lower rates of RTW, and iii) persistent high fear avoidance from baseline to six-nine months after injury, as well as less reduction in fear avoidance behaviors with time, would be associated with lower rates of RTW six-nine months after injury. We also aimed to investigate what routinely collected demographic and clinical factors might moderate these relationships.
Materials and methods
Design and setting
This is a secondary analysis of data collected from participants attending outpatient concussion services in New Zealand who were enrolled in two separate studies. Both studies used prospective observational methods following participants for up to 9 months after mTBI. The study samples were combined to provide a larger representative sample of people attending concussion services. In study 1, participants were recruited from five outpatient clinics providing rehabilitation services for mTBI across both the North (n = 2) and South Islands (n = 3) of New Zealand between February 2019 and October 2021. The aim of study 1 was to investigate psychological predictors of mTBI outcome. In study 2, participants were recruited from an additional nine outpatient clinics providing rehabilitation services for mTBI in the North Island of New Zealand between March 2020 and September 2020. The aim of study 2 was to examine the role of psychological flexibility as a mediating factor influencing psychological predictors of mTBI outcome. All clinics were funded by New Zealand’s government-funded injury insurance scheme, with the funder also providing standard operating procedures for mTBI management across all participating clinics. Eligibility, recruitment procedures, study assessment timelines, and measures were similar across both studies, enabling merging of datasets for the analyses. Eligible and consenting participants completed questionnaires using REDCap (Citation31), a secure web-based platform either in person or by e-mail link (n = 169), by mailed questionnaires (n = 5), or by telephone (n = 1). Data were collected at enrollment (mean = 6.5 weeks after injury (SD = 2.6, range 2–13 weeks); time 1) and 6 months later (mean = 31.8 weeks post-injury (SD = 3.9, range 23–44 weeks); time 2). Data collection continued during the COVID-19 pandemic and during periods of restriction and lockdown in New Zealand, data were collected remotely.
Ethical approvals for the studies were received from New Zealand’s National Health and Disability Ethics Committee (study 1: ref 18/CEN/79) and the Auckland University of Technology Ethics Committee (study 2: ref 20/32).
Participants
Eligible potential participants were approached by a clinician from the outpatient clinic to invite participation. Eligibility criteria for participants for both studies were as follows: 1) aged 16-years or older (study 1) and 18-years or older (study 2), 2) sustained an mTBI according to World Health Organization Neurotrauma Taskforce criteria (Citation32), 3) were less than 3 months post injury at enrollment, 4) were fluent in English, 5) were engaged in work-related activity at time of injury, and 6) had no prior neurological condition or severe unstable medical condition (e.g., respiratory illness and cancer), including a past history of moderate-to-severe traumatic brain injury. In study 1, n = 85 and in study 2, n = 90 participants’ data were included, resulting in a combined sample of n = 175 participants (see ).
Data collection and measures
i) Demographic and clinical variables
Data for both studies were collected via self-report and included age at injury, gender, ethnicity, highest education level, pre-injury employment status, mental health history, and history of previous mTBI. Clinical variables included mechanism of injury, time from injury to the first study visit (time 1) and time from injury to the second study visit (time 2).
ii) Return to work outcome at time 2, 6–9 months after mTBI
In study 1, participants were asked at their second study visit “Have you returned to your usual levels of work-related activity (including study)?” Response options were coded as “yes I am back at usual levels of work activity; yes, but I am still not back at usual levels; No – I’m not back yet.” In study 2, these RTW outcomes were collected by file review for example, recorded RTW outcomes by occupational and vocational therapists at 6 months post-injury. For the analyses, RTW outcome was dichotomized as i) return to usual levels of work activity, or ii) not back or partially back to usual levels.
iii) Post-concussion symptoms
The Rivermead Post-Concussion Symptom Questionnaire (RPQ) is a 16-item self-report questionnaire that assesses common symptoms following mTBI (Citation33). The RPQ consists of somatic symptoms (headaches, dizziness, nausea and vomiting, noise and light sensitivity, sleep disturbance, and double vision); cognitive symptoms (forgetfulness/poor memory, poor concentration, and taking longer to think); and emotional symptoms (being irritable/easily angered feeling depressed or tearful, feeling frustrated or impatient). Participants rated the presence and problem status of these symptoms on a scale of 0–4 (0 = not experienced at all; 1 = no more of a problem than before injury; 2 = a mild problem; 3 = a moderate problem; 4 = a severe problem). A total score was calculated by summing all 16 items, with scores of 1 recoded to 0 following recommendations of King et al. (Citation33). Rasch analysis has shown that the RPQ demonstrated good internal consistency in a traumatic brain injury sample (person separation index = 0.87) (Citation34).
iv) The Fear Avoidance Behavior after Traumatic Brain Injury Questionnaire (FAB-TBI)
The FAB-TBI includes 16 items sourced from fear avoidance scales originally developed for chronic pain and has been validated for mTBI (Citation35). Items are rated on a 4-point scale ranging from 0 (strongly disagree) to 3 (strongly agree) and summed to produce a total score ranging from 0 to 48, with higher scores meaning greater levels of avoidance. Items refer to the avoidance of activities that might make symptoms worse (e.g., “I should not do my normal work with my present symptoms, “I purposely avoid doing activities that might elicit a headache”). The FAB-TBI has been validated using the Rasch model in an mTBI sample and shown good internal consistency (person separation index = 0.91) (Citation35). In this study, FAB-TBI total ordinal scores were converted to total interval scores using previously developed Rasch conversion tables (Citation35).
v) Depression, Anxiety, and Stress Scale-21 (DASS-21)
The DASS-21 (Citation36) is a 21-item self-reported scale measuring depression, anxiety, and stress with a focus on the previous 7 days. Higher scores on this measure reflect elevated levels of depression, anxiety, and stress symptoms. The DASS-21 has good psychometric properties and is a valid measure of depression, anxiety, and stress symptoms in people with brain injury (Citation37). For this study, total DASS-21 scores were calculated to reflect general psychological distress, with higher scores indicating higher distress (Citation38). The DASS-21 as a unidimensional scale has shown good internal consistency (Cronbach's alpha = 0.86) (Citation38).
Statistical analyses
Data were analyzed using SPSS version 28 (Citation39). Findings are reported following Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines (Citation40). Demographic and clinical characteristics were summarized using descriptive statistics such as means, standard deviation, ranges, and frequencies.
In step 1, demographic and clinical variables were examined by levels of fear avoidance at times 1 and 2. In step 2, we examined associations between time 1 fear avoidance (FAB-TBI interval scores) and dichotomized RTW outcome at time 2, using logistic regression. Odds ratios (OR) and 95% confidence intervals (CIs) were estimated controlling for demographic and clinical covariates identified as potential confounders. Covariates included in the models were selected a priori in line with STROBE recommendations, guided by previous research (Citation41), and included demographics (age, gender, ethnicity, and education), mental health history, prior concussion history, symptom burden, and distress. Continuous measures were rescaled by 10% of the scale maximum before being entered into the regression models to improve interpretability (Citation42). First, the main predictors of interest (fear avoidance at time 1) and covariates were entered separately into individual models to examine unadjusted associations between the various predictors and with RTW outcomes. Adjusted modeling then included all covariates were then entered into a single model to estimate the adjusted association between fear avoidance and RTW while controlling for potential confounders together. Next, we examined associations between fear avoidance (FAB-TBI interval scores) at time 2 and dichotomized RTW outcome at time 2, using independent sample t-tests.
In step 3, we examined patterns of fear avoidance between times 1 and 2 and associations between these patterns and RTW outcomes. Pearson’s correlation was computed between time 1 and time 2 FAB-TBI interval scores. The Bland Altman approach (Citation43) was used to examine the agreement and differences between FAB-TBI at times 1 and 2 in more depth, by using the mean and standard deviations of the differences between FAB-TBI time 1 and 2 scores. The differences between the FAB-TBI interval scores between time 1 and 2 were plotted against the averages of these two measurements. 95% agreement limits were calculated for difference scores with the assumption that 95% of scores should lie within ±2 SD of the mean difference (Citation43). FAB-TBI scores were dichotomized as low versus high at times 1 and 2, based on frequency distributions in the sample and normative data previously published (Citation21), to consider associations between change patterns in FAB-TBI scores over time and RTW outcome. These associations were examined by calculating the proportion of participants who RTW, and comparing group differences using chi-square tests.
Estimates were reported with two-sided 95% CIs. We used list-wise deletion, the default SPSS approach, to manage missing data. There were no missing data points for our primary outcome (RTW at 6–9 months after mTBI). Missing data points for our main predictor (FAB-TBI scores) were low and randomly distributed (Time 1: 7%; Time 2: 4%).
Results
Description of study sample
The sample was on average 36.7 years of age (SD 13.7, range 16–69). There were more women (65%) and a majority reported their ethnicity as New Zealand European (91%). Participants endorsed high levels of education, with 65% describing their highest education level as tertiary or University. The most common injury mechanism was falling (39%), followed by head struck by an object (24%) and transport-related accidents (21%). Over half of the sample reported a mental health history (55%) and 47% endorsed a prior history of mTBI. Demographic and clinical characteristics for studies 1 and 2 are shown in . Demographic and clinical characteristics grouped by patterns of fear avoidance between times 1 and 2 are shown in . Notably, shows there was a relationship between education and fear avoidance patterns, with participants endorsing higher educational attainment being over-represented in low fear avoidance groups. At time 2, 53% of the sample had RTW.
Table 1. Demographic and clinical characteristics of the two study samples (n = 175).
Table 2. Demographic and clinical characteristics of the study sample by patterns of fear avoidance behavior after traumatic brain injury (FAB-TBI) scores at times 1 and 2 (n = 175).
Fear avoidance and return to work or study outcome
i) Time 1 fear avoidance and RTW ()
Table 3. Baseline variables and return to work related activity 6–9 months after mild traumatic brain injury (n = 175).
Unadjusted logistic regression modeling showed fear avoidance at time 1 made a contribution to RTW 6–9 months after mTBI (χ2 (1) = 4.40, p = 0.05). Those with high fear avoidance were less likely to be back at the usual levels of work (OR 0.75, 95% CI 0.56–0.99). Other time 1 variables associated with RTW at time 2 included age, symptom burden, and psychological distress. Those participants who were older and those with higher levels of symptoms and distress at time 1, were less likely to be back at usual levels of work at time 2. Adjustment for demographic and clinical variables shrunk the estimated effect of fear avoidance toward the null (OR 0.82, 95% CI 0.55–1.24), suggesting some of the observed association between fear avoidance at time 1 and RTW is due to confounding with these variables, most likely age. Of the covariates included in the full model, only age (being older) and having a previous mTBI were associated with non-RTW (full model χ2 (12) = 29.08, p < 0.01). This means hypothesis one is only partially supported because while high fear avoidance at time 1 was associated with RTW, the relationship was confounded by demographic factors such as age.
ii) Time 2 fear avoidance and RTW
Fear avoidance at time 2 was associated with being back at usual levels of work (mean difference = 5.56, 95% confidence intervals 3.63, 7.49, p < 0.01), meaning those with higher fear avoidance were less likely to be back at usual levels of work. These results support hypothesis two.
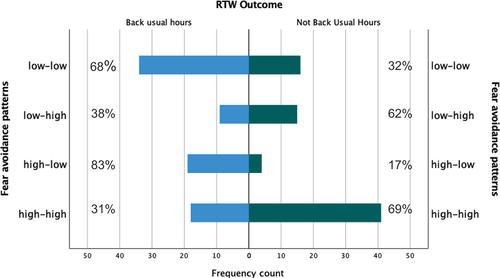
iii) Patterns of fear avoidance over time RTW
The time 1 and 2 FAB-TBI scores were correlated (r = 0.52, p < 0.01). We then examined difference patterns in FAB-TBI interval scores over time before examining these differences in relation to RTW outcomes. Differences in FAB-TBI interval scores between times 1 and 2 (Time 1 – Time 2) for the whole sample were as follows: mean of the difference = 6.93, 95% agreement limits −5.10 to 18.94. shows the differences in FAB-TBI interval scores plotted against the average of time 1 and 2 FAB-TBI interval scores with 95% agreement limits. On average, participants showed an improvement in their FAB-TBI interval score (reduction in fear avoidance), though there was significant variability, with some participants endorsing large reductions in fear avoidance and some, worsening fear avoidance with time. also shows that these patterns were associated with RTW.
Figure 2. Fear avoidance scores between times 1 and 2, showing mean of the difference (middle line) and 95% agreement limits. (A larger positive difference means greater improvement in fear avoidance. FAB-TBI = Fear Avoidance Behavior after Traumatic Brain Injury questionnaire; RTW = return to usual levels of work-related activity 6–9 months after mild traumatic brain injury).
Change patterns between low and high fear avoidance were associated with RTW (χ2(3) = 26.64, p < 0.01). Participants with low levels of fear avoidance at both times 1 and 2 were more likely to be back at usual levels of work at time 2 (n = 34, 68% back at work). Those with high fear avoidance at time 1 but low fear avoidance at time 2 were also more likely to be back at work (n = 19, 83% back at work). On the other hand, participants with high levels of fear avoidance at both times 1 and 2 were less likely to have returned to usual levels of work (n = 18, 31% back at work). Those with low fear avoidance at time 1 but high fear avoidance at time 2, were also less likely to be back at work (n = 9, 38% back at work). These relationships are shown graphically in .
Discussion
Return to work outcomes after mTBI are complex and multifactorial, with interactions between demographic, injury-related, occupational, and psychological factors. In our sample, 53% of participants had returned to usual levels of work-related activity 6 to 9 months after mTBI. This is lower than that reported in other studies where 60–90% of people have returned to work 6 months after mTBI (Citation4,Citation44). Higher return to work rates are typically reported among samples of participants recruited from acute or emergency department settings (Citation6). Accordingly, the lower rate in our study may reflect not only differences in the way return to work was conceptualized but also differences in sample characteristics. Our participants were recruited from outpatient services within 3 months of injury and likely reflect a sub-set of the wider working mTBI population. Those referred to outpatient services are likely to be those with greater risk for slow recovery and symptom persistence, arguably requiring more time to return to usual levels of activity (Citation18). In these individuals, examining psychological risk factors may help to better understand recovery and return to activity outcomes such as work.
The focus of the present study was associations between fear avoidance and mTBI work-related activity outcome. Fear avoidance behavior has been associated with general recovery and symptomatic outcome after mTBI (Citation18,Citation19) and may also be important in understanding return to activities such as work. Consistent with the study hypotheses, fear avoidance early after injury was a weak predictor of RTW 6–9 months after mTBI. However, participants with persistent high levels of fear avoidance from baseline or worsening fear avoidance with time, were less likely to be back at usual levels of work 6–9 months after their injury.
Our findings are supported by fear avoidance theoretical frameworks (Citation20), although they do not necessarily uncover the direction of relationships between fear avoidance and RTW. That is, the point at which avoidance behaviors transitioned to more or less adaptive patterns remains unclear. Participants with low fear avoidance at time 1 or those with high baseline fear avoidance but who were able to transition from high to low avoidance between times 1 and 2 seemed more likely to have returned to usual levels of work by 6–9 months. For these participants, it is not known if lower levels of fear avoidance at time 2 followed or allowed for successful RTW.
Conversely, those with higher baseline fear avoidance unremitting over time, or those who transitioned from low fear avoidance to high fear avoidance, were less likely to be back at work 6–9 months after mTBI. Models of fear avoidance and learning theory (Citation20,Citation23), would suggest that for those with persistent high fear avoidance, associations between feared stimuli (e.g. worsening of symptoms) and certain activities (e.g. cognitive activity or work) may be negatively reinforced and maintained over time because of persistent avoidance of symptom triggers. In those whose fear avoidance increased with time, premature return to activity or work failure experiences could reinforce cause and effect beliefs about dangerousness of engaging in activities such as work, encouraging increased avoidance of symptom triggers rather than development of approach-type behaviors. For this group, avoidance of symptom triggers may generalize and strengthen with time (Citation45), although as noted, determining the point where avoidance shifts to becoming less adaptive remains unclear.
Mechanisms shown to mediate relationships between distress, post-concussion symptoms, and outcome after mTBI, help to understand what mediates transitions between avoidance and approach coping after mTBI (Citation17). One such mechanism is psychological flexibility (Citation46). Psychological flexibility involves adapting to and balancing fluctuating situational demands, allocating mental resources and shifting perspective (Citation47). Although relationships are likely to be complex, one possibility is that coping styles involving high psychological inflexibility may result in more rigid application of advice from mTBI clinicians to rest and pace return to activity to minimize symptom exacerbations. This might inadvertently reinforce and strengthen avoidance.
Considering other variables that might impact these relationships, we also found older age was associated with fear avoidance and lower odds of being back at usual levels of work. This is consistent with many studies that show that older adults can take longer to return to work (Citation11). Another important demographic factor that could mediate relationships between fear avoidance and return to work outcomes is education. Lower levels of education have been found among those with delayed return to work after mTBI (Citation1), and among those with higher levels of fear avoidance after mTBI (Citation18). In our study, there were trends to lower levels of educational attainment among participants with higher levels of fear avoidance at baseline, but these relationships did not appear associated with return to work over time. This may reflect the complexity of relationships between fear avoidance and return to work outcomes, underscoring the importance of exploring other factors such as, for example, psychological flexibility (Citation17).
Clinical implications
Work place accommodations and pacing interventions can be useful early after mTBI for some (Citation48), but potentially unhelpful for those who are highly fear avoidant. For this group, interventions encouraging pacing and symptom avoidance may reinforce dangerousness beliefs. High or increasing levels of fear avoidance behavior should flag to clinicians that alternative treatment approaches are indicated.
Treatment approaches for fear avoidance in other patient populations, such as chronic pain, typically involve adaptation of cognitive behavior therapy (CBT) targeting fear and anxiety (Citation20). Graded exposure-based therapy (GET) that targets fear of activities and situations perceived to exacerbate symptoms, may be ideally suited to addressing avoidant coping after mTBI. These approaches typically include intentional exposure to feared stimuli. Such approaches have been shown to decrease levels of pain-related fear and improve function among people with chronic back pain (Citation49). These approaches have also begun to be applied to mTBI. In a multi-center randomized controlled trial in the Netherlands (Citation50), a brief CBT intervention is being evaluated that targets maladaptive coping styles such as avoidance, in particular to enhance mTBI return to work outcomes. In a feasibility study in Canada, participants (n = 73) were randomized to treatments designed to address fear avoidance or endurance coping styles (Citation27). In this feasibility study, GET demonstrated potential to selectively reduce fear avoidance after mTBI and is a promising option for improving outcomes among those at risk for prolonged mTBI symptoms.
Finally, clinicians could consider treatment approaches that specifically target psychological processes that might mediate relationships between fear avoidance and return to activity after mTBI. For example, targeting psychological inflexibility is a core component of acceptance and commitment therapy (ACT) approaches (Citation51). There is increasing theoretical and empirical support for ACT interventions for people with persistent difficulties following traumatic brain injury (Citation17,Citation52).
Limitations and directions for future research
There are limitations to acknowledge. Merging datasets from two studies while advantageous in providing a larger pool of participants could have introduced bias if there were systematic differences between samples. There is no particular reason to expect this would be the case given recruitment sites across the two studies were comparable in terms of patient referral criteria and characteristics, funding and service specifications. In addition, other than dropout rates, we did not have demographic or clinical data available to check for attrition bias between those enrolled participants who did and did not complete study visits over time. It is possible that those dropping out of study participation were those already back at work, thus our data may overestimate rates of non-return to work after mTBI. Over-estimating poor outcomes is a noted concern associated with attrition bias in mTBI studies (Citation53).
Using a binary endpoint for defining return-to-work outcomes risks missing complexity that may be important in understanding nuances in the relationships between fear avoidance and return to work. Productivity loss was also not captured and is likely important (Citation44). In addition, although rates of RTW outcome did not differ across the two datasets (data not shown), the way return to work outcomes were collected differed across the two studies (self-report in study 1 and by file review in study 2). Future studies could consider standardized measures of return to work-related activity such as the Lam Employment Absence and Productivity Scale (Citation54). More nuanced examinations of variables associated with return work could also include a broader range of occupational factors such as the type of pre-injury work role (e.g. levels of responsibility and autonomy) and stability of pre-injury work (Citation6). Social support has also been shown to be associated with return to work outcomes but was not captured by our study (Citation11). Data collection also occurred during the COVID-19 pandemic with potential for additional unanticipated complications for participants in terms of recovery and return to work-related activities.
Other factors known to be associated with outcomes in mTBI samples but not captured by our study may help to tease out relationships between fear avoidance and return to work outcomes. These factors include expectations and injury beliefs (Citation55,Citation56), psychological flexibility (Citation17), and compensation factors (Citation57), among others. We did not have data available from both datasets for severity of mTBI such as Glasgow Coma Scale scores, duration of post-traumatic amnesia or imaging findings. This means we could not assess whether return to work outcomes could have been influenced by injury severity.
Conclusions
Patterns of fear avoidance were differentially associated with return to usual levels of work-related activity in this study, building on work demonstrating the impact of fear avoidance on mTBI recovery. Participants with persistent high fear avoidance or increasing fear avoidance with time were less likely to be back at work 6–9 months after their injury. The point where avoidance shifts to more or less adaptive coping behaviors remains unclear and could be a focus of future research. Psychological flexibility is a promising mediating mechanism that could help understand these transitions.
Disclosure statement
The authors report no declarations of interest.
Additional information
Funding
References
- Cancelliere C, Kristman V, Cassidy J, Hincapié C, Côté P, Boyle E, Carroll LJ, Stålnacke B-M, Nygren-de Boussard C, Borg J, et al. Systematic review of return to work after mild traumatic brain injury: results of the international collaboration on mild traumatic brain injury prognosis. Arch Phys Med Rehabil. 2014;95(3 Suppl 2):S201–S9. doi:10.1016/j.apmr.2013.10.010.
- Graff H, Deleu N, Christiansen P, Rytter H. Facilitators of and barriers to return to work after mild traumatic brain injury: a thematic analysis. Neuropsychol Rehabil. 2021;31(9):1349–73. doi:10.1080/09602011.2020.1778489.
- Cancelliere C, Donovan J, Stochkendahl M, Biscardi M, Ammendolia C, Myburgh C, Cassidy JD. Factors affecting return to work after injury or illness: best evidence synthesis of systematic reviews. Chiropract Manual Ther. 2016;24(1):32. doi:10.1186/s12998-016-0113-z.
- Bloom B, Thomas S, Ahrensberg J, Weaver R, Fowler A, Bestwick J, Harris T, Pearse R. A systematic review and meta- analysis of return to work after mild traumatic brain injury. Brain Injury. 2018;32(13–14):1623–36. doi:10.1080/02699052.2018.1532111.
- Theadom A, Barker-Collo S, Jones K, Kahan M, Te Ao B, McPherson K, Starkey N, Feigin V, Feigin V, Theadom A, et al. Work limitations 4 years after mild traumatic brain injury: a cohort study. Arch Phys Med Rehabil. 2017;98:1560–66.
- de Koning M, Scheenen M, van der Horn H, Timmerman M, Hageman G, Roks G, Spikman JM, van der Naalt J. Prediction of work resumption and sustainability up to 1 year after mild traumatic brain injury. Neurology. 2017;89:1908–14.
- Chu S, Tsai Y, Xiao S, Huang S, Yang C. Quality of return to work in patients with mild traumatic brain injury: a prospective investigation of associations among post-concussion symptoms, neuropsychological functions, working status and stability. Brain Injury. 2017;31(12):1674–82. doi:10.1080/02699052.2017.1332783.
- Frostad Liaset I, Loras H. Perceived factors in return to work after acquired brain injury: a qualitative meta-synthesis. Scand J Occup Ther. 2016;23(6):446–57. doi:10.3109/11038128.2016.1152294.
- Gamboa AJ, Holland G, Tierney J, Gibson D. American Community Survey: earnings and employment for persons with traumatic brain injury. NeuroRehabilitation. 2006;21(4):327–33. doi:10.3233/NRE-2006-21407.
- Waljas M, Iverson G, Lange R, Liimatainen S, Hartikainen K, Dastidar P, Soimakallio S, Öhman J. Return to work following mild traumatic brain injury. J Head Trauma Rehabil. 2014;29(5):443–50. doi:10.1097/HTR.0000000000000002.
- Kahan M, Jones K, Balalla S, McPherson K, Stedman E, Feigin V. Return to pre-injury work following mild traumatic brain injury. Brain Impairment. 2018;19(2):153–65. doi:10.1017/BrImp.2018.7.
- Waljas M, Iverson G, Lange R, Hakulinen U, Dastidar P, Huhtala H, Liimatainen S, Hartikainen K, Öhman J. A prospective biopsychosocial study of the persistent post-concussion symptoms following mild traumatic brain injury. J Neurotrauma. 2015;32:534–47.
- Stulemeijer M, van der Werf S, Borm G, Voc P. Early prediction of favourable recovery 6 months after mild traumatic brain injury. J Neurol Neurosurg Psychiatry. 2008;79:936–42. doi:10.1136/jnnp.2007.131250.
- Broshek D, De Marco A, Freeman J. A review of post-concussion syndrome and psychological factors associated with concussion. Brain Injury. 2015;29(2):228–37. doi:10.3109/02699052.2014.974674.
- Snell D, Hay-Smith E, Surgenor L, Siegert R. Examination of outcome after mild traumatic brain injury: the contribution of injury beliefs and Leventhal’s common sense model. Neuropsychol Rehabil. 2013;23(3):333–62. doi:10.1080/09658211.2012.758419.
- Mallya S, Sutherland J, Pongracic S, Mainland B, Ornstein T. The manifestation of anxiety disorders after traumatic brain injury: a review. J Neurotrauma. 2015;32:411–21. doi:10.1089/neu.2014.3504.
- Faulkner J, Snell D, Theadom A, Mahon S, Barker-Collo S. The role of psychological flexibility in recovery following mild traumatic brain injury. Rehabil Psychol. 2021;66(4):479–90. doi:10.1037/rep0000406.
- Silverberg N, Panenka W, Iverson G. Fear avoidance and clinical outcomes from mild traumatic brain injury. J Neurotrauma. 2018;35:1864–73. doi:10.1089/neu.2018.5662.
- Wijenberg M, Stapert S, Verbunt J, Ponsford J, Van Heugten C. Does the fear avoidance model explain persistent symptoms after traumatic brain injury? Brain Injury. 2017;31(12):1597–604. doi:10.1080/02699052.2017.1366551.
- Zale E, Ditre J. Pain-related fear, disability, and the fear avoidance model of chronic pain. Curr Opin Psychol. 2015;1(5):24–30. doi:10.1016/j.copsyc.2015.03.014.
- Cairncross M, Debert C, Hunt C, Bayley M, Comper P, Chandra T, Silverberg ND. Normative data for the fear avoidance behavior after traumatic brain injury questionnaire in a clinical sample of adults with mild TBI. J Head Trauma Rehabil. 2021;36(5):E355–E62. doi:10.1097/HTR.0000000000000669.
- Cassetta B, Cairncross M, Brasher P, Panenka W, Silverberg N. Avoidance and endurance coping after mild traumatic brain injury are associated with disability outcomes. Rehabil Psychol. 2021;66(2):160–69. doi:10.1037/rep0000372.
- Krypotos A-M, Effting M, Kindt M, Beckers T. Avoidance learning: a review of theoretical models and recent developments. Front Behav Neurosci. 2015;9(189). doi:10.3389/fnbeh.2015.00189.
- Leeuw M, Goossens ME, Linton SJ, Crombez G, Boersma K, Vlaeyen JW. The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med. 2007;30(1):77–94. doi:10.1007/s10865-006-9085-0.
- Silverberg N, Iverson G, Panenka W. Cogniphobia in mild traumatic brain injury. J Neurotrauma. 2017;34(13):2141–46. doi:10.1089/neu.2016.4719.
- Suhr J, Spickard B. Pain-related fear is associated with cognitive task avoidance: exploration of the cogniphobia construct in a recurrent headache sample. Clin Neuropsychol. 2012;26(7):1128–41. doi:10.1080/13854046.2012.713121.
- Silverberg N, Cairncross M, Brasher P, Vranceanu A, Snell D, Yeates K. Feasibility of concussion rehabilitation approaches tailored to psychological coping styles: a randomized controlled trial. Arch Phys Med Rehabil. 2021;28. doi:10.1016/j.apmr.2021.12.005.
- Silverberg N, Iaccarino M, Panenka W, Iverson G, McCulloch K, Dams-O’Connor K, Reed N, McCrea M, Cogan AM, Park Graf MJ, et al. Management of concussion and mild traumatic brain injury: a synthesis of practice guidelines. Arch Phys Med Rehabil. 2020;101(2):382–93. doi:10.1016/j.apmr.2019.10.179.
- Ontario Neurotrauma Foundation. Guideline for concussion/mild traumatic brain injury and prolonged symptoms: 3rd Edition (for Adults 18+ years of age). Ontario, Canada: Ontario Neurotrauma Foundation,; 2018.
- Silverberg N, Otamendi T. Advice to rest for more than 2 days after mild traumatic brain injury is associated with delayed return to productivity: a case-control study. Front Neurol. 2019;10:362. doi:10.3389/fneur.2019.00362.
- Harris P, Taylor R, Thielke R, Payne J, Gonzalez N, Conde J. Research electronic data capture (REDCap) - a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. doi:10.1016/j.jbi.2008.08.010.
- Holm L, Cassidy J, Carroll L, Borg J. Summary of the WHO collaborating centre for neurotrauma task force on mild traumatic brain injury. J Rehabil Med. 2005;37(3):137–41. doi:10.1080/16501970510027321.
- King N, Crawford S, Wenden F, Moss N, Wade D. The rivermead post concussion symptoms questionnaire: a measure of symptoms commonly experienced after head injury and its reliability. J Neurol. 1995;242:587–92. doi:10.1007/BF00868811.
- Balalla S, Krägeloh C, Medvedev O, Siegert R. Is the rivermead post-concussion symptoms questionnaire a reliable and valid measure to assess long-term symptoms in traumatic brain injury and orthopedic injury patients? A novel investigation using rasch analysis. Neurotrauma Rep. 2020;1(1):63–72. doi:10.1089/neur.2020.0017.
- Snell D, Siegert R, Debert C, Cairncross M, Silverberg N. Evaluation of the fear avoidance behavior after traumatic brain injury questionnaire. J Neurotrauma. 2020;37(13):1566–73. doi:10.1089/neu.2019.6729.
- Lovibond S, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995;33(3):335–43. doi:10.1016/0005-7967(94)00075-U.
- Ownsworth T, Little T, Turner B, Hawkes A, Shum D. Assessing emotional status following acquired brain injury: the clinical potential of the depression, anxiety and stress scales. Brain Injury. 2008;22(11):858–69. doi:10.1080/02699050802446697.
- Zanon C, Brenner R, Baptista M, Vogel D, Rubin M, Al-Darmaki F, Gonçalves M, Heath PJ, Liao H-Y, Mackenzie CS, et al. Examining the dimensionality, reliability, and invariance of the depression, anxiety, and stress Scale-21 (DASS-21) across eight countries. Assessment. 2021;28(6):1531–44. doi:10.1177/1073191119887449.
- IBM Corp. IBM SPSS statistics for MacIntosh. VA, NY: IBM Corp; 2020.
- Vandenbroucke J, von Elm E, Altman D, Gøtzsche P, Mulrow C, Pocock S, Poole C, Schlesselman JJ, Egger M. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLoS Med. 2007;4(10):1628–54. doi:10.1371/journal.pmed.0040297.
- Silverberg N, Gardner A, Brubacher J, Panenka W, Li Jun J, Iverson G. Systematic review of multivariable prognostic models for mild traumatic brain injury. J Neurotrauma. 2015;32(8):517–26. doi:10.1089/neu.2014.3600.
- Geman A. Scaling regression inputs by dividing by two standard deviations. Stat Med. 2008;27:2865–73. doi:10.1002/sim.3107.
- Giavarina D. Understanding Bland Altman Analysis. Biochemia Medica. 2015;25(2):141–51. doi:10.11613/BM.2015.015.
- Silverberg N, Panenka W, Iverson G. Work productivity loss after mild traumatic brain injury. Arch Phys Med Rehabil. 2018;99:250–56. doi:10.1016/j.apmr.2017.07.006.
- Hofmann S. Cognitive processes during fear acquisition and extinction in animals and humans: implications for exposure therapy of anxiety disorders. Clin Psychol Rev. 2008;28(2):199–210. doi:10.1016/j.cpr.2007.04.009.
- Whiting D, Deane F, Simpson G, McLeod H, Ciarrochi J. Cognitive and psychological flexibility after a traumatic brain injury and the implications for treatment in acceptance-based therapies: a conceptual review. Neuropsychol Rehabil. 2017;27(2):263–99. doi:10.1080/09602011.2015.1062115.
- Kashdan T, Rottenberg J. Psychological flexibility as a fundamental aspect of health. Clin Psychol Rev. 2010;30(7):865–78. doi:10.1016/j.cpr.2010.03.001.
- Gourdeau J, Fingold A, Colantonio A, Mansfield E, Stergiou-Kita M. Workplace accommodations following work-related traumatic brain injury: what works? Disabil Rehabil. 2020;42(4):552–61. doi:10.1080/09638288.2018.1503733.
- Trost Z, Parsons T. Beyond distraction: virtual reality graded exposure therapy as treatment for pain-related fear and disability in chronic pain. J Appl Biobehav Res. 2014;19:106–26. doi:10.1111/jabr.12021.
- Scheenen M, Visser-Keizer A, van der Naalt J, Spikman J. Description of an early cognitive behavioral intervention (UPFRONT-intervention) following mild traumatic brain injury to prevent persistent complaints and facilitate return to work. Clin Rehabil. 2017;31(8):1019–29. doi:10.1177/0269215516687101.
- Hayes S, Strosahl K, Wilson K. Acceptance and commitment therapy: the process and practice of mindful change (2nd Edition). 2nd ed. New York, NY: The Guilford Press; 2012.
- Whiting D, Deane F, McLeod H, Ciarrochi J, Simpson G. Can acceptance and commitment therapy facilitate psychological adjustment after a severe traumatic brain injury? A pilot randomized controlled trial. Neuropsychol Rehabil. 2020;30(7):1348–71. doi:10.1080/09602011.2019.1583582.
- Cancelliere C, Verville L, Stubbs J, Yu H, Hincapié C, Cassidy J. Post-concussion symptoms and disability in adults with mild traumatic brain injury: a systematic review and meta-analysis. J Neurotrauma. 2022. doi:10.1089/neu.2022.0185.
- Lam R, Michalak E, Yatham L. A new clinical rating scale for work absence and productivity: validation in patients with major depressive disorder. BMC Psychiatry. 2009;9:78–85. doi:10.1186/1471-244X-9-78.
- Snell D, Surgenor L, Hay-Smith E, Williman J, Siegert R. The contribution of psychological factors to recovery after mild traumatic brain injury: is cluster analysis a useful approach? Brain Injury. 2015;29(3):291–99. doi:10.3109/02699052.2014.976594.
- Whittaker R, Kemp S, House A. Illness perceptions in mild head injury. J Neurol Neurosurg Psychiatry. 2007;78(6):644–46. doi:10.1136/jnnp.2006.101105.
- Mansfield E, Stergiou-Kita M, Cassidy J, Bayley M, Mantis S, Kristman V, Kirsh B, Gomez M, Jeschke MG, Vartanian O, et al. Return-to- work challenges following a work-related mild TBI: the injured worker perspective. Brain Injury. 2015;29:1362–69.